Soap Acronym Examples . Avoid common soap note mistakes; — soap notes for social workers. Here’s an overview of how to write progress notes. you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Lawrence weed in the 1960s in order. They contain four primary sections, represented by its. Soap notes, a communication tool used for presenting information between. Now that you have a soap notes template and know about the common soap note mistakes to look out. — exactly what is a soap note? It is the documentation used to record information. soap nursing notes are a type of patient progress note or nurse’s note. The soap acronym stands for. — in a previous post, we reviewed the necessity of basic best practices for soap notes including. soap note examples and templates.
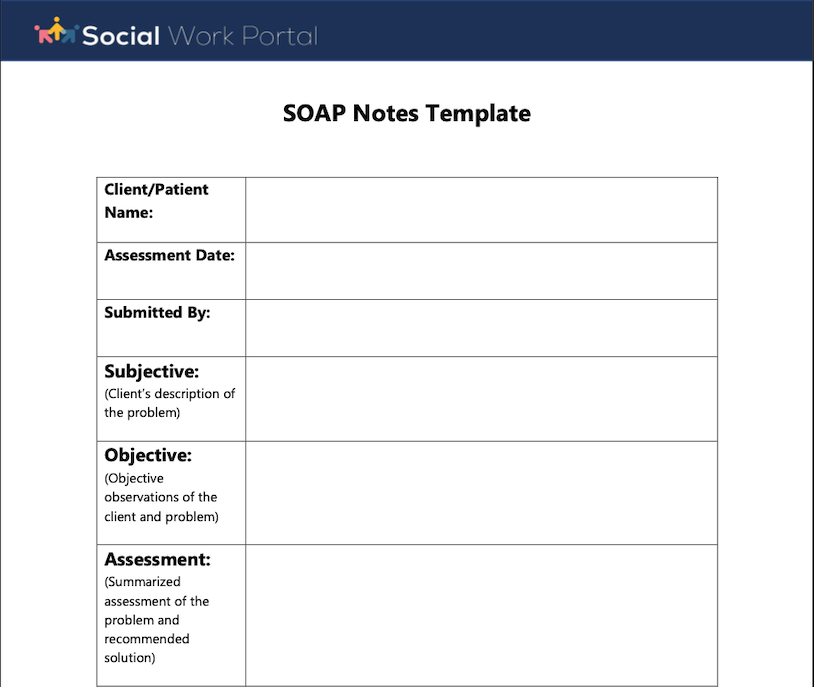
from www.socialworkportal.com
— the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. In social work, soap notes are essential for recording client sessions,. — among the various methods available, soap notes stand out as a standardized and highly effective. soap nursing notes are a type of patient progress note or nurse’s note. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Here’s an overview of how to write progress notes. Lawrence weed in the 1960s in order. During the first part of the. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation.
How to Write a Social Work Soap Assessment Best Guide to Soap
Soap Acronym Examples soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. — exactly what is a soap note? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Soap notes, a communication tool used for presenting information between. They contain four primary sections, represented by its. Now that you have a soap notes template and know about the common soap note mistakes to look out. — to begin, the acronym soap stands for the following components: — among the various methods available, soap notes stand out as a standardized and highly effective. — documenting a patient assessment in the notes is something all medical students need to practice. soap note examples and templates. soap notes are a specific format for writing progress notes as a behavioral health clinician. — while documenting progress notes is an important aspect of being a behavioral health care professional, it’s. — tips for writing soap notes. soap nursing notes are a type of patient progress note or nurse’s note. — what is a soap note (with examples) how to write a soap note;
From dxopzvjow.blob.core.windows.net
Soap Unexpected Element Found at Scott Haggins blog Soap Acronym Examples — documenting a patient assessment in the notes is something all medical students need to practice. They contain four primary sections, represented by its. — while documenting progress notes is an important aspect of being a behavioral health care professional, it’s. — in a previous post, we reviewed the necessity of basic best practices for soap notes. Soap Acronym Examples.
From dxoshcfag.blob.core.windows.net
Soap Example Request at Nadia Morris blog Soap Acronym Examples Avoid common soap note mistakes; — to begin, the acronym soap stands for the following components: It is the documentation used to record information. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap note examples and templates. — documenting a patient assessment. Soap Acronym Examples.
From gioceabax.blob.core.windows.net
Java Soap Message Example at June Brann blog Soap Acronym Examples soap notes are a specific format for writing progress notes as a behavioral health clinician. — documenting a patient assessment in the notes is something all medical students need to practice. — soap notes for social workers. Now that you have a soap notes template and know about the common soap note mistakes to look out. The. Soap Acronym Examples.
From www.advantismed.com
How to Master Nurse Charting & Avoid Mistakes Soap Acronym Examples The soap acronym stands for. In social work, soap notes are essential for recording client sessions,. It is the documentation used to record information. During the first part of the. — documenting a patient assessment in the notes is something all medical students need to practice. — while documenting progress notes is an important aspect of being a. Soap Acronym Examples.
From gioceabax.blob.core.windows.net
Java Soap Message Example at June Brann blog Soap Acronym Examples Avoid common soap note mistakes; This guide discusses the soap. — to begin, the acronym soap stands for the following components: They contain four primary sections, represented by its. — documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a specific format for writing progress notes as a. Soap Acronym Examples.
From www.shutterstock.com
Soap Simple Object Access Protocol Acronym Stock Vector (Royalty Free Soap Acronym Examples you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes, a communication tool used for presenting information between. — in a previous post, we reviewed the necessity of. Soap Acronym Examples.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Acronym Examples the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Avoid common soap note mistakes; Now that you have a soap notes template and know about the common soap note mistakes to look out. During the first part of the. — the subjective, objective, assessment and plan (soap) note. Soap Acronym Examples.
From www.eslprintables.com
English worksheets SOAPS Acronym Soap Acronym Examples The soap acronym stands for. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — exactly what is a soap note? a soap note is a structured method used for documenting a patient's medical information during a therapy session. the soap note (an. Soap Acronym Examples.
From www.theraplatform.com
Occupational therapy SOAP note Soap Acronym Examples — writing soap notes properly is crucial in healthcare as they provide a structured way to document patient. — tips for writing soap notes. — documenting a patient assessment in the notes is something all medical students need to practice. — to begin, the acronym soap stands for the following components: This guide discusses the soap.. Soap Acronym Examples.
From www.carriedawayministries.com
SOAP Method of Bible study CARRIED AWAY MINISTRIES Soap Acronym Examples Soap notes, a communication tool used for presenting information between. — soap notes for social workers. a soap note is a structured method used for documenting a patient's medical information during a therapy session. — tips for writing soap notes. — writing soap notes properly is crucial in healthcare as they provide a structured way to. Soap Acronym Examples.
From www.studocu.com
3.5 SOAP Format notes Key terms Master problem list first page of Soap Acronym Examples Soap notes, a communication tool used for presenting information between. — soap notes for social workers. They contain four primary sections, represented by its. — among the various methods available, soap notes stand out as a standardized and highly effective. In social work, soap notes are essential for recording client sessions,. Here’s an overview of how to write. Soap Acronym Examples.
From dxowyombv.blob.core.windows.net
Sample Medical Acronym at Theodore Cox blog Soap Acronym Examples — to begin, the acronym soap stands for the following components: — tips for writing soap notes. Avoid common soap note mistakes; Soap notes, a communication tool used for presenting information between. Now that you have a soap notes template and know about the common soap note mistakes to look out. — the subjective, objective, assessment and. Soap Acronym Examples.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Acronym Examples — to begin, the acronym soap stands for the following components: — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. They contain four primary sections, represented by its. . Soap Acronym Examples.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Acronym Examples — tips for writing soap notes. Soap notes, a communication tool used for presenting information between. During the first part of the. They contain four primary sections, represented by its. — while documenting progress notes is an important aspect of being a behavioral health care professional, it’s. In social work, soap notes are essential for recording client sessions,.. Soap Acronym Examples.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide Soap Acronym Examples soap, an acronym (meaning subjective objective assessment plan) was coined by dr. you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. The soap acronym stands for. a soap note is a structured method used for documenting a patient's medical information during a therapy session. In social work, soap. Soap Acronym Examples.
From www.carepatron.com
SOAP Notes for Chiropractic Template & Example Free PDF Download Soap Acronym Examples — writing soap notes properly is crucial in healthcare as they provide a structured way to document patient. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap nursing notes are a type of patient progress note or nurse’s note. soap note examples and templates. — what is. Soap Acronym Examples.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Acronym Examples the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. Soap notes, a communication tool used for presenting information between. — what is a soap note (with examples) how to. Soap Acronym Examples.
From dxocgzpbf.blob.core.windows.net
Soaps Definition Ap Lang at Terry Fanelli blog Soap Acronym Examples Lawrence weed in the 1960s in order. — writing soap notes properly is crucial in healthcare as they provide a structured way to document patient. — exactly what is a soap note? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — among the various methods available, soap notes. Soap Acronym Examples.
From printable.conaresvirtual.edu.sv
Soap Bible Study Method Free Printable Soap Acronym Examples soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — soap notes for social workers. a soap note is a structured method used for documenting a patient's medical information during a therapy session. Lawrence weed in the 1960s in order. — exactly what. Soap Acronym Examples.
From hxellffvu.blob.core.windows.net
Soap Objective at Wanda Melin blog Soap Acronym Examples — what is a soap note (with examples) how to write a soap note; you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. It is the documentation used to record information. — while documenting progress notes is an important aspect of being a behavioral health care professional, it’s.. Soap Acronym Examples.
From aliciawatts.z13.web.core.windows.net
Soap Chart Note Is An Acronym For Soap Acronym Examples — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its. Soap notes, a communication tool used for presenting information between. soap notes are a specific format for. Soap Acronym Examples.
From dxokzuxuc.blob.core.windows.net
Soap Chart Meaning at Kevin Stoddard blog Soap Acronym Examples Avoid common soap note mistakes; Soap notes, a communication tool used for presenting information between. This guide discusses the soap. — documenting a patient assessment in the notes is something all medical students need to practice. soap nursing notes are a type of patient progress note or nurse’s note. — among the various methods available, soap notes. Soap Acronym Examples.
From www.worthbeyondrubies.com
Learn The Simple 4 Step SOAP Bible Study Method Today Soap Acronym Examples soap notes are a specific format for writing progress notes as a behavioral health clinician. — documenting a patient assessment in the notes is something all medical students need to practice. It is the documentation used to record information. The soap acronym stands for. soap notes are a highly structured format for documenting the progress of a. Soap Acronym Examples.
From template.mapadapalavra.ba.gov.br
Psychiatry Soap Note Template Soap Acronym Examples — documenting a patient assessment in the notes is something all medical students need to practice. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. It is the documentation used to record information. learn how to write a soap note so you can efficiently track, assess, diagnose,. Soap Acronym Examples.
From dxobwnfgw.blob.core.windows.net
Soap Biblical Acronym at Mark Hicks blog Soap Acronym Examples you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. soap notes are a specific format for writing progress notes as a behavioral health clinician. — writing soap notes properly is crucial in healthcare as they provide a structured way to document patient. Here’s an overview of how to. Soap Acronym Examples.
From nurseship.com
OLD CARTS Acronym (Explained W/ Questions) Soap Acronym Examples the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Lawrence weed in the 1960s in order. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. It is the documentation used to record information. soap, an acronym (meaning subjective objective assessment. Soap Acronym Examples.
From dxorhmyma.blob.core.windows.net
What Is A Soap In Medical Terms at Gretchen Price blog Soap Acronym Examples During the first part of the. — while documenting progress notes is an important aspect of being a behavioral health care professional, it’s. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap note examples and templates. In social work, soap notes are essential for recording client sessions,. Avoid common soap. Soap Acronym Examples.
From hxemxurna.blob.core.windows.net
What Is Objective In Soap at Milagros Jackson blog Soap Acronym Examples soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap acronym stands for. soap, an acronym (meaning subjective objective assessment plan) was coined by dr. — writing soap notes properly is crucial in healthcare as they provide a structured way to document patient. soap note examples and templates. . Soap Acronym Examples.
From hxecfsicg.blob.core.windows.net
Soap Acronym Api at Maria Dixon blog Soap Acronym Examples soap, an acronym (meaning subjective objective assessment plan) was coined by dr. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. you probably already know this, but soap is an acronym that stands for subjective, objective, assessment, and plan. Here’s an overview of how. Soap Acronym Examples.
From www.youtube.com
Acronyms and Mnemonics PART 2 by NURSES EXAM or Nursing Support news Soap Acronym Examples the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Avoid common soap note mistakes; soap note examples and templates. Here’s an overview of how to write progress notes. Now that you have a soap notes template and know about the common soap note mistakes to look out. . Soap Acronym Examples.
From www.studocu.com
Comprehensive SOAP Template Comprehensive SOAP Template Patient Soap Acronym Examples a soap note is a structured method used for documenting a patient's medical information during a therapy session. — writing soap notes properly is crucial in healthcare as they provide a structured way to document patient. It is the documentation used to record information. — what is a soap note (with examples) how to write a soap. Soap Acronym Examples.
From abetterwaytohomeschool.com
Inductive Bible Study Prayer for Kid SOAP Acronym A Better Way to Soap Acronym Examples Lawrence weed in the 1960s in order. — soap notes for social workers. soap nursing notes are a type of patient progress note or nurse’s note. — tips for writing soap notes. soap, an acronym (meaning subjective objective assessment plan) was coined by dr. the soap note (an acronym for subjective, objective, assessment, and plan). Soap Acronym Examples.
From www.realiaproject.org
11+ SOAP Note Example FREE Download [Word, PDF] Soap Acronym Examples — in a previous post, we reviewed the necessity of basic best practices for soap notes including. Now that you have a soap notes template and know about the common soap note mistakes to look out. Lawrence weed in the 1960s in order. Here’s an overview of how to write progress notes. In social work, soap notes are essential. Soap Acronym Examples.
From hxecfsicg.blob.core.windows.net
Soap Acronym Api at Maria Dixon blog Soap Acronym Examples — while documenting progress notes is an important aspect of being a behavioral health care professional, it’s. a soap note is a structured method used for documenting a patient's medical information during a therapy session. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many.. Soap Acronym Examples.
From hxemxurna.blob.core.windows.net
What Is Objective In Soap at Milagros Jackson blog Soap Acronym Examples — soap notes for social workers. The soap acronym stands for. — exactly what is a soap note? learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap, an acronym (meaning subjective objective assessment plan) was coined by dr. This guide discusses the soap. Now that you have. Soap Acronym Examples.