What Does Soap Stand For In Medical . Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The acronym stands for subjective,. In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. Each letter refers to one of four sections in the document. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers.
from www.peterainsworth.com
Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Exactly what is a soap note?. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. In the soap format, soap stands for subjective, objective, assessment, and plan. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. Each letter refers to one of four sections in the document.
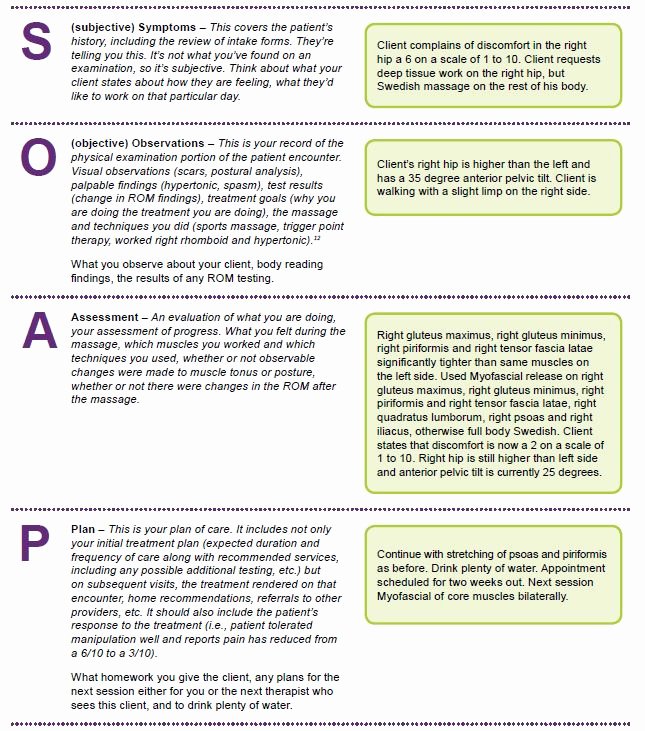
Soap Documentation Example
What Does Soap Stand For In Medical Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Each letter refers to one of four sections in the document. The acronym stands for subjective,. Exactly what is a soap note?. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers.
From www.pinterest.jp
behavioral health soap note Social work exam, School social work What Does Soap Stand For In Medical Soap notes are a standardized method for documenting patient information in healthcare. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The acronym stands for subjective,. Soap notes are a standardized method of documenting. What Does Soap Stand For In Medical.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox What Does Soap Stand For In Medical Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. Exactly what is a soap note?. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. What Does Soap Stand For In Medical.
From ferio.in
Ferio Stainless Steel Single Soap Holder for Bathroom / Soap Stand for What Does Soap Stand For In Medical Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document. What Does Soap Stand For In Medical.
From topanswerideas.com
The Importance of Soap Notes in Well Woman Exams A Comprehensive Guide What Does Soap Stand For In Medical In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient. What Does Soap Stand For In Medical.
From www.powerdiary.com
SOAP Notes for Occupational Therapy OT SOAP Note Examples What Does Soap Stand For In Medical The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for. What Does Soap Stand For In Medical.
From studylib.net
SOAP Notes Format in EMR What Does Soap Stand For In Medical Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. In the soap format, soap stands for subjective, objective, assessment,. What Does Soap Stand For In Medical.
From positivepsychology.com
What are SOAP Notes in Counseling? (+ Examples) What Does Soap Stand For In Medical Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a highly structured format for documenting the progress of. What Does Soap Stand For In Medical.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by What Does Soap Stand For In Medical Each letter refers to one of four sections in the document. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Exactly what is a soap note?. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing. What Does Soap Stand For In Medical.
From study.com
Quiz & Worksheet POVMR & SOAP Record Formats What Does Soap Stand For In Medical Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. Each letter refers to one. What Does Soap Stand For In Medical.
From www.youtube.com
Soap pronunciation and definition YouTube What Does Soap Stand For In Medical In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings.. What Does Soap Stand For In Medical.
From www.theraplatform.com
Occupational therapy SOAP note What Does Soap Stand For In Medical In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a. What Does Soap Stand For In Medical.
From www.studypool.com
SOLUTION Writing soap notes Studypool What Does Soap Stand For In Medical Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. In the soap format, soap stands for subjective, objective, assessment, and. What Does Soap Stand For In Medical.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education What Does Soap Stand For In Medical Each letter refers to one of four sections in the document. Exactly what is a soap note?. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. In the soap format, soap stands for subjective, objective, assessment, and plan. The acronym stands for subjective,. Soap notes are. What Does Soap Stand For In Medical.
From learningcampusdirk.z13.web.core.windows.net
What Does Soap Stand For Notes What Does Soap Stand For In Medical Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Exactly what is a soap note?. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. What Does Soap Stand For In Medical.
From vootmart.com
304 Stainless Steel Chrome Finish Soap Dish Soap Case Soap Holder Soap What Does Soap Stand For In Medical Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. In the soap format, soap. What Does Soap Stand For In Medical.
From www.pinterest.co.uk
SOAPStone Strategy for Written Analysis Analysis, Rhetorical analysis What Does Soap Stand For In Medical The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Exactly what is. What Does Soap Stand For In Medical.
From www.meritech.com
How Does Soap Work? How Soap Works to Remove Germs and Pathogens What Does Soap Stand For In Medical Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. What Does Soap Stand For In Medical.
From swimmingfreestyle.net
30 Medical soap Note Template Example Document Template What Does Soap Stand For In Medical Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are. What Does Soap Stand For In Medical.
From fireflies.ai
10 SOAP Note Templates in 2024 What Does Soap Stand For In Medical The acronym stands for subjective,. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians. What Does Soap Stand For In Medical.
From learningcampusdirk.z13.web.core.windows.net
What Does Soap Stand For Notes What Does Soap Stand For In Medical Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Each letter refers. What Does Soap Stand For In Medical.
From eternalbible.org
What Does Soap Stand For In Bible Study Eternal Bible What Does Soap Stand For In Medical The acronym stands for subjective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a standardized method of documenting patient encounters in. What Does Soap Stand For In Medical.
From aranieco.com
How are soaps different from detergents? Arani Ecosteps What Does Soap Stand For In Medical Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The acronym stands for subjective,. Soap notes are. What Does Soap Stand For In Medical.
From dt4ems.com
SOAP Method Can Keep Staff and Patients Safe DT4EMS What Does Soap Stand For In Medical The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Exactly what is a soap note?.. What Does Soap Stand For In Medical.
From chirotouch.com
Chiropractic SOAP Notes What Does SOAP Stand For? ChiroTouch What Does Soap Stand For In Medical Exactly what is a soap note?. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. In the soap format, soap stands for subjective, objective, assessment, and plan. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a highly structured format for documenting the. What Does Soap Stand For In Medical.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Does Soap Stand For In Medical Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. What Does Soap Stand For In Medical.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide What Does Soap Stand For In Medical Soap notes are a standardized method for documenting patient information in healthcare. In the soap format, soap stands for subjective, objective, assessment, and plan. The acronym stands for subjective,. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are. What Does Soap Stand For In Medical.
From www.youtube.com
What do you mean by "all natural soap"? YouTube What Does Soap Stand For In Medical Soap notes are a standardized method for documenting patient information in healthcare. Each letter refers to one of four sections in the document. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely. What Does Soap Stand For In Medical.
From www.slideshare.net
Nursing Skills Charting What Does Soap Stand For In Medical The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The acronym stands for subjective,. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. What Does Soap Stand For In Medical.
From lesboucans.com
Therapy Progress Note Template Free For Your Needs What Does Soap Stand For In Medical The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Exactly what is a soap note?. The acronym stands for subjective,. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.. What Does Soap Stand For In Medical.
From www.peterainsworth.com
Soap Documentation Example What Does Soap Stand For In Medical Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a standardized method for documenting patient information. What Does Soap Stand For In Medical.
From worksheets.clipart-library.com
Free Printable Blank Hot Process Soap Worksheet The Nova Studio What Does Soap Stand For In Medical Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The acronym stands for subjective,. Exactly what is a soap. What Does Soap Stand For In Medical.
From cleanandhappynest.org
Is it Okay to Dilute Liquid Hand Soap with Water? Cleaning is Caring What Does Soap Stand For In Medical Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The acronym stands for subjective,. Exactly what is a soap note?. Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a highly structured format. What Does Soap Stand For In Medical.
From zolmi.com
How To Write Massage Therapy Soap Notes in 2024 Examples What Does Soap Stand For In Medical Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method for documenting patient information in healthcare.. What Does Soap Stand For In Medical.
From www.etsy.com
SOAP Notes Etsy What Does Soap Stand For In Medical The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The acronym stands for subjective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a standardized method of documenting patient encounters in. What Does Soap Stand For In Medical.
From www.carriedawayministries.com
SOAP Method of Bible study CARRIED AWAY MINISTRIES What Does Soap Stand For In Medical The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. In. What Does Soap Stand For In Medical.