September 12, 2024
The Impacts Of Hormones On Urinary System Incontinence In Postmenopausal Women


Urinary System Incontinence In Women If left unattended, these skin disorders might result in press sores and abscess, potentially causing additional infections. The accurate frequency of urinary incontinence is challenging to approximate. Part of the trouble has been in defining the degree, amount, and frequency of urine loss essential to qualify as pathologic, with varying meanings amongst research studies.
Much More On Urinary Incontinence
How to treat hormone imbalances?
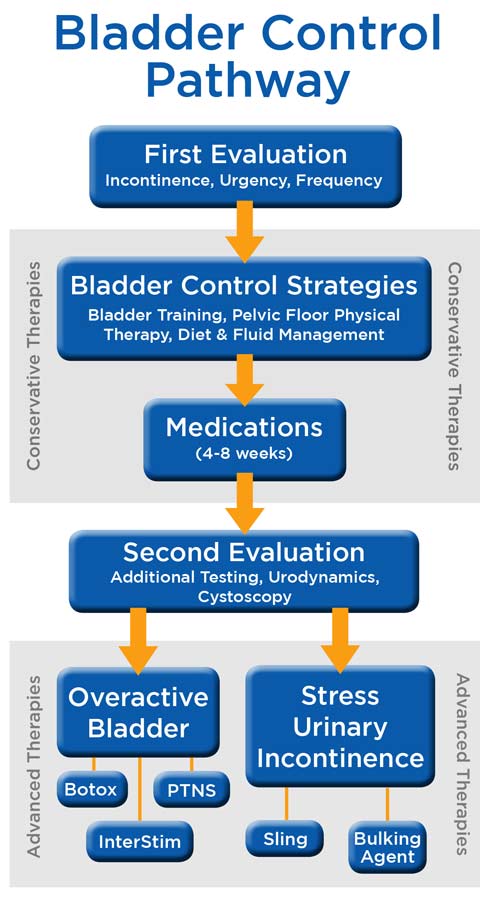
There are many different factors that your healthcare provider will certainly take into consideration when developing a treatment prepare for your urinary incontinence. The sort of incontinence
Learn more and the ways it affects your life are both big factors to consider. Your supplier will additionally speak with you about the kind of therapy you are most comfortable with.
Low Estrogen Levels
Low estrogen can trigger bladder signs and symptoms by thinning the cells that lines the vaginal area. This decreases the flexibility and stamina of the vagina and bordering muscles, reducing muscle assistance for the bladder and associated frameworks, such as the urethra. However, not all people with reduced estrogen establish bladder concerns. For example, individuals that have actually previously delivered might have pelvic flooring disorder.
- If the sacral cord is entailed, urinary system incontinence or retention can be expected.
- Well, while there isn't much urodynamic study to describe the connection between menstruations and urinary incontinence, there is a frequency of incontinence symptoms during ladies's periods.
- Estrogen and progesterone degrees increase continuously while pregnant and reach their optimal in the third trimester.
- There is usually temporary bladder paralysis followed by uncontrolled reflex micturition subsequent to manual compression.
- It is often brought on by particular modifications in body feature that may result from conditions, use medicines and/or the start of an ailment.
- The impact that HRT has on UI depends on the sort of treatment carried out.
Lots of surgical procedures for incontinence can be done under a light sedation, staying clear of the demand for general anesthetic. Bladder dysfunction is a typical obstacle, especially later on in life and throughout times of significant hormone adjustment. Reduced estrogen bladder symptoms can include incontinence, over active bladder, and pain. The science behind INNOVO focuses on Neuromuscular Electrical Excitement (NMES), a tested technique used in various medical settings to fix up muscles and boost muscular tissue function. The suggested dose is 0.2 to 0.4 mg/kg every 8 to 12 hours or 15 to 60 mg/dog. Dismiss ectopic ureters or various other structural irregularities that permit pee to bypass typical sphincters. Purgative urography is made use of to picture the kidneys and determine the program and termination of the ureters and the urinary system bladder. Because of the setting and function of steroids in the urinary tract, making use of replaced hormone treatment in menopause has long brought in the interest of scientists and providers of healthcare in this area. In ladies without urethral hypermobility, the urethra is supported during anxiety by 3 interrelated systems. One device is response, or volunteer, closure of the pelvic flooring. Contraction of the levator ani facility raises the proximal urethra and bladder neck, tightens up undamaged connective cells sustains, and raises the perineal body, which might serve as a urethral backstop. If you're experiencing incontinence during your period or your cycle, it can transform your quality of life.