Soap Charting Method . Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. wondering how to write soap notes? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is standard across all types of chart. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. there are four basic components of a soap note: Here are soap note examples.
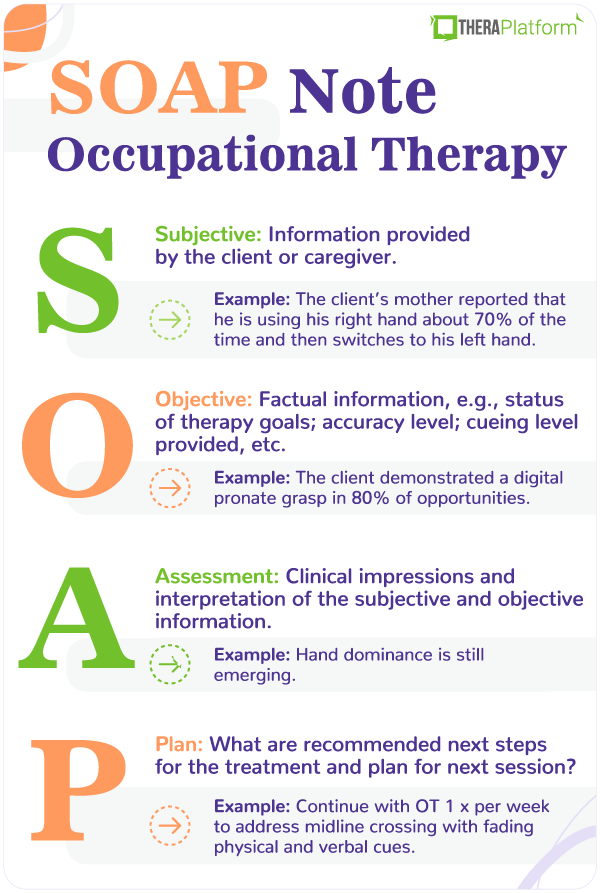
from www.theraplatform.com
— the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic components of a soap note: soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. wondering how to write soap notes? A soap note is standard across all types of chart. Here are soap note examples.
Occupational therapy SOAP note
Soap Charting Method Subjective, objective, assessment, and plan. Subjective, objective, assessment, and plan. there are four basic components of a soap note: Here are soap note examples. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. wondering how to write soap notes? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method Getting the soap format right is essential for therapists. Here are soap note examples. wondering how to write soap notes? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Soap Charting Method.
From slideplayer.com
Chapter 13 Managing Medical Records ppt download Soap Charting Method — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Here are soap note examples. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note is standard across all types of chart. — the subjective, objective,. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method A soap note is standard across all types of chart. Here are soap note examples. there are four basic components of a soap note: soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document. Soap Charting Method.
From www.slideserve.com
PPT Communication of the Nursing Process Documentation PowerPoint Soap Charting Method soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note is standard across all types of chart. Subjective, objective, assessment, and plan. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic. Soap Charting Method.
From tucsonceu.com
Integrating Interview Skills & SOAP Charting into your Treatment Plan Soap Charting Method Here are soap note examples. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic components of a soap note: wondering how to write soap notes? Subjective, objective, assessment, and plan. Getting the soap format right is essential for therapists. soap notes are a highly structured. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method wondering how to write soap notes? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. soap notes are a highly structured format for documenting the progress of a patient during treatment and is. Soap Charting Method.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 Soap Charting Method Subjective, objective, assessment, and plan. wondering how to write soap notes? — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. A soap note is standard across all types of chart. there are four basic components of a soap note: soap notes are a highly structured format for documenting the. Soap Charting Method.
From www.realiaproject.org
11+ SOAP Note Example FREE Download [Word, PDF] Soap Charting Method Here are soap note examples. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. wondering how to write soap notes? A soap note is standard across all types of chart. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters. Soap Charting Method.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Charting Method wondering how to write soap notes? A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. there are four basic components of a soap note: — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is standard across all types of chart. wondering how to write soap notes? Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. soap notes are a highly structured format for documenting the progress. Soap Charting Method.
From www.vrogue.co
Sample Soap Notes Occupational Therapy Pdf Fill Out A vrogue.co Soap Charting Method Here are soap note examples. Getting the soap format right is essential for therapists. wondering how to write soap notes? — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. there are four basic components of a soap note: A soap note is standard across all types of chart. Subjective, objective,. Soap Charting Method.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Charting Method Subjective, objective, assessment, and plan. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Getting the soap format right is essential for therapists. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Here are soap note examples. . Soap Charting Method.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Charting Method Here are soap note examples. there are four basic components of a soap note: wondering how to write soap notes? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. A. Soap Charting Method.
From www.etsy.com
SOAP Notes Etsy Soap Charting Method Subjective, objective, assessment, and plan. Here are soap note examples. Getting the soap format right is essential for therapists. wondering how to write soap notes? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. there are four basic components of a soap note: . Soap Charting Method.
From www.slideserve.com
PPT Medical Records and Documentation PowerPoint Presentation, free Soap Charting Method Subjective, objective, assessment, and plan. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Here are soap note examples. there are four basic components of a soap note: A soap note is standard across all types of chart. soap notes are a highly structured format for documenting the progress of. Soap Charting Method.
From www.slideserve.com
PPT Nursing Fundamentals Chapter 9 Recording & Reporting PowerPoint Soap Charting Method Getting the soap format right is essential for therapists. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. there are four basic components of a soap note: Here. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. there are four basic components of a soap note: Here are soap note examples. wondering how to write soap notes? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Getting the soap format. Soap Charting Method.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 Soap Charting Method wondering how to write soap notes? Subjective, objective, assessment, and plan. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Here are soap note examples. A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. — soap—or subjective, objective, assessment and. Soap Charting Method.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Charting Method — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Here are soap note examples. there are four basic components of a soap note: A soap note is standard across all types of chart. wondering how to write soap notes? Getting the soap format right is essential for therapists. soap. Soap Charting Method.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Charting Method soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Here are soap note examples. there are four basic components of a soap note: Getting the soap format right is essential for therapists. — the subjective, objective, assessment and plan (soap) note is an acronym. Soap Charting Method.
From www.advantismed.com
How to Master Nurse Charting & Avoid Mistakes Soap Charting Method there are four basic components of a soap note: A soap note is standard across all types of chart. Here are soap note examples. wondering how to write soap notes? Subjective, objective, assessment, and plan. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many.. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Getting the soap format right is essential for therapists. wondering how to write soap notes? there are four basic components of a soap note: — the subjective, objective, assessment and plan (soap) note is. Soap Charting Method.
From studylib.net
Patient SOAP Note Charting Procedures Soap Charting Method — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. wondering how to write soap notes? Here are soap note examples. Subjective, objective, assessment, and plan. there are four basic components of a soap note: A soap note is standard across all types of chart. soap notes are a highly. Soap Charting Method.
From covenantlifecog.com
SOAPmethodposter Soap Charting Method A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Here are soap note examples. Subjective, objective, assessment, and plan. soap notes are a highly structured format for documenting the progress of a. Soap Charting Method.
From slideplayer.com
Chapter 13 Managing Medical Records ppt download Soap Charting Method wondering how to write soap notes? there are four basic components of a soap note: — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Here are soap note examples. A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. Subjective, objective,. Soap Charting Method.
From dxoghuaue.blob.core.windows.net
Soap Define Method at Victoria Yin blog Soap Charting Method Here are soap note examples. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is standard across all types of chart. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Subjective, objective, assessment, and plan. wondering how to write soap. Soap Charting Method.
From quizzmediasophie.z13.web.core.windows.net
The E Entry In The Soaper Charting Method Means Soap Charting Method Subjective, objective, assessment, and plan. Getting the soap format right is essential for therapists. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. A soap note is standard across all types of chart. soap notes are a highly structured format for documenting the progress of a patient during treatment and is. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method Getting the soap format right is essential for therapists. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. there are four basic components of a soap note: A. Soap Charting Method.
From www.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract Soap Charting Method A soap note is standard across all types of chart. Here are soap note examples. there are four basic components of a soap note: Subjective, objective, assessment, and plan. Getting the soap format right is essential for therapists. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one. Soap Charting Method.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Charting Method Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. there are four basic components of a soap note: — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. wondering. Soap Charting Method.
From clinicsense.com
ClinicSense Write Effective Massage Therapy SOAP Notes + Examples Soap Charting Method A soap note is standard across all types of chart. wondering how to write soap notes? there are four basic components of a soap note: Subjective, objective, assessment, and plan. Getting the soap format right is essential for therapists. Here are soap note examples. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. wondering how to write soap notes? — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. — the subjective, objective, assessment and plan (soap) note is an acronym. Soap Charting Method.
From www.pinterest.com
SOAP vs SBAR Nursing school survival, Nursing school tips, Nursing Soap Charting Method Getting the soap format right is essential for therapists. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. wondering how to write soap notes? A soap note is standard across all types of chart. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a.. Soap Charting Method.
From lucadavies.z19.web.core.windows.net
The R Entry In The Soaper Charting Method Means Soap Charting Method — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Subjective, objective, assessment, and plan. Getting the soap format right is essential for therapists. wondering how to write soap notes? A soap note is standard across all types of chart. Here are soap note examples. — soap—or subjective, objective, assessment and. Soap Charting Method.
From www.theraplatform.com
Occupational therapy SOAP note Soap Charting Method Subjective, objective, assessment, and plan. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. wondering how to write soap notes? Here are soap note examples. . Soap Charting Method.