Soap And Nursing . looking for a soap note example nursing students can really use? We’ve got it for you. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. Hear our top tips for. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely.
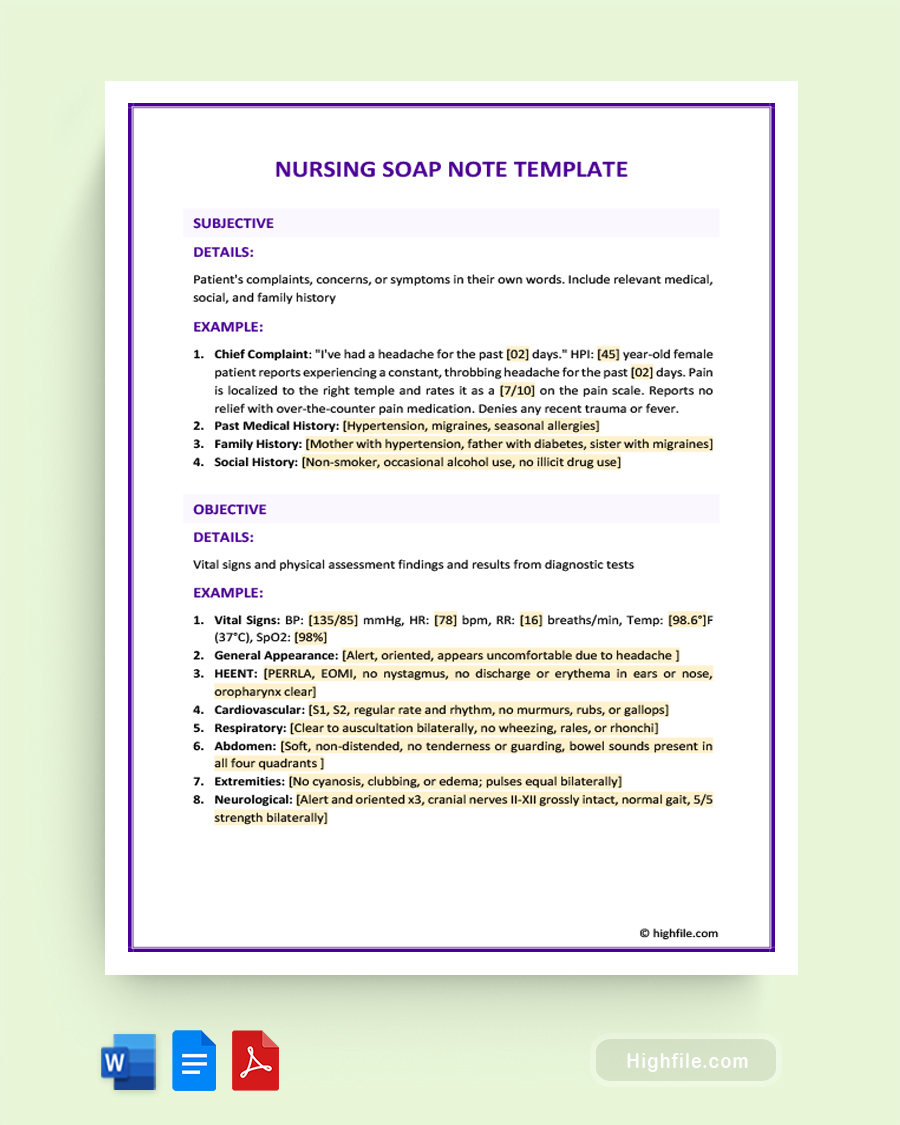
from www.highfile.com
the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. Hear our top tips for. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. looking for a soap note example nursing students can really use? We’ve got it for you. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely.
Nursing SOAP Note Template Word PDF Google Docs Highfile
Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. looking for a soap note example nursing students can really use? We’ve got it for you. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. Hear our top tips for. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse.
From www.pinterest.com.au
progress soap nursing diagnosis Saferbrowser Image Search Results Soap And Nursing the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. We’ve got. Soap And Nursing.
From www.carepatron.com
SOAP Notes for Nursing Template & Example Free PDF Download Soap And Nursing soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Hear our top tips for. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the. Soap And Nursing.
From www.theraplatform.com
Occupational therapy SOAP note Soap And Nursing Hear our top tips for. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. We’ve got it for you. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. looking for a soap note example. Soap And Nursing.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. looking for. Soap And Nursing.
From www.slideshare.net
Nursing Skills Charting Soap And Nursing the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. Hear our top tips for. looking for a soap note example nursing students can really use? it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. We’ve. Soap And Nursing.
From ivypanda.com
Intermittent Headaches Nursing (SOAP) Analysis 911 Words Case Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Hear our top tips for. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. We’ve got it for you. looking. Soap And Nursing.
From viewpoint.online
How to put the patient first in your eye examinations Viewpoint Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. it can be difficult to write. Soap And Nursing.
From www.advantismed.com
How to Master Nurse Charting & Avoid Mistakes Soap And Nursing Hear our top tips for. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. We’ve got it for you. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. the primary purpose of a nursing soap note is to allow clinicians. Soap And Nursing.
From www.highfile.com
Nursing SOAP Note Template Word PDF Google Docs Highfile Soap And Nursing looking for a soap note example nursing students can really use? the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. soap—or subjective, objective, assessment. Soap And Nursing.
From enfermagem4you.pt
Significado do SOAP na enfermagem uma abordagem prática Enfermagem 4You Soap And Nursing it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. looking for a soap note example nursing students can really use? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. We’ve got it for you. the primary purpose of a nursing. Soap And Nursing.
From professionalwritingservices.in
How to Write SOP For Nursing Best Guidelines & Samples Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. We’ve got it for you. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the primary. Soap And Nursing.
From www.slideserve.com
PPT Communication of the Nursing Process Documentation PowerPoint Soap And Nursing soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. looking for a soap note example nursing students can really use? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the soapie charting method is a commonly used template for nursing notes that can be very. Soap And Nursing.
From nursingwritingservice.com
Greenish discharge from left breast soap noteBest Nursing Writing Soap And Nursing it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. looking. Soap And Nursing.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners, Physician Soap And Nursing it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. looking for a soap note example nursing students can really use? Hear our top tips for. the soapie charting method is a. Soap And Nursing.
From quizzmediasophie.z13.web.core.windows.net
The E Entry In The Soaper Charting Method Means Soap And Nursing the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. looking for a soap note example nursing students can really use? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the subjective, objective, assessment and plan (soap) note is an acronym. Soap And Nursing.
From nursingschoolofsuccess.com
SOAP Note Example Nursing SOAP Note Nursing School of Success Soap And Nursing Hear our top tips for. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. looking for a soap note example. Soap And Nursing.
From studycorgi.com
SOAP (Nursing) Note on Dyspnea, Confusion, and Fatigue Free Essay Example Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. We’ve got it for you. Hear our top tips for. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. it can be difficult to write a nursing note in an organized and detailed manner, and there are. Soap And Nursing.
From www.pinterest.com
SOAP Notes Etsy in 2021 Soap note, Nursing notes, Marriage and Soap And Nursing We’ve got it for you. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Hear our top tips for. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. soap notes are a standardized method of documenting patient encounters in medical and. Soap And Nursing.
From www.pinterest.es
SOAP vs SBAR Nursing School Studying, Nursing School Notes, Medical Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the primary purpose of a nursing soap. Soap And Nursing.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap And Nursing soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Hear our top tips for. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. . Soap And Nursing.
From www.studocu.com
SOAP Note and FULL Nursing Care Plan for L&D clinical. Newborn pt Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. We’ve got it for you. the soapie charting method is a. Soap And Nursing.
From studylib.net
Patient SOAP Note Charting Procedures Soap And Nursing We’ve got it for you. looking for a soap note example nursing students can really use? soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the subjective, objective, assessment and plan (soap) note is an acronym. Soap And Nursing.
From medium.com
Improve Patient Care The Importance of Accurate Nursing SOAP Notes Soap And Nursing Hear our top tips for. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. soap notes are a standardized method of documenting patient encounters in medical. Soap And Nursing.
From www.pinterest.com
Soap Note Etsy Soap note, Medical school essentials, Medical school Soap And Nursing soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the soapie charting method is a commonly used template for nursing. Soap And Nursing.
From medicalaid.org
Understanding SOAP Notes for Clinical Rotations International Medical Aid Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Hear our top tips for. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. soap—or. Soap And Nursing.
From npchartingschool.com
Examples of a SOAP note plus 7 tips for charting! Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. looking for a soap note example nursing students can really use? Hear our top tips for. it can be difficult to write a nursing note in an. Soap And Nursing.
From carstens.com
Best Practices for SOAP Notes in Nursing Carstens Soap And Nursing soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. Hear our top tips for. We’ve got it for you. the subjective, objective, assessment and plan (soap) note is an acronym representing. Soap And Nursing.
From www.etsy.com
Nurse Soap Nurse Appreciation Soap Set Lotion Bar CNA Doctor Etsy Soap And Nursing it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. Hear. Soap And Nursing.
From www.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract Soap And Nursing the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. looking for a soap note example nursing students can really use? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Hear our top tips for. the subjective, objective, assessment. Soap And Nursing.
From www.pinterest.com
Nursing SOAP Note Example Nursing notes, Medical prescription, Soap note Soap And Nursing the primary purpose of a nursing soap note is to allow clinicians to document patient encounters in a continuous, structured way. We’ve got it for you. Hear our top tips for. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. the subjective, objective, assessment and plan (soap) note is an acronym. Soap And Nursing.
From www.dreamstime.com
The Doctor Washes His Hands with Soap before Starting the Operation Soap And Nursing soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. looking for a soap note example nursing students can really use? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. it can be difficult to write a nursing note in an organized and detailed manner,. Soap And Nursing.
From nursingresearchhelp.com
Best Nursing SOAP notes writing guide Nursing Research Help Soap And Nursing it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Hear our top tips for. looking for a soap note example nursing students can really use? the primary purpose of a nursing. Soap And Nursing.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap And Nursing the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. We’ve got it for you. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the. Soap And Nursing.
From dt4ems.com
SOAP Method Can Keep Staff and Patients Safe DT4EMS Soap And Nursing it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Hear our top tips for. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes. Soap And Nursing.
From www.flickr.com
The Role of SOAP Notes in Nursing Practice The SOAP note i… Flickr Soap And Nursing soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. the soapie charting method is a commonly used template for nursing notes that can be very helpful for any nurse. it can be difficult to write a nursing note in an organized and detailed manner, and there are several strategies. the. Soap And Nursing.