Example Of Medical Notes . Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. The acronym stands for subjective, objective, assessment, and plan: The subjective section captures the patient's personal experience, symptoms, and medical history. Then, use the soap method to. It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
from www.examples.com
Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. The subjective section captures the patient's personal experience, symptoms, and medical history. Then, use the soap method to. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective, objective, assessment, and plan:
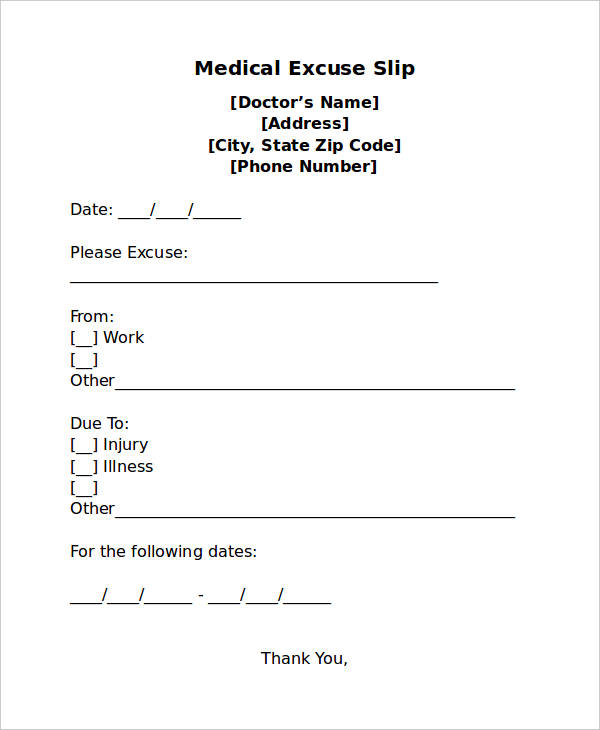
Doctor's Note 17+ Examples, How to Get, PDF
Example Of Medical Notes They contain four primary sections, represented by its acronym: It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. The subjective section captures the patient's personal experience, symptoms, and medical history. The acronym stands for subjective, objective, assessment, and plan: Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Start your clinical note by briefly summarizing the main presenting issues. Then, use the soap method to. Soap notes are a standardized method for documenting patient information in healthcare. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. They contain four primary sections, represented by its acronym:
From www.sampletemplates.com
FREE 9+ Medical Note Samples in MS Word PDF Example Of Medical Notes A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. The subjective section captures the patient's personal experience, symptoms, and medical history. The acronym stands for subjective, objective, assessment, and. Example Of Medical Notes.
From www.sampletemplates.com
FREE 9+ Medical Note Samples in MS Word PDF Example Of Medical Notes A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. The acronym stands for subjective, objective, assessment, and plan: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective section. Example Of Medical Notes.
From templatearchive.com
30 Useful Nursing Note Samples (+Templates) TemplateArchive Example Of Medical Notes Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective, objective, assessment, and plan: The subjective section captures the patient's personal experience, symptoms, and medical history. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Soap notes are a widely used and accepted format by. Example Of Medical Notes.
From www.template.net
13+ FREE Sample Doctor Note Templates [Edit & Download] Example Of Medical Notes The acronym stands for subjective, objective, assessment, and plan: Then, use the soap method to. Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It’s like having. Example Of Medical Notes.
From www.samplenotes.net
Medical Note Template Free Word Template, Format & Example Example Of Medical Notes Then, use the soap method to. Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective section captures. Example Of Medical Notes.
From templatelab.com
36 Free Doctor Note Templates [for Work or School] Example Of Medical Notes Start your clinical note by briefly summarizing the main presenting issues. They contain four primary sections, represented by its acronym: A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. Soap. Example Of Medical Notes.
From geekymedics.com
Writing in the Notes an overview Geeky Medics Example Of Medical Notes Soap notes are a standardized method for documenting patient information in healthcare. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. The acronym stands for subjective, objective, assessment, and plan: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented. Example Of Medical Notes.
From www.carepatron.com
Clinical Progress Notes Template & Example Free PDF Download Example Of Medical Notes A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare.. Example Of Medical Notes.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Example Of Medical Notes Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective section captures the patient's personal experience, symptoms, and medical history. Soap notes are a specific format for writing progress notes as a behavioral health clinician. It’s like having a second pair of eyes and ears but with the precision of a surgeon. Example Of Medical Notes.
From www.sampletemplates.com
FREE 33+ Doctor Note Samples in MS Word Example Of Medical Notes Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective, objective, assessment, and plan: A patient’s notes consist of ward round notes, consultations—that. Example Of Medical Notes.
From templatediy.com
Doctors Note For Surgery Template Printable in PDF & Word Example Of Medical Notes The subjective section captures the patient's personal experience, symptoms, and medical history. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Start your clinical note by briefly summarizing the main. Example Of Medical Notes.
From www.doctorsnote.com
DoctorsNote Real Online Doctor's Notes Example Of Medical Notes Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Start your clinical note by briefly summarizing the main presenting issues. They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It’s. Example Of Medical Notes.
From www.docformats.com
Medical Note Template 30+ Doctor Note Samples Example Of Medical Notes A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. They contain four primary sections, represented by its acronym:. Example Of Medical Notes.
From templatelab.com
36 Free Doctor Note Templates [for Work or School] Example Of Medical Notes Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Start your clinical note by briefly summarizing the main presenting issues. It’s like having a second pair of eyes and ears but with the precision of a. Example Of Medical Notes.
From www.sampletemplates.com
FREE 9+ Medical Note Samples in MS Word PDF Example Of Medical Notes Start your clinical note by briefly summarizing the main presenting issues. The acronym stands for subjective, objective, assessment, and plan: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective section captures the patient's personal experience, symptoms, and medical history. Soap notes are a standardized method for documenting patient information in healthcare.. Example Of Medical Notes.
From www.sampletemplates.com
FREE 9+ Medical Note Samples in MS Word PDF Example Of Medical Notes Then, use the soap method to. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Soap notes are a specific format. Example Of Medical Notes.
From www.carepatron.com
Patient Note Template & Example Free PDF Download Example Of Medical Notes Soap notes are a standardized method for documenting patient information in healthcare. They contain four primary sections, represented by its acronym: The subjective section captures the patient's personal experience, symptoms, and medical history. Start your clinical note by briefly summarizing the main presenting issues. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations,. Example Of Medical Notes.
From www.examples.com
Progress Note 18+ Examples, Format, How to Write, Pdf Example Of Medical Notes Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective, objective, assessment, and plan: A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. It’s like having a second pair. Example Of Medical Notes.
From templatelab.com
36 Free Doctor Note Templates [for Work or School] Example Of Medical Notes Then, use the soap method to. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective, objective, assessment, and plan: It’s like having a second pair of eyes and ears but with the precision of a surgeon. Example Of Medical Notes.
From www.docformats.com
Medical Note Template 30+ Doctor Note Samples Example Of Medical Notes Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective, objective, assessment, and plan: Then, use the soap method to. Soap notes are a specific format. Example Of Medical Notes.
From www.docformats.com
Medical Note Template 30+ Doctor Note Samples Example Of Medical Notes They contain four primary sections, represented by its acronym: Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective, objective, assessment, and plan: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective section captures the patient's personal experience, symptoms, and medical history. Start your. Example Of Medical Notes.
From sample-templates123.com
Medical Note Template How To Create One In 2023 Free Sample, Example Example Of Medical Notes Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective, objective, assessment, and plan: Then, use the soap method to. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to. Example Of Medical Notes.
From www.101planners.com
FREE Customizable and Printable Doctors Note Templates Example Of Medical Notes Soap notes are a specific format for writing progress notes as a behavioral health clinician. Start your clinical note by briefly summarizing the main presenting issues. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Then, use the soap method to. The subjective section captures the. Example Of Medical Notes.
From www.docformats.com
Medical Note Template 30+ Doctor Note Samples Example Of Medical Notes The acronym stands for subjective, objective, assessment, and plan: Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. The subjective section captures the patient's personal experience, symptoms, and medical. Example Of Medical Notes.
From www.samplenotes.net
Medical Note How to Get a Doctor's Note (with Samples & Templates) Example Of Medical Notes Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Then, use the soap method to. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers,. Example Of Medical Notes.
From bestprofessionaltemplate01.blogspot.com
Medical Office Note Template Great Professional Template Example Of Medical Notes Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. The acronym stands for subjective, objective, assessment, and plan: The subjective section captures the patient's personal experience, symptoms, and medical history. It’s like having a second pair of eyes and ears but with the precision of a. Example Of Medical Notes.
From www.docformats.com
Medical Note Template 30+ Doctor Note Samples Example Of Medical Notes Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Start your clinical note by briefly summarizing the main presenting issues. It’s like having a second pair of eyes and ears but with the precision of a surgeon and. Example Of Medical Notes.
From www.docformats.com
Medical Note Template 30+ Doctor Note Samples Example Of Medical Notes It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. The subjective section captures the patient's personal experience, symptoms, and medical history. The acronym stands for subjective, objective, assessment, and plan: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Start. Example Of Medical Notes.
From www.template.net
5+ Medical Progress Note Templates PDF Example Of Medical Notes The subjective section captures the patient's personal experience, symptoms, and medical history. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. Start your clinical note by briefly summarizing the main presenting. Example Of Medical Notes.
From templatelab.com
36 Free Doctor Note Templates [for Work or School] Example Of Medical Notes Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed. Example Of Medical Notes.
From www.dexform.com
Sample doctor’s note in Word and Pdf formats Example Of Medical Notes Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. Soap notes are a specific format for writing progress notes as a behavioral health clinician. A patient’s notes consist of ward. Example Of Medical Notes.
From www.examples.com
Doctor's Note 17+ Examples, How to Get, PDF Example Of Medical Notes A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and. They contain four primary sections, represented by its acronym: Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. The subjective section captures the patient's personal experience, symptoms, and medical. Example Of Medical Notes.
From templatelab.com
36 Free Doctor Note Templates [for Work or School] Example Of Medical Notes Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social workers, to capture. The subjective section captures the patient's personal experience, symptoms, and medical history. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Soap. Example Of Medical Notes.
From www.examples.com
Medical Note 8+ Examples, Format, How to Get, Pdf Example Of Medical Notes Then, use the soap method to. They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective section captures the patient's personal experience, symptoms, and medical history. A patient’s notes consist of ward round notes, consultations—that is, visits from other specialties—results of investigations, and.. Example Of Medical Notes.
From www.examples.com
Medical Note 8+ Examples, Format, How to Get, Pdf Example Of Medical Notes Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: It’s like having a second pair of eyes and ears but with the precision of a surgeon and the speed of lightning. Start your clinical note by briefly summarizing the main presenting issues. The acronym. Example Of Medical Notes.