September 12, 2024
Medical Administration Of Urinary Incontinence In Women
Professional Monitoring Of Urinary Incontinence In Females The Panel ends that while laser or magnetic/ES treatment might supply some advantage contrasted to placebo it remains vital to advise individuals on the immaturity of the data. It shows up present data does not suggest supremacy of these brand-new emerging innovations in contrast to developed non-invasive treatments such as PFME. At some time between six weeks and 6 months after surgical treatment, the individual ought to be assessed and analyzed personally by the doctor or his/her designee to review the outcomes of surgical treatment and to assess for any prospective problems. MUS may be defined as retropubic slings (RMUS; top-down or bottom-up), transobturator slings (TMUS; inside-out or outside-in), single laceration slings (SIS), or adjustable slings.Dr. Meeks highlights the recent innovation in bladder cancer - Urology Times
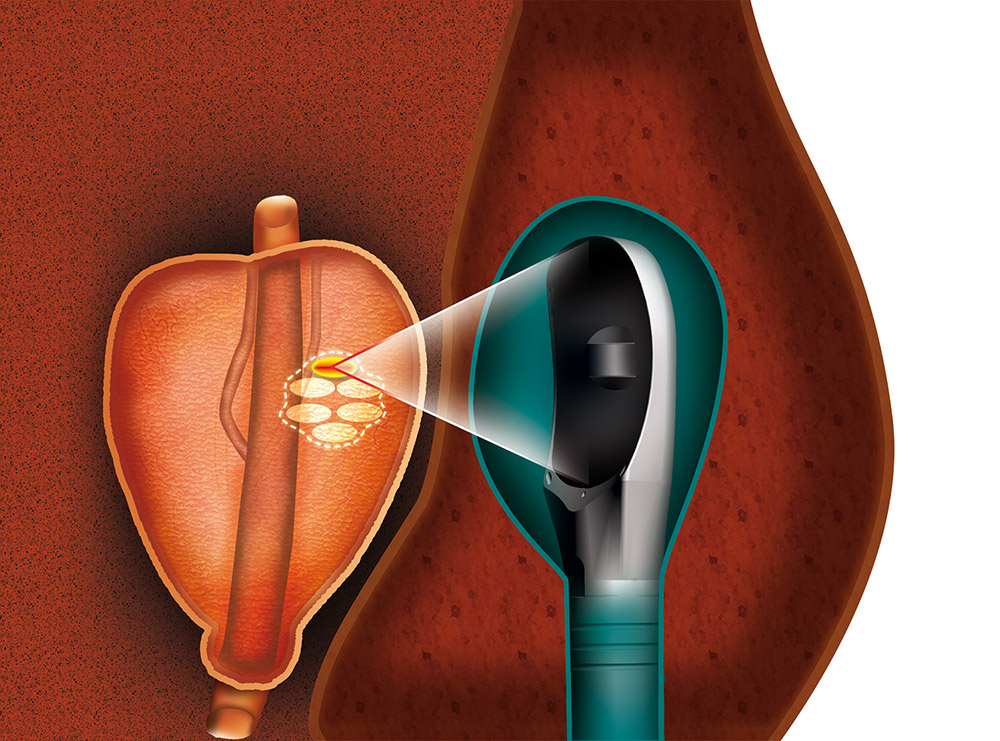
Dr. Meeks highlights the recent innovation in bladder cancer.
Posted: Sat, 04 May 2024 07:00:00 GMT [source]
Options For Managing Post-prostatectomy Urinary Incontinence
Pelvic flooring muscle exercise (PFME) is specified in this Standard as a workout program details to the pelvic flooring muscle mass team that is self-guided as a home exercise program only. The individual might have discovered the program via patient education literary works or with a solitary basic direction session from an ideal specialist. Pelvic flooring muscle training (PFMT) is specified as a training program particular to the pelvic flooring muscle group that is practitioner guided. Generally, PFMT will consist of customized pelvic flooring muscle awareness training utilizing verbal, tactile, and/or visual comments together with a home PFME program to be advanced throughout follow-up sees with the practitioner.- Through the UCLA Health Institute of Urologic Oncology (IUO), our experts go to the forefront of ingenious therapies for urologic cancer, consisting of bladder cancer, kidney cancer cells, testicular cancer cells, and prostate cancer.
- Insufficient recovery of continence after AUS positioning can be as a result of a host of aspects, including suboptimal cuff sizing at the time of original procedure or poor stress managing balloon slope.
- Patients must be aware that with any type of treatment there is a risk of ongoing symptoms of SUI right away after the procedure or frequent SUI at a later time that might require further treatment.
- If are refractory to Kegel sphincter recovery or various other conservative measures such as diet plan, liquid and bladder retraining techniques, 2 minimally-invasive choices might be taken into consideration.
Problems After Surgical Treatment
If clients are having voiding disorder, a decline in the force of their urinary stream, unforeseen discomfort, frequent UTI, new onset dyspareunia, or other unforeseen symptoms, they ought to be assessed personally by the clinician or his/her designee. If proper, depending upon the index surgery, the client can be taught tidy intermittent catheterization (CIC), a catheter can be placed, or surgical treatment may be required. Additionally, in scenarios of preoperative issue pertaining to postoperative voiding dysfunction (e.g., low quality bladder contraction identified on urodynamic examination), CIC guideline should be taken into consideration as a part of preoperative mentor. Considerations might include prior pelvic flooring reconstruction and technique, temporal relationship to any previous surgical procedure, visibility or lack of pelvic prolapse, level of urethral flexibility, concomitant and urinary system urgency or seriousness urinary incontinence signs and symptoms. The third objective of the diagnostic assessment is to help in prognosis and option of therapy. Our urologists are experienced at treating also one of the most complex disorders of the urinary system. If your overactive bladder hasn't improved with lifestyle adjustments and medicines and you don't wish to have surgical procedure, percutaneous tibial nerve stimulation (PTNS) is an alternative. Throughout this strategy, the physician inserts a fine-needle electrode right into the nerve simply over your ankle. The systematic testimonial used to educate this guideline was carried out by a methodology group at ECRI Institute. Resolution of the standard extent and review of the last methodical testimonial to inform standard statements was conducted along with the SUI Panel. The nerves and muscles of the urinary Recovery system collaborate to help your bladder hold and release urine. Lots of innovative urogynecology innovations are still in growth, but this field of study is moving forward rapidly. " And urinary incontinence is additionally a chronic condition that tends to get worse as people age. This means we require a lot of alternatives." There are a variety of treatments for OAB, and scientists are researching a lot more in clinical tests. Refining which person populaces with SUI and BNC/VUAS will gain from synchronous BNC/VUAS therapy and AUS placement instead of organized procedures will boost the QoL of numerous people. 7 trials satisfied inclusion standards regarding the effectiveness of a pre-operative PFMT program boosting post-prostatectomy continence. The toughness of the referral is restricted by heterogeneous approaches of evaluation and contrast among the various research studies. The AUA utilizes a 3-tiered toughness of evidence system to underpin evidence-based guideline declarations. There are couple of realities and several viewpoints regarding forecasting the outcome of surgical treatment based upon the problems described over. Nonetheless few medical professionals would certainly disagree that operations for SUI should be restricted to those who have demonstrable SUI, consisting of occult SUI verifiable only after reduction of pelvic organ prolapse. However, an understanding of the specific concomitant conditions assists in customized therapy preparation and informed permission. It additionally supplies the doctor details with which to formulate a feeling concerning possible outcome and possible issues such as incomplete bladder draining, consistent, worsened, or de novo urgency/UUI, and frequent sphincteric incontinence. Urodynamic examination might serve in illuminating intricate presentations of incontinence.Just how much does the Emsella chair expense?
The Emsella chair treatment expense is generally around $& #x 24; 270-330 for a single session and $& #x 24; 2,000-3,000 for 6 sessions. The overall cost will certainly consider the number of sessions needed based on the existing stamina of a patient''s pelvic flooring muscle mass.
Social Links