September 7, 2024
Management Of Urinary System Incontinence In Postmenopausal Ladies: An Emas Medical Guide
Menopause And Urinary Incontinence Throughout a female's life, from adolescence to menopause, the delicate balance of hormones manages a symphony of modifications that can influence urinary continence and pelvic flooring strength. Occasionally, there are adjustments to your daily life that can actually help your incontinence. These modifications frequently include exercises you can do to reinforce your pelvic flooring muscular tissues, adjustments to your normal practices and an improved diet regimen. Some people notice enhancements by making these modifications in your home and do not need extra treatment. By integrating INNOVO right into their treatment plan, women can support their urinary system wellness and restore confidence in their day-to-days live. Kegel exercises are a basic way to build strength in your pelvic flooring muscles. These workouts are done by lifting, holding and then unwinding your pelvic flooring muscles. You can find these muscle mass by quiting the flow of urine mid-stream while you're peing. Only do this until you discover how to locate the muscles-- quiting the circulation of pee mid-stream isn't healthy over a long period of time.Comprehending The Web Link In Between Low Estrogen Degrees And Urinary Incontinence
Because of the position and feature of steroids in the urinary system, the use of replaced hormone therapy in menopause has long drawn in the focus of scientists and providers of healthcare in this area. In females without urethral hypermobility, the urethra is maintained throughout stress and anxiety by 3 related systems. One device is reflex, or volunteer, closure of the pelvic floor. Contraction of the levator ani facility elevates the proximal urethra and bladder neck, tightens intact connective cells sustains, and raises the perineal body, which might work as a urethral backstop. If you're experiencing incontinence throughout your period or your cycle, it can transform your quality of life.Neurologic Causes
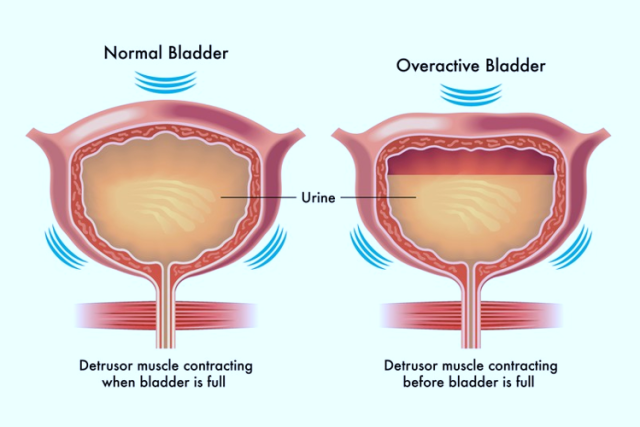
It can likewise compromise your pelvic floor muscular tissues, making it more difficult to hold in pee. Nonneurogenic urinary incontinence may be brought on by anatomic or practical disorders (e.g., ectopic ureters) influencing the storage stage of micturition. Hormone-responsive urinary incontinence is likewise a typical type of nonneurogenic urinary incontinence. In these people (generally canines), the detrusor response is regular; typical peeing actions, in addition to urine dribbling, happens.Treatment For Low Estrogen Bladder Signs
It additionally assists maintain your bladder and urethra healthy and working appropriately. They may no more be able to regulate your bladder as they did before. As your estrogen degrees continue to go down throughout and after menopause, your UI signs might become worse. Estrogens, normally in the kind of diethylstilbestrol, are carried out to made sterile females.- Individuals with urinary incontinence often live with this condition for 6-9 years before seeking clinical therapy.
- Psychophysiological feedback is collaborated with pelvic flooring (Kegel) exercises.
- The hollow participant by supporting muscular tissues is placed in an ideal place and if for any type of factor the supporting muscle mass shed the capability, bladder displaced from its location and creates issues for the person.
- Cauda equina disorder can develop in clients with a big centrally protruding disk.
What hormonal agent keeps you from peeing?
Social Links