Does Unicare Require Prior Authorization . In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. You can also refer to. The medical code (s) listed. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. The process of giving a member’s treating, ordering, or. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). All prior authorization requests will be available for viewing on availity essentials. After hours, verify member eligibility by. Use the prior authorization tool within availity.
from www.jindalhc.com
Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. You can also refer to. After hours, verify member eligibility by. The medical code (s) listed. The process of giving a member’s treating, ordering, or. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. All prior authorization requests will be available for viewing on availity essentials. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements.
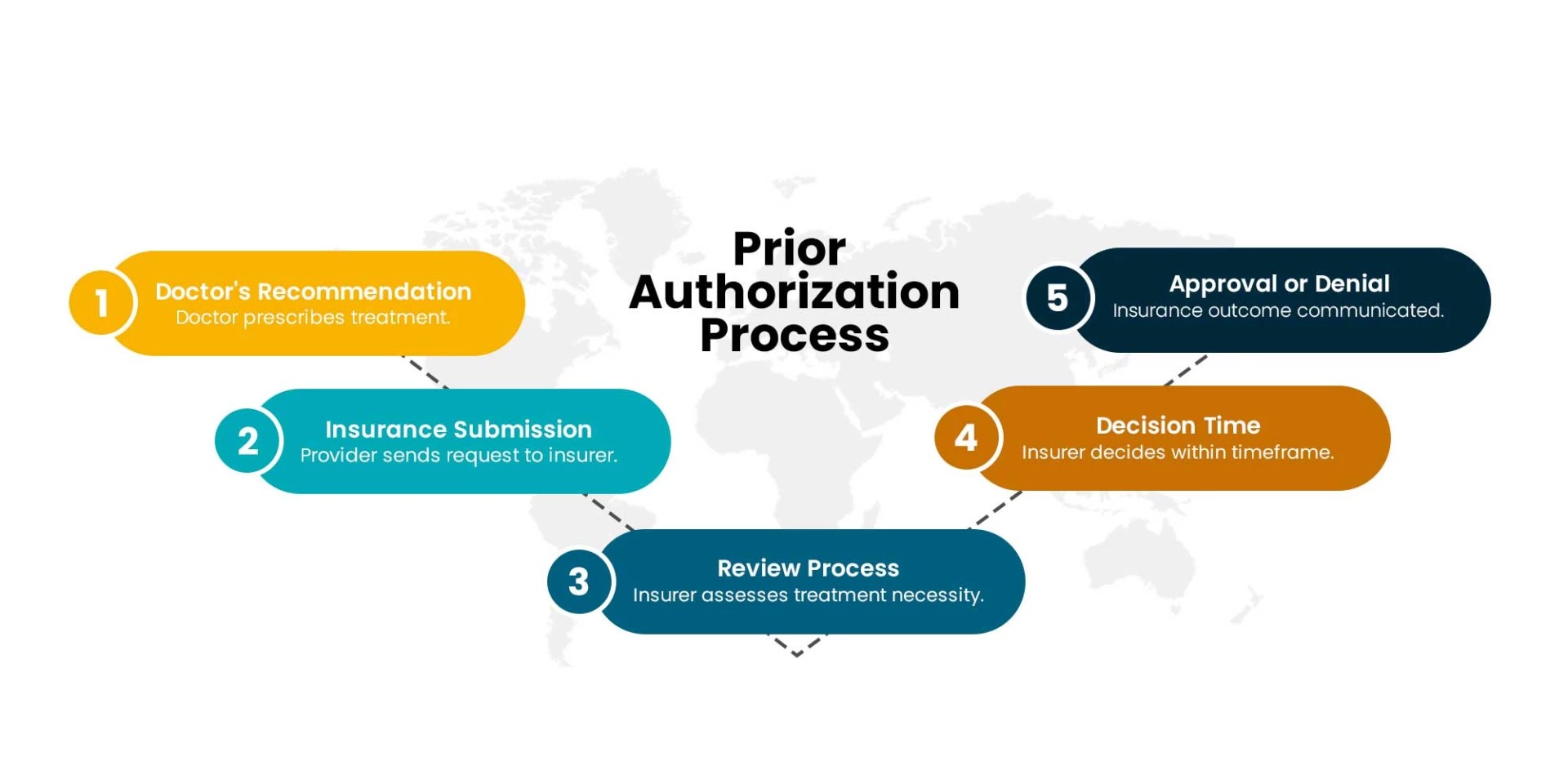
A Complete Overview of Prior Authorization Process
Does Unicare Require Prior Authorization Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. You can also refer to. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). All prior authorization requests will be available for viewing on availity essentials. Use the prior authorization tool within availity. The medical code (s) listed. After hours, verify member eligibility by. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. The process of giving a member’s treating, ordering, or.
From loezgfkio.blob.core.windows.net
Does Unicare Require Prior Authorization at Samantha Doyle blog Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and. Does Unicare Require Prior Authorization.
From www.redoxengine.com
Fixing prior authorization Redox Does Unicare Require Prior Authorization Use the prior authorization tool within availity. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. You can also refer to. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. After hours,. Does Unicare Require Prior Authorization.
From gerriebleonanie.pages.dev
Mmo Prior Auth List 2024 Edita Marketa Does Unicare Require Prior Authorization Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. The process of giving a member’s. Does Unicare Require Prior Authorization.
From loezgfkio.blob.core.windows.net
Does Unicare Require Prior Authorization at Samantha Doyle blog Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. After hours, verify member eligibility by. You can also. Does Unicare Require Prior Authorization.
From www.pdffiller.com
Fillable Online Standardized Prior Authorization Form to Does Unicare Require Prior Authorization Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. The medical code (s) listed. You can also refer to. After hours, verify member eligibility by. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. The. Does Unicare Require Prior Authorization.
From www.planforms.net
Prior Authorization Requests Form Keen Transport Printable Pdf Download Does Unicare Require Prior Authorization The medical code (s) listed. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Effective july 1, 2023, prior authorization (pa) requirements will change for the. Does Unicare Require Prior Authorization.
From valer.health
Prior Authorization Valer Does Unicare Require Prior Authorization Use the prior authorization tool within availity. All prior authorization requests will be available for viewing on availity essentials. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. You can also refer to. The medical code (s) listed. In most cases, your doctor will provide unicare with the information necessary to get services. Does Unicare Require Prior Authorization.
From staffingly.com
Outsourcing Prior Authorization Process An Approach to Optimizing Your Does Unicare Require Prior Authorization Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. All prior authorization requests will be available for viewing on availity essentials. Use the prior authorization tool within availity. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). The process of. Does Unicare Require Prior Authorization.
From akasa.com
How To Speed Up Your Prior Authorization Workflow AKASA Does Unicare Require Prior Authorization In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. The process of giving a member’s treating, ordering, or. After hours, verify member eligibility. Does Unicare Require Prior Authorization.
From www.myndshft.com
The Ultimate Guide to Prior Authorization Myndshft Does Unicare Require Prior Authorization After hours, verify member eligibility by. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. Use the prior authorization tool within availity. You can also refer to. All prior authorization requests will be available for viewing on availity essentials. In most cases, your doctor will provide unicare with the information necessary to get. Does Unicare Require Prior Authorization.
From www.pollockcohen.com
Prior Authorization Investigation Pollock Cohen LLP Does Unicare Require Prior Authorization The medical code (s) listed. Use the prior authorization tool within availity. The process of giving a member’s treating, ordering, or. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. All prior authorization requests will be available for viewing on availity essentials. Unicare’s prior authorization lookup tool online (pluto). Does Unicare Require Prior Authorization.
From www.jindalhc.com
A Complete Overview of Prior Authorization Process Does Unicare Require Prior Authorization In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. You can also refer to. After hours, verify member eligibility by. Use the prior authorization tool within availity. All prior authorization requests will be available for viewing on availity essentials. The medical code (s) listed. Unicare’s prior. Does Unicare Require Prior Authorization.
From chronicdiseasecoalition.org
Prior Authorization and the Patient Experience Insights from a… Does Unicare Require Prior Authorization All prior authorization requests will be available for viewing on availity essentials. Use the prior authorization tool within availity. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. You can also refer to. The medical code (s) listed. Effective july 1, 2024, all prior authorization (pa). Does Unicare Require Prior Authorization.
From www.keyscriptsllc.com
The Power of Prior Authorization KeyScripts, LLC Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. You can also refer to. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Prior authorization means that a health provider needs to get approval from. Does Unicare Require Prior Authorization.
From medicare-faqs.com
How To Do A Prior Authorization For Medicare Does Unicare Require Prior Authorization All prior authorization requests will be available for viewing on availity essentials. You can also refer to. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Effective july 1, 2024, all. Does Unicare Require Prior Authorization.
From themedicarefamily.com
Does Medicare Require Prior Authorization? Does Unicare Require Prior Authorization You can also refer to. Use the prior authorization tool within availity. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. After hours, verify member eligibility by. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do. Does Unicare Require Prior Authorization.
From vativorx.com
What is prior authorization and how does the process work? VativoRx Does Unicare Require Prior Authorization You can also refer to. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. After hours, verify member eligibility by. All prior authorization requests will be available for viewing on. Does Unicare Require Prior Authorization.
From www.planforms.net
Unicare Health Plan Of Wv Prior Authorization Form Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Use the prior authorization tool within availity. You can also refer to. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. All prior authorization requests will be available for viewing on availity essentials.. Does Unicare Require Prior Authorization.
From loezgfkio.blob.core.windows.net
Does Unicare Require Prior Authorization at Samantha Doyle blog Does Unicare Require Prior Authorization The medical code (s) listed. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). All prior authorization requests will be available for viewing on availity essentials. You can also refer to. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. The process of giving a member’s treating,. Does Unicare Require Prior Authorization.
From www.hrrmc.com
Insurance Prior Authorization Timeframes Medical Center in Salida Does Unicare Require Prior Authorization All prior authorization requests will be available for viewing on availity essentials. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). After hours, verify member eligibility by. You can also refer to. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. In most. Does Unicare Require Prior Authorization.
From www.psychiatryatlanta.com
What is Prior Authorization? Some Mysteries Explained Atlanta Does Unicare Require Prior Authorization The medical code (s) listed. All prior authorization requests will be available for viewing on availity essentials. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. Use the prior authorization tool within availity. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). Prior authorization means that a. Does Unicare Require Prior Authorization.
From nanthealth.com
CMS Finalizes Revolutionary Prior Authorization Rule NantHealth Does Unicare Require Prior Authorization Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. All prior authorization requests will be available for viewing on availity essentials. You can also refer to. The medical code (s) listed. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment,. Does Unicare Require Prior Authorization.
From www.planforms.net
Does Medicare Require Prior Authorization For Ct Scans Ct Scan Machine Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). The medical code (s) listed. After hours, verify member eligibility by. Prior authorization means that a health provider needs to get approval from a patient's. Does Unicare Require Prior Authorization.
From www.allzonems.com
Prior Authorization Process Streamlined by CMS Does Unicare Require Prior Authorization Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. All prior authorization requests will be available for viewing on availity essentials. Use the prior authorization tool within availity. The medical code (s) listed. In most cases, your doctor will provide unicare with the information necessary to. Does Unicare Require Prior Authorization.
From getreferralmd.com
The Shocking Truth about Prior Authorizations in Healthcare Does Unicare Require Prior Authorization You can also refer to. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. After. Does Unicare Require Prior Authorization.
From staffingly.com
PRIOR AUTHORIZATION PROCESS Staffingly, Inc Does Unicare Require Prior Authorization After hours, verify member eligibility by. You can also refer to. Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. All prior authorization requests will be available for viewing on availity essentials. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a. Does Unicare Require Prior Authorization.
From practolytics.com
3 Ways to Improve Prior Authorization Services for Your Practice Does Unicare Require Prior Authorization Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. You can also refer to. Effective july 1, 2023, prior authorization (pa) requirements will change for the. Does Unicare Require Prior Authorization.
From medicare-faqs.com
How Do I Submit A Prior Authorization To Medicare? Does Unicare Require Prior Authorization After hours, verify member eligibility by. Prior authorization means that a health provider needs to get approval from a patient's health plan before moving ahead with a treatment, procedure,. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Unicare’s prior authorization lookup tool online (pluto) can assist with determining. Does Unicare Require Prior Authorization.
From www.pdffiller.com
Fillable Online Unicare wv medicaid prior authorization form Fax Email Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. All prior authorization requests will be available for viewing on availity essentials. The process of giving a. Does Unicare Require Prior Authorization.
From loezgfkio.blob.core.windows.net
Does Unicare Require Prior Authorization at Samantha Doyle blog Does Unicare Require Prior Authorization Unicare’s prior authorization lookup tool online (pluto) can assist with determining a code’s prior authorization requirements. All prior authorization requests will be available for viewing on availity essentials. After hours, verify member eligibility by. The medical code (s) listed. The process of giving a member’s treating, ordering, or. Effective july 1, 2023, prior authorization (pa) requirements will change for the. Does Unicare Require Prior Authorization.
From eforms.com
Free Medicare Prior (Rx) Authorization Form PDF eForms Does Unicare Require Prior Authorization The medical code (s) listed. All prior authorization requests will be available for viewing on availity essentials. You can also refer to. The process of giving a member’s treating, ordering, or. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. In most cases, your doctor will provide unicare with. Does Unicare Require Prior Authorization.
From www.signnow.com
Massachusetts Standard Prior Authorization 20162024 Form Fill Out Does Unicare Require Prior Authorization Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. After hours, verify member eligibility by. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Use the prior authorization tool within availity. Effective july 1, 2023,. Does Unicare Require Prior Authorization.
From www.thesuperbill.com
All You Need to Know About Prior Authorization — SuperBill Does Unicare Require Prior Authorization The medical code (s) listed. All prior authorization requests will be available for viewing on availity essentials. You can also refer to. After hours, verify member eligibility by. The process of giving a member’s treating, ordering, or. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything.. Does Unicare Require Prior Authorization.
From www.planforms.net
Unicare Health Plan Of Wv Prior Authorization Form Does Unicare Require Prior Authorization Use the prior authorization tool within availity. In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. The process of giving a member’s treating, ordering, or. Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. Effective. Does Unicare Require Prior Authorization.
From medleedshcs.com
Prior Authorization Complete analysis of regulations Does Unicare Require Prior Authorization In most cases, your doctor will provide unicare with the information necessary to get services preapproved and you won’t need to do anything. Effective july 1, 2023, prior authorization (pa) requirements will change for the following code (s). Effective july 1, 2024, all prior authorization (pa) requests must be submitted via the mco portal, interactive care reviewer (icr),. You can. Does Unicare Require Prior Authorization.