What Does Medicare Pay For Hospital Stays . After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. The exact amount of coverage that medicare provides depends on how long a person. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. You’re admitted to the hospital as. For days 61 through 90, the beneficiary must pay a daily. Medicare doesn't cover 100% of hospital bills. How much does medicare pay for you to stay in a hospital?
from www.kff.org
The exact amount of coverage that medicare provides depends on how long a person. How much does medicare pay for you to stay in a hospital? You’re admitted to the hospital as. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare doesn't cover 100% of hospital bills. For days 61 through 90, the beneficiary must pay a daily. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers the first 60 days of a hospital stay after a person has paid their deductible.
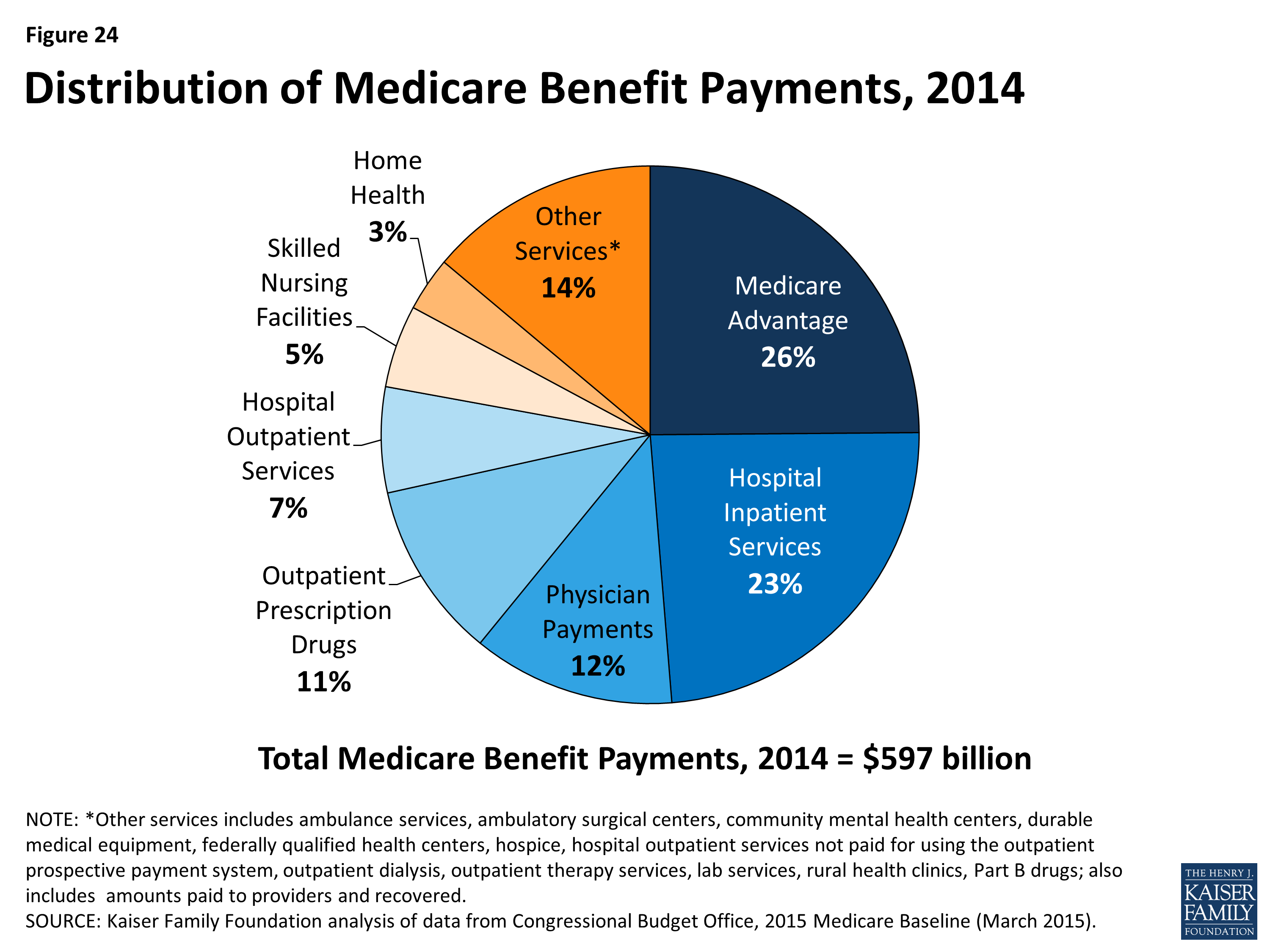
A Primer on Medicare How much does Medicare spend, and how does
What Does Medicare Pay For Hospital Stays Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. For days 61 through 90, the beneficiary must pay a daily. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare doesn't cover 100% of hospital bills. You’re admitted to the hospital as. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. How much does medicare pay for you to stay in a hospital? The exact amount of coverage that medicare provides depends on how long a person. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible.
From www.kff.org
How Much Could Medicare Beneficiaries Pay For a Hospital Stay Related What Does Medicare Pay For Hospital Stays For days 61 through 90, the beneficiary must pay a daily. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. The exact amount of coverage that medicare provides depends on how long a person. Medicare doesn't cover 100% of hospital bills. Medicare covers the first 60 days of a. What Does Medicare Pay For Hospital Stays.
From www.wsj.com
Hospitals Brace for New Medicare Payment Rules WSJ What Does Medicare Pay For Hospital Stays You’re admitted to the hospital as. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. The exact amount of coverage that medicare provides depends on how long a person. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare. What Does Medicare Pay For Hospital Stays.
From www.kff.org
10 Essential Facts About Medicare's Financial Outlook KFF What Does Medicare Pay For Hospital Stays Medicare doesn't cover 100% of hospital bills. The exact amount of coverage that medicare provides depends on how long a person. You’re admitted to the hospital as. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare covers the first 60 days of a hospital stay after a person. What Does Medicare Pay For Hospital Stays.
From www.health.gov.au
Medicare billing in public hospitals overview Australian Government What Does Medicare Pay For Hospital Stays You’re admitted to the hospital as. The exact amount of coverage that medicare provides depends on how long a person. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. How much does medicare. What Does Medicare Pay For Hospital Stays.
From www.federalregister.gov
Federal Register Medicare Program; FY 2022 Hospice Wage Index and What Does Medicare Pay For Hospital Stays Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare pays for the first 60 days. What Does Medicare Pay For Hospital Stays.
From www.ahrq.gov
Declining Hospital Costs for Seniors with Traditional Medicare Agency What Does Medicare Pay For Hospital Stays How much does medicare pay for you to stay in a hospital? The exact amount of coverage that medicare provides depends on how long a person. For days 61 through 90, the beneficiary must pay a daily. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each. What Does Medicare Pay For Hospital Stays.
From www.aha.org
Infographic Medicare Significantly Underpays Hospitals for Cost of What Does Medicare Pay For Hospital Stays The exact amount of coverage that medicare provides depends on how long a person. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which. What Does Medicare Pay For Hospital Stays.
From www.peoplekeep.com
How much does a hospital stay cost? What Does Medicare Pay For Hospital Stays After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare doesn't cover 100% of hospital bills. How much does medicare pay for you to stay in a hospital? Medicare pays for the first 60 days of qualifying inpatient. What Does Medicare Pay For Hospital Stays.
From www.kff.org
How Much Could Medicare Beneficiaries Pay For a Hospital Stay Related What Does Medicare Pay For Hospital Stays Medicare doesn't cover 100% of hospital bills. Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance.. What Does Medicare Pay For Hospital Stays.
From medicare-faqs.com
What Does Medicare Pay For Hospital Stays What Does Medicare Pay For Hospital Stays Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. You’re admitted to the. What Does Medicare Pay For Hospital Stays.
From www.medicarefaq.com
Medicare Part A Hospital Coverage and Benefits for 2021 MedicareFAQ What Does Medicare Pay For Hospital Stays Medicare doesn't cover 100% of hospital bills. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of. What Does Medicare Pay For Hospital Stays.
From sphweb.bumc.bu.edu
Paying for Health Care in the US What Does Medicare Pay For Hospital Stays The exact amount of coverage that medicare provides depends on how long a person. For days 61 through 90, the beneficiary must pay a daily. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible.. What Does Medicare Pay For Hospital Stays.
From www.sutterhealth.org
Medicare Advantage Sutter Health What Does Medicare Pay For Hospital Stays You’re admitted to the hospital as. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. For days 61 through 90, the beneficiary must pay a daily. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare doesn't cover 100% of hospital bills.. What Does Medicare Pay For Hospital Stays.
From www.medicarefaq.com
Medicare Coverage for Cancer Treatments (Chemo and Immunotherapy) What Does Medicare Pay For Hospital Stays The exact amount of coverage that medicare provides depends on how long a person. You’re admitted to the hospital as. Medicare doesn't cover 100% of hospital bills. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare pays for the first 60 days of qualifying inpatient hospital stays after. What Does Medicare Pay For Hospital Stays.
From www.healthline.com
How Much Does Medicare Pay for Hospital Stays? What Does Medicare Pay For Hospital Stays Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers the first 60 days of a hospital. What Does Medicare Pay For Hospital Stays.
From www.kff.org
Understanding Medicaid Hospital Payments and the Impact of Recent What Does Medicare Pay For Hospital Stays Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. For days 61 through 90, the beneficiary must pay a daily. The exact amount of coverage that medicare provides depends on how long. What Does Medicare Pay For Hospital Stays.
From www.kff.org
A Primer on Medicare What is Medicare's role in delivery system What Does Medicare Pay For Hospital Stays For days 61 through 90, the beneficiary must pay a daily. You’re admitted to the hospital as. The exact amount of coverage that medicare provides depends on how long a person. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient,. What Does Medicare Pay For Hospital Stays.
From meps.ahrq.gov
STATISTICAL BRIEF 164 Expenses for Hospital Inpatient Stays, 2004 What Does Medicare Pay For Hospital Stays Medicare doesn't cover 100% of hospital bills. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. How much does medicare pay for you to stay in a hospital? For days 61 through 90,. What Does Medicare Pay For Hospital Stays.
From wsj.com
How Medicare Rewards Copious NursingHome Therapy WSJ What Does Medicare Pay For Hospital Stays Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare doesn't cover 100% of hospital bills. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. For days 61. What Does Medicare Pay For Hospital Stays.
From www.usatoday.com
Hospitals terminate Medicare Advantage contracts over payments What Does Medicare Pay For Hospital Stays Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers the first 60 days of a hospital stay after a person. What Does Medicare Pay For Hospital Stays.
From estes.house.gov
Representative Ron Estes What Does Medicare Pay For Hospital Stays After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare doesn't cover 100% of hospital bills. Medicare part. What Does Medicare Pay For Hospital Stays.
From www.medicalnewstoday.com
Medicare and hospital stays Coverage and outofpocket costs What Does Medicare Pay For Hospital Stays You’re admitted to the hospital as. For days 61 through 90, the beneficiary must pay a daily. How much does medicare pay for you to stay in a hospital? Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. After you pay the part a deductible, medicare pays the full cost. What Does Medicare Pay For Hospital Stays.
From www.kff.org
Comparing Private Payer and Medicare Payment Rates for Select Inpatient What Does Medicare Pay For Hospital Stays Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. You’re admitted to the hospital as. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600. What Does Medicare Pay For Hospital Stays.
From www.nytimes.com
Hospitals Stand to Lose Billions Under ‘Medicare for All’ The New What Does Medicare Pay For Hospital Stays How much does medicare pay for you to stay in a hospital? The exact amount of coverage that medicare provides depends on how long a person. For days 61 through 90, the beneficiary must pay a daily. Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. Medicare doesn't cover. What Does Medicare Pay For Hospital Stays.
From www.cms.gov
MLN6922507 Medicare Payment Systems What Does Medicare Pay For Hospital Stays After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare doesn't cover 100% of hospital bills. You’re admitted to the hospital. What Does Medicare Pay For Hospital Stays.
From arnoldmotewealthmanagement.com
Medigap vs Medicare Advantage Comparing Supplemental Insurance Options What Does Medicare Pay For Hospital Stays Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. You’re admitted to the hospital as. Medicare covers the first 60 days of. What Does Medicare Pay For Hospital Stays.
From www.kff.org
A Primer on Medicare How much does Medicare spend, and how does What Does Medicare Pay For Hospital Stays How much does medicare pay for you to stay in a hospital? Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. For days 61 through 90, the beneficiary must pay a daily. Medicare doesn't cover 100% of hospital bills. Medicare pays for the first 60 days of qualifying inpatient hospital stays after. What Does Medicare Pay For Hospital Stays.
From www.nytimes.com
Many Hospitals Charge More Than Twice What Medicare Pays for the Same What Does Medicare Pay For Hospital Stays How much does medicare pay for you to stay in a hospital? The exact amount of coverage that medicare provides depends on how long a person. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: For days 61 through 90, the beneficiary must pay a daily. Medicare covers the first 60 days of. What Does Medicare Pay For Hospital Stays.
From www.cnn.com
What Medicare for all means for doctors and hospitals CNN Politics What Does Medicare Pay For Hospital Stays Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. The exact amount of coverage that medicare provides depends on how long a person. How much does medicare pay for you to stay in a hospital? After you pay the part a deductible, medicare pays the full cost of covered hospital. What Does Medicare Pay For Hospital Stays.
From www.kff.org
An Overview of Medicare KFF What Does Medicare Pay For Hospital Stays For days 61 through 90, the beneficiary must pay a daily. You’re admitted to the hospital as. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means. The exact amount of coverage that medicare provides depends on how long. What Does Medicare Pay For Hospital Stays.
From www.medigap.com
How Medicare Advantage HMO Plans Work What Does Medicare Pay For Hospital Stays Medicare covers hospital stays, but there are limitations on the number of days and you may have to pay coinsurance. For days 61 through 90, the beneficiary must pay a daily. After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient,. What Does Medicare Pay For Hospital Stays.
From www.medicare.org
Does Medicare Cover Bed Sores or Pressure Sores? Medicare & Medicare What Does Medicare Pay For Hospital Stays You’re admitted to the hospital as. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: For days 61 through 90, the beneficiary must pay a daily. The exact amount of coverage that medicare provides. What Does Medicare Pay For Hospital Stays.
From www.caribbeanlife.com
Choosing a Medicare Plan Three key benefits to consider Caribbean Life What Does Medicare Pay For Hospital Stays Medicare part a (hospital insurance) covers inpatient hospital care if you meet both of these conditions: Medicare doesn't cover 100% of hospital bills. The exact amount of coverage that medicare provides depends on how long a person. How much does medicare pay for you to stay in a hospital? Medicare covers hospital stays, but there are limitations on the number. What Does Medicare Pay For Hospital Stays.
From www.ncbi.nlm.nih.gov
Figure 1, Aggregate hospital costs and hospital stays by payer, 2012 What Does Medicare Pay For Hospital Stays Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. Medicare pays for the first 60 days of qualifying inpatient hospital stays after the beneficiary pays their $1,600 deductible. How much does medicare pay for you to stay in a hospital? Medicare doesn't cover 100% of hospital bills. You’re admitted to the hospital. What Does Medicare Pay For Hospital Stays.
From www.kff.org
A Primer on Medicare What does Medicare cover? Sec 4 761504 KFF What Does Medicare Pay For Hospital Stays Medicare covers the first 60 days of a hospital stay after a person has paid their deductible. How much does medicare pay for you to stay in a hospital? After you pay the part a deductible, medicare pays the full cost of covered hospital services for the first 60 days of each benefit period when you’re an inpatient, which means.. What Does Medicare Pay For Hospital Stays.