Soaps Writing Format . Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Each letter refers to one of four sections in the document. They contain four primary sections, represented by its acronym: In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. All case notes start with the date and. Here’s how to tackle each. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition.
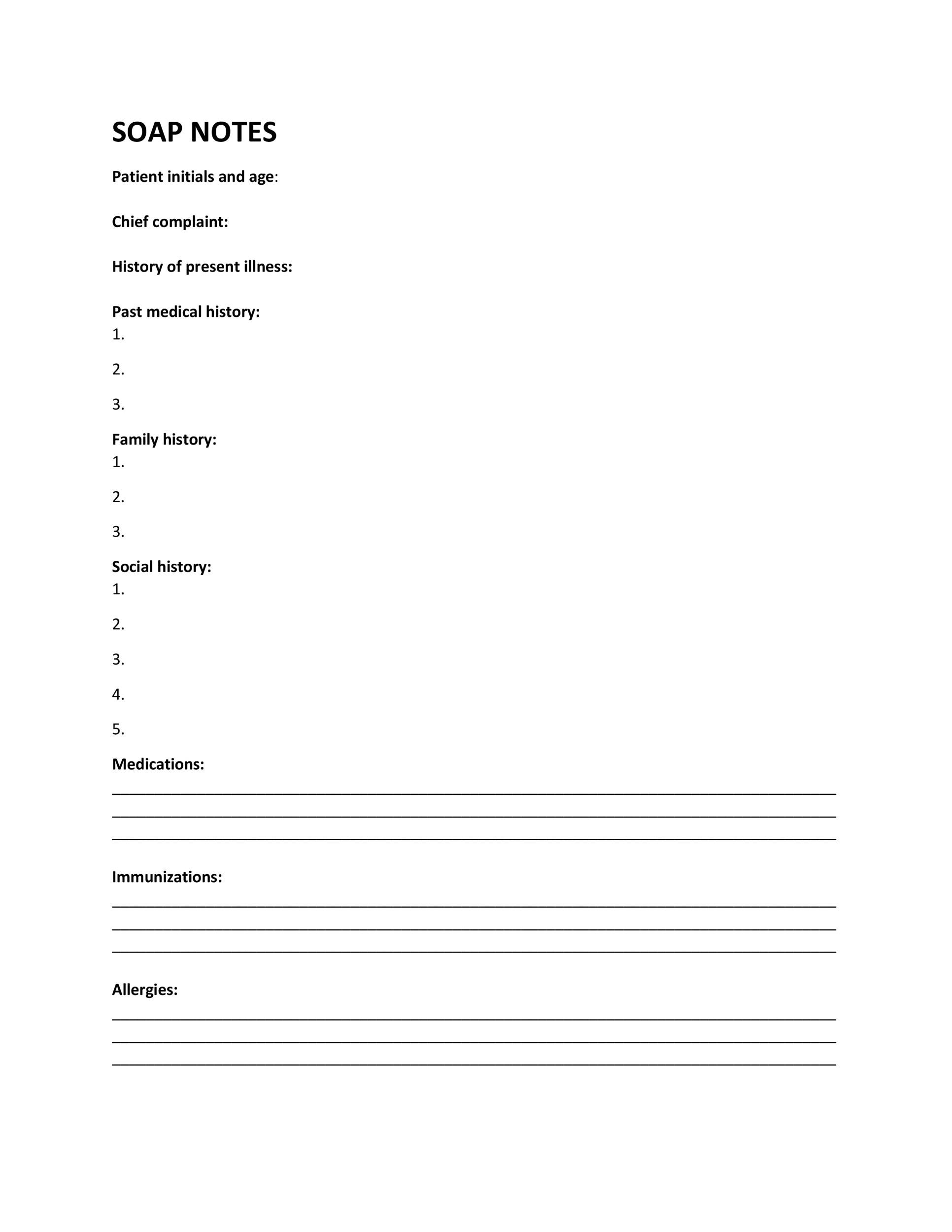
from templatelab.com
A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. All case notes start with the date and. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. Here’s how to tackle each. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document.
40 Fantastic SOAP Note Examples & Templates Template Lab
Soaps Writing Format Here’s how to tackle each. Here’s how to tackle each. All case notes start with the date and. They contain four primary sections, represented by its acronym: Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Each letter refers to one of four sections in the document. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
From www.wordtemplatesonline.net
How to Write a SOAP Note (20+ SOAP Note Examples) Soaps Writing Format In the soap format, soap stands for subjective, objective, assessment, and plan. They contain four primary sections, represented by its acronym: Each letter refers to one of four sections in the document. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. All case notes start with the date and. Soap notes can provide consistent. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Here’s how to tackle each. A soap note is a method of documentation used by healthcare providers, including pas, physicians and. Soaps Writing Format.
From www.wordtemplatesonline.net
35+ SOAP Note Examples (Blank Formats & Writing Tips) Soaps Writing Format In the soap format, soap stands for subjective, objective, assessment, and plan. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Here’s how to tackle each. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Soap notes can. Soaps Writing Format.
From thevisualcommunicationguy.com
SOAPStoneWritingStrategy_Reference The Visual Communication Guy Soaps Writing Format Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes can provide consistent documentation to monitor the client’s progress and to. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format In the soap format, soap stands for subjective, objective, assessment, and plan. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. All case notes start with the date and. Soap notes are a specific format for writing progress notes as a behavioral health clinician.. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soaps Writing Format Each letter refers to one of four sections in the document. They contain four primary sections, represented by its acronym: Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. Soap notes are a specific format for writing progress notes as a behavioral health clinician. A soap note is a method. Soaps Writing Format.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soaps Writing Format They contain four primary sections, represented by its acronym: A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Each letter refers to one of four sections in the document. Writing soap notes might seem daunting at first, but with practice, it becomes second nature.. Soaps Writing Format.
From www.pinterest.jp
Beginner’s Guide to Writing a SOAP Note (with SOAP note template) My Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soaps Writing Format Here’s how to tackle each. Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for subjective, objective, assessment, and plan. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Writing soap notes properly is crucial in healthcare as they provide a structured. Soaps Writing Format.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soaps Writing Format Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. They contain four primary sections, represented by its acronym: All case notes start with the date and. Each letter refers to one of four sections in the document. Soap notes can provide consistent documentation to monitor the client’s progress and to. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format In the soap format, soap stands for subjective, objective, assessment, and plan. All case notes start with the date and. They contain four primary sections, represented by its acronym: Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes can provide. Soaps Writing Format.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soaps Writing Format Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Here’s how to tackle each. Writing soap notes properly is crucial in healthcare as they provide a structured way. Soaps Writing Format.
From www.sampletemplates.com
Soap Note Template 10 Download Free Documents in PDF , Word Soaps Writing Format Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information. Soaps Writing Format.
From gradecrest.com
Soap Notes A Howto write Guide, Templates, and Samples Soaps Writing Format They contain four primary sections, represented by its acronym: In the soap format, soap stands for subjective, objective, assessment, and plan. Here’s how to tackle each. Soap notes are a specific format for writing progress notes as a behavioral health clinician. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write. Soaps Writing Format.
From www.pinterest.ca
Soap Note Template Word Fresh 35 soap Note Examples Blank formats Soaps Writing Format All case notes start with the date and. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring.. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soaps Writing Format Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. In the soap format, soap stands for subjective, objective, assessment, and plan. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Here’s how to tackle each.. Soaps Writing Format.
From www.theraplatform.com
Occupational therapy SOAP note Soaps Writing Format They contain four primary sections, represented by its acronym: Here’s how to tackle each. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. Each letter refers to one of four sections. Soaps Writing Format.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soaps Writing Format Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. Here’s how to tackle each. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. They contain four primary sections,. Soaps Writing Format.
From www.youtube.com
How to Write SOAP Format for Mental Health Counselors YouTube Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Here’s how to tackle each. In the soap format, soap stands for subjective, objective, assessment, and plan. All case notes start with the date and. Writing soap notes properly is. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for subjective, objective, assessment, and plan. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions,. Soaps Writing Format.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soaps Writing Format Each letter refers to one of four sections in the document. All case notes start with the date and. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format They contain four primary sections, represented by its acronym: A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Here’s how to tackle each. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for. Soaps Writing Format.
From www.wikihow.com
How to Write a Soap Note (with Pictures) wikiHow Soaps Writing Format They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. All case notes start with the date and. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. In the soap. Soaps Writing Format.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soaps Writing Format Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses,. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format All case notes start with the date and. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soaps Writing Format All case notes start with the date and. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Each letter refers to one of four sections in the document. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Writing. Soaps Writing Format.
From www.artemisaba.com
ABA SOAP Notes Tips, Examples & Template Artemis ABA Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for subjective, objective, assessment, and plan. All case notes start with the date and. They contain four primary sections, represented by its acronym: Here’s how to tackle each. Soap notes can provide consistent documentation to monitor the client’s progress. Soaps Writing Format.
From www.sampletemplates.com
FREE 8+ Sample Soap Note Templates in MS Word PDF Soaps Writing Format Soap notes are a specific format for writing progress notes as a behavioral health clinician. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. In. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format They contain four primary sections, represented by its acronym: All case notes start with the date and. Writing soap notes might seem daunting at first, but with practice, it becomes second nature. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. In the soap format, soap. Soaps Writing Format.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soaps Writing Format Writing soap notes might seem daunting at first, but with practice, it becomes second nature. They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. Soap. Soaps Writing Format.
From www.slideshare.net
SOAP Notes Dentistry Example Soaps Writing Format Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. Here’s how to tackle each. Writing soap notes properly is crucial in healthcare as. Soaps Writing Format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soaps Writing Format They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. A soap note is a method of documentation used by healthcare providers, including pas, physicians and nurses, to write down information about a patient's condition. Soap notes are a specific format for writing progress notes. Soaps Writing Format.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soaps Writing Format Here’s how to tackle each. Soap notes can provide consistent documentation to monitor the client’s progress and to gain a holistic view of each session with the client. Writing soap notes properly is crucial in healthcare as they provide a structured way to document patient interactions, ensuring. In the soap format, soap stands for subjective, objective, assessment, and plan. Writing. Soaps Writing Format.