Define Retro Authorization Medical Billing . This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes.
from authorizationletter.org
Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization secures approval for medical services already rendered to a patient. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. It refers to obtaining approval for medical services.
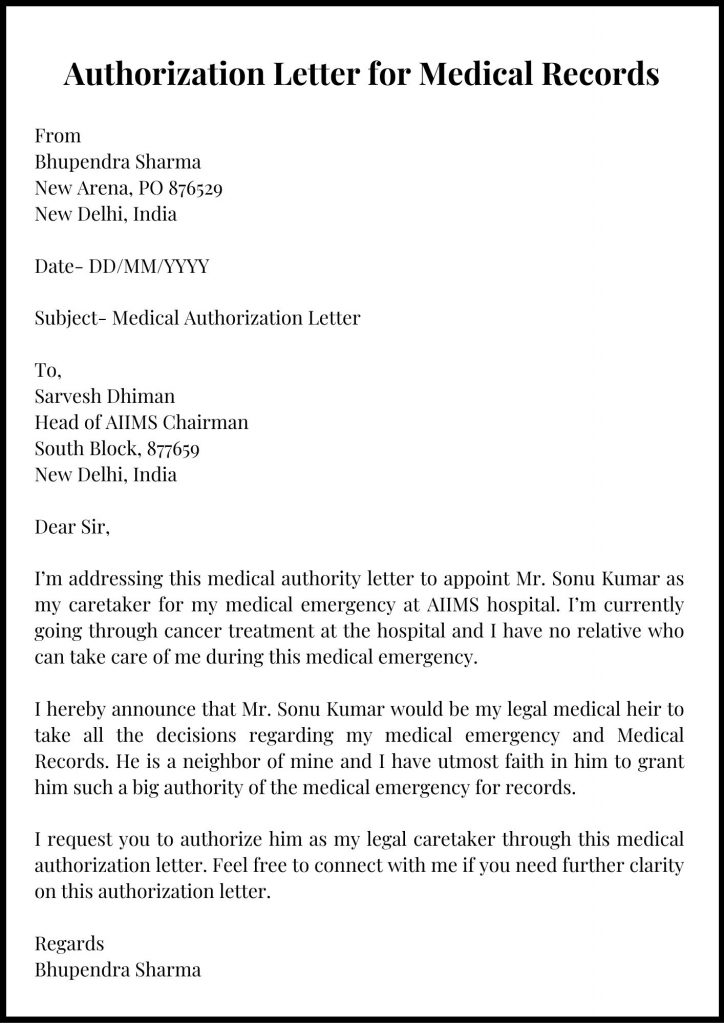
Sample Authorization Letter for Medical Records Example
Define Retro Authorization Medical Billing Retro authorization secures approval for medical services already rendered to a patient. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. It refers to obtaining approval for medical services. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization secures approval for medical services already rendered to a patient. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes.
From www.outsourcestrategies.com
Retro Authorization in Medical Billing Define Retro Authorization Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. It refers to obtaining approval for medical services. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retroactive authorization refers to requests made to the insurance company. Define Retro Authorization Medical Billing.
From umbsbillingservices.com
What Is Retro Authorization in Medical Billing? Define Retro Authorization Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization is eligible in medical billing when a service that was already performed needs to. Define Retro Authorization Medical Billing.
From revtrailmed.com
Authorization Services RevTrail Your Premier Medical Billing Company Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retroactive authorization refers. Define Retro Authorization Medical Billing.
From www.carecloud.com
Complete Guide Prior Authorization in Medical Billing? Define Retro Authorization Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. It refers to obtaining approval for medical services.. Define Retro Authorization Medical Billing.
From www.caplinedentalservices.com
What is authorization in medical billing? Capline Dental Sservices Define Retro Authorization Medical Billing It refers to obtaining approval for medical services. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. This article aims to shed light on the different types of. Define Retro Authorization Medical Billing.
From rightmedicalbilling.com
Prior and Retro Authorization Services Right Medical Billing Define Retro Authorization Medical Billing Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. This article aims. Define Retro Authorization Medical Billing.
From templates.rjuuc.edu.np
Medical Authorization Template Define Retro Authorization Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. This article aims to shed light on the different types of authorization in medical billing, highlighting. Define Retro Authorization Medical Billing.
From www.upwork.com
Prior Authorization and Retro Authorization Services Upwork Define Retro Authorization Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement. Define Retro Authorization Medical Billing.
From businesshobbie.com
Steps Involved In The Medical Billing Process Business Hobbie Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. It refers to obtaining approval for medical services. This article aims to shed light on the different types. Define Retro Authorization Medical Billing.
From umbsbillingservices.com
What Is Retro Authorization in Medical Billing? Define Retro Authorization Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. It refers to obtaining approval for medical services. Retro authorization secures approval for medical services already rendered to a patient. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified. Define Retro Authorization Medical Billing.
From www.caplinehealthcaremanagement.com
What is Authorization in Medical Billing Define Retro Authorization Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. It refers to obtaining approval for medical services. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment. Define Retro Authorization Medical Billing.
From www.slideserve.com
PPT Understanding Insurance Prior Authorization Process PowerPoint Define Retro Authorization Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. This article aims to shed light on the different types of. Define Retro Authorization Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF Define Retro Authorization Medical Billing It refers to obtaining approval for medical services. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. This article aims to shed light on the different types of authorization in medical billing,. Define Retro Authorization Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF Define Retro Authorization Medical Billing Retro authorization secures approval for medical services already rendered to a patient. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization also known. Define Retro Authorization Medical Billing.
From medicalbillingdoubts.com
What is Authorization Number? MEDICAL BILLING AR CALLING JOBS Define Retro Authorization Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization is the process of getting permission. Define Retro Authorization Medical Billing.
From www.caplinehealthcaremanagement.com
What is Preauthorization in Medical Billing Define Retro Authorization Medical Billing This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retroactive authorization refers to requests made to the insurance company for. Define Retro Authorization Medical Billing.
From umbsbillingservices.com
What Is Retro Authorization in Medical Billing? Define Retro Authorization Medical Billing This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier.. Define Retro Authorization Medical Billing.
From www.dochub.com
Wellcare retro authorization form Fill out & sign online DocHub Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. It refers to obtaining approval for medical services. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing. Define Retro Authorization Medical Billing.
From medicalbillingrcm.com
What is Pre Authorization in Medical Billing? Define Retro Authorization Medical Billing It refers to obtaining approval for medical services. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retro authorization secures. Define Retro Authorization Medical Billing.
From www.slideserve.com
PPT Role of Prior Authorization in Medical Billing PowerPoint Define Retro Authorization Medical Billing This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization secures approval for medical services already rendered to a patient. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization is eligible. Define Retro Authorization Medical Billing.
From authorizationletter.org
Sample Authorization Letter for Medical Records Example Define Retro Authorization Medical Billing This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization secures approval for medical services already rendered to a patient. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is. Define Retro Authorization Medical Billing.
From precisebs.com
Importance of Authorization in Medical Billing Precisebs Define Retro Authorization Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. It refers to obtaining approval for medical services. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retro authorization secures approval for medical services already rendered to a patient. Retro authorization is the process. Define Retro Authorization Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF Define Retro Authorization Medical Billing Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period. Define Retro Authorization Medical Billing.
From www.pdffiller.com
Fillable Online Retroactive eligibility authorization process Fax Email Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. It refers to obtaining approval for medical services. Retro authorization is eligible in medical billing when a service. Define Retro Authorization Medical Billing.
From www.caplinehealthcaremanagement.com
Difference between authorization and preauthorization in medical billing Define Retro Authorization Medical Billing Retro authorization secures approval for medical services already rendered to a patient. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization is eligible in medical. Define Retro Authorization Medical Billing.
From jqqwmseqmh.blogspot.com
RetroAuthorization Example Letter Printable retro authorization Define Retro Authorization Medical Billing Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. It refers to obtaining approval for medical services. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retroactive authorization refers to requests made to the. Define Retro Authorization Medical Billing.
From www.pdffiller.com
Fillable Online Retro Authorization Process Fax Email Print pdfFiller Define Retro Authorization Medical Billing Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights. Define Retro Authorization Medical Billing.
From www.caplinehealthcaremanagement.com
What Is Meant By Retro Authorization In Medical Billing? Define Retro Authorization Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes. Define Retro Authorization Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services. Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization also known as retrospective. Define Retro Authorization Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF Define Retro Authorization Medical Billing Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their. Define Retro Authorization Medical Billing.
From ircm.com
Optimizing Retro Authorization for Medical Billing Success Define Retro Authorization Medical Billing Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been. Define Retro Authorization Medical Billing.
From www.caplinehealthcaremanagement.com
What Are Referrals In Medical Billing and Why Are They Needed? Define Retro Authorization Medical Billing Retro authorization is the process of getting permission from an insurance company for a medical treatment rendered earlier. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time has ended. In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes.. Define Retro Authorization Medical Billing.
From umbsbillingservices.com
What Is Retro Authorization in Medical Billing? Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective. Define Retro Authorization Medical Billing.
From rightmedicalbilling.com
Medical Billing Services in Illinois Right Medical Billing Define Retro Authorization Medical Billing In the realm of medical billing, retro authorization, or retroactive authorization, ensures precision in reimbursement processes. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing. Define Retro Authorization Medical Billing.
From ircm.com
Optimizing Retro Authorization for Medical Billing Success Define Retro Authorization Medical Billing It refers to obtaining approval for medical services. This article aims to shed light on the different types of authorization in medical billing, highlighting their significance and providing insights into their respective processes and. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is eligible in medical billing. Define Retro Authorization Medical Billing.