Aetna Medicare Specialty Pharmacy Prior Authorization Form . They will look at your overall health or any. This form is for use only where a. † use a separate claim form for each patient. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. Required clinical information must be completed in its entirety for all precertification requests. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Specialty drug prior authorization requests. All fields on this form are required. Has the patient been receiving the requested drug within the last 120 days? In some plans, you might need prior authorization for the place where you get a. Please attach all clinical information. † claims must be submitted within two years of date of purchase. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. This guide includes lists of the services and medicines that need prior authorization.
from www.pdffiller.com
† use a separate claim form for each patient. Please attach all clinical information. This form is for use only where a. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. † claims must be submitted within two years of date of purchase. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Specialty drug prior authorization requests. Has the patient been receiving the requested drug within the last 120 days? This guide includes lists of the services and medicines that need prior authorization. All fields on this form are required.
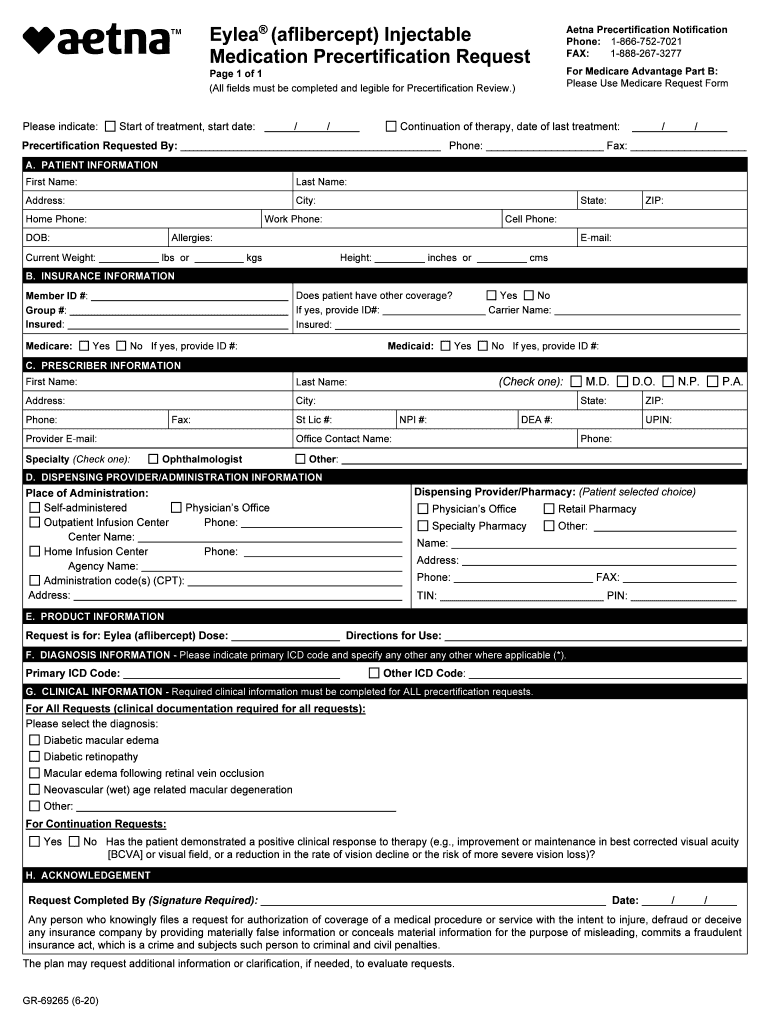
2020 Form Aetna GR69265 Fill Online, Printable, Fillable, Blank
Aetna Medicare Specialty Pharmacy Prior Authorization Form Required clinical information must be completed in its entirety for all precertification requests. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Specialty drug prior authorization requests. This form is for use only where a. All fields on this form are required. They will look at your overall health or any. Has the patient been receiving the requested drug within the last 120 days? To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. In some plans, you might need prior authorization for the place where you get a. Please attach all clinical information. This guide includes lists of the services and medicines that need prior authorization. † claims must be submitted within two years of date of purchase. Required clinical information must be completed in its entirety for all precertification requests. † use a separate claim form for each patient.
From www.uslegalforms.com
KY Aetna Pharmacy Prior Authorization Request Form Fill and Sign Aetna Medicare Specialty Pharmacy Prior Authorization Form Required clinical information must be completed in its entirety for all precertification requests. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. This form is for use only where. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Pharmacy Prior Authorization Request Form Fax Email Aetna Medicare Specialty Pharmacy Prior Authorization Form They will look at your overall health or any. Please attach all clinical information. This guide includes lists of the services and medicines that need prior authorization. † claims must be submitted within two years of date of purchase. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. In some plans,. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From formspal.com
Aetna Pharmacy Prior Authorization PDF Form FormsPal Aetna Medicare Specialty Pharmacy Prior Authorization Form In some plans, you might need prior authorization for the place where you get a. † claims must be submitted within two years of date of purchase. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Please attach all clinical information. Has the patient been receiving the requested drug within the last. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Aetna Specialty Pharmacy Prior Authorization Form Fax Aetna Medicare Specialty Pharmacy Prior Authorization Form Please attach all clinical information. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. † claims must be submitted within two years of date of purchase. All fields on this form are required. Has the patient been receiving the requested drug within the last 120 days? This. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
2020 Form Aetna GR69265 Fill Online, Printable, Fillable, Blank Aetna Medicare Specialty Pharmacy Prior Authorization Form For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. This form is for use only where a. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. To get prior authorization, your doctor must first submit a request for a. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.contrapositionmagazine.com
Aetna Medicare Prior Auth Form For Medication Form Resume Examples Aetna Medicare Specialty Pharmacy Prior Authorization Form This guide includes lists of the services and medicines that need prior authorization. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. † use a separate claim form for each patient. All fields on this form are required. To get prior authorization, your doctor must first submit a request for a specific. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From eforms.com
Free Medicare Prior (Rx) Authorization Form PDF eForms Aetna Medicare Specialty Pharmacy Prior Authorization Form All fields on this form are required. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. This form is for use only where a. In some plans, you might need prior authorization for the place where you get a. They will look at your overall health or any. For part d prior. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From fill.io
Fill Free fillable Aetna Better Health PDF forms Aetna Medicare Specialty Pharmacy Prior Authorization Form Specialty drug prior authorization requests. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. This form is for use only where a. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. All fields on this form are required. To. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From lorneqchristyna.pages.dev
Aetna Prior Authorization List 2024 Poppy Cariotta Aetna Medicare Specialty Pharmacy Prior Authorization Form Required clinical information must be completed in its entirety for all precertification requests. All fields on this form are required. Specialty drug prior authorization requests. In some plans, you might need prior authorization for the place where you get a. This form is for use only where a. Has the requested drug been dispensed at a pharmacy and approved for. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From lorneqchristyna.pages.dev
Aetna Prior Authorization List 2024 Poppy Cariotta Aetna Medicare Specialty Pharmacy Prior Authorization Form This guide includes lists of the services and medicines that need prior authorization. This form is for use only where a. Please attach all clinical information. Required clinical information must be completed in its entirety for all precertification requests. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. Has the requested. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Pharmacy Prior Authroization Forms AetnaPharmacy Aetna Medicare Specialty Pharmacy Prior Authorization Form † use a separate claim form for each patient. Has the patient been receiving the requested drug within the last 120 days? They will look at your overall health or any. Please attach all clinical information. Required clinical information must be completed in its entirety for all precertification requests. To get prior authorization, your doctor must first submit a request. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From old.sermitsiaq.ag
Generic Prior Authorization Form Template Aetna Medicare Specialty Pharmacy Prior Authorization Form Please attach all clinical information. They will look at your overall health or any. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Has the patient been receiving the requested drug within the last 120 days? This guide includes lists of the services and medicines that need. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From freedownloads.net
Download AETNA Prescription Drug Authorization Request Form PDF RTF Aetna Medicare Specialty Pharmacy Prior Authorization Form They will look at your overall health or any. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. In some plans, you might need prior authorization for the place where you get a. † claims must be submitted within two years of date of purchase. All fields on this form are required.. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online (800) 3106826 Specialty Medication Prior Authorization Aetna Medicare Specialty Pharmacy Prior Authorization Form Please attach all clinical information. All fields on this form are required. † claims must be submitted within two years of date of purchase. Specialty drug prior authorization requests. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. They will look at your overall health or any. In some plans, you might. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Specialty Pharmacy Prior Authorization Form Fax Email Aetna Medicare Specialty Pharmacy Prior Authorization Form Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Required clinical information must be completed in its entirety for all precertification requests. Has the patient been receiving the requested drug within the last 120 days? † use a separate claim form for each patient. † claims must be submitted within two years. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From ariaatr.com
Free Aetna Prior Rx Authorization Form Pdf Eforms Aria Art Aetna Medicare Specialty Pharmacy Prior Authorization Form † use a separate claim form for each patient. Please attach all clinical information. This form is for use only where a. † claims must be submitted within two years of date of purchase. In some plans, you might need prior authorization for the place where you get a. Has the patient been receiving the requested drug within the last. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From ariaatr.com
Free Aetna Prior Rx Authorization Form Pdf Eforms Aria Art Aetna Medicare Specialty Pharmacy Prior Authorization Form This form is for use only where a. Specialty drug prior authorization requests. Please attach all clinical information. † claims must be submitted within two years of date of purchase. Has the patient been receiving the requested drug within the last 120 days? For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Aetna pharmacy management prior authorization form Fax Aetna Medicare Specialty Pharmacy Prior Authorization Form In some plans, you might need prior authorization for the place where you get a. Specialty drug prior authorization requests. Please attach all clinical information. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. This guide includes lists of the services and medicines that need prior authorization. Has the patient been receiving. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.scribd.com
Aetna Prior Authorization Form PDF Medical Record Health Sciences Aetna Medicare Specialty Pharmacy Prior Authorization Form Has the patient been receiving the requested drug within the last 120 days? Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. † use a separate claim form for each patient. Please attach all clinical information. † claims must be submitted within two years of date of purchase. This guide includes lists. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.formsbank.com
Specialty Pharmacy Prior Authorization Form printable pdf download Aetna Medicare Specialty Pharmacy Prior Authorization Form Specialty drug prior authorization requests. Please attach all clinical information. † claims must be submitted within two years of date of purchase. In some plans, you might need prior authorization for the place where you get a. This form is for use only where a. To get prior authorization, your doctor must first submit a request for a specific procedure,. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Pharmacy Prior Authorization Request Form Aetna Aetna Medicare Specialty Pharmacy Prior Authorization Form In some plans, you might need prior authorization for the place where you get a. Required clinical information must be completed in its entirety for all precertification requests. Please attach all clinical information. This form is for use only where a. Specialty drug prior authorization requests. † claims must be submitted within two years of date of purchase. They will. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From pharmacywalls.blogspot.com
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls Aetna Medicare Specialty Pharmacy Prior Authorization Form This form is for use only where a. † use a separate claim form for each patient. Required clinical information must be completed in its entirety for all precertification requests. Specialty drug prior authorization requests. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Has the requested. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Pharmacy Prior Authroization Forms AetnaPharmacy Aetna Medicare Specialty Pharmacy Prior Authorization Form Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Specialty drug prior authorization requests. † claims must be submitted within two years of date of purchase. In some plans, you might need prior authorization for the place where you get a. This guide includes lists of the services and medicines that need. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.planforms.net
Aetna Drug Plan Prior Authorization Form Aetna Medicare Specialty Pharmacy Prior Authorization Form In some plans, you might need prior authorization for the place where you get a. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. All fields on this form are required. Specialty drug prior authorization requests. This form is for use only where a. Has the patient been receiving the requested. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.dochub.com
06/04/2013 Prior Authorization AETNA BETTER HEALTH OF PENNSYLVANIA Non Aetna Medicare Specialty Pharmacy Prior Authorization Form Required clinical information must be completed in its entirety for all precertification requests. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. † claims must be submitted within two years of date of purchase. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Aetna Pharmacy Management Prior Auth Form. Aetna Aetna Medicare Specialty Pharmacy Prior Authorization Form For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. † claims must be submitted within two years of date of purchase. They will look at your overall health or any. Please attach all clinical information. Required clinical information must be completed in its entirety for all precertification. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.signnow.com
Banner Aetna Prior Authorization Form Complete with ease airSlate Aetna Medicare Specialty Pharmacy Prior Authorization Form This form is for use only where a. Has the patient been receiving the requested drug within the last 120 days? Specialty drug prior authorization requests. Required clinical information must be completed in its entirety for all precertification requests. They will look at your overall health or any. Please attach all clinical information. This guide includes lists of the services. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
20222024 Form Aetna GR69265 Fill Online, Printable, Fillable, Blank Aetna Medicare Specialty Pharmacy Prior Authorization Form This form is for use only where a. They will look at your overall health or any. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Specialty drug prior authorization requests. Has the patient been receiving the requested drug within the last 120 days? Required clinical information must be completed in its. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From studylib.net
Specialty Medication Prior Authorization Cover Sheet Aetna Medicare Specialty Pharmacy Prior Authorization Form † use a separate claim form for each patient. In some plans, you might need prior authorization for the place where you get a. Specialty drug prior authorization requests. Please attach all clinical information. This guide includes lists of the services and medicines that need prior authorization. To get prior authorization, your doctor must first submit a request for a. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Aetna Medicare Prior Authorization Form Fill Online, Printable Aetna Medicare Specialty Pharmacy Prior Authorization Form All fields on this form are required. † claims must be submitted within two years of date of purchase. Required clinical information must be completed in its entirety for all precertification requests. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. Please attach all clinical information. In some plans, you might need. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From eforms.com
Free Aetna Prior (Rx) Authorization Form PDF eForms Aetna Medicare Specialty Pharmacy Prior Authorization Form Required clinical information must be completed in its entirety for all precertification requests. All fields on this form are required. They will look at your overall health or any. † claims must be submitted within two years of date of purchase. To get prior authorization, your doctor must first submit a request for a specific procedure, test or prescription. For. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.sampleforms.com
FREE 10+ Sample Medicare Forms in PDF MS Word Aetna Medicare Specialty Pharmacy Prior Authorization Form For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. † claims must be submitted within two years of date of purchase. Has the patient been receiving the requested drug within the last 120 days? Specialty drug prior authorization requests. To get prior authorization, your doctor must first. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.pdffiller.com
Fillable Online Aetna Medicare Medication Prior Authorization Form Fax Aetna Medicare Specialty Pharmacy Prior Authorization Form In some plans, you might need prior authorization for the place where you get a. † claims must be submitted within two years of date of purchase. Has the requested drug been dispensed at a pharmacy and approved for coverage previously by a prior. All fields on this form are required. This form is for use only where a. This. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From www.formsbank.com
From Wv160601 Aetna Prior Authorization Form printable pdf download Aetna Medicare Specialty Pharmacy Prior Authorization Form This guide includes lists of the services and medicines that need prior authorization. † claims must be submitted within two years of date of purchase. This form is for use only where a. Please attach all clinical information. Has the patient been receiving the requested drug within the last 120 days? Has the requested drug been dispensed at a pharmacy. Aetna Medicare Specialty Pharmacy Prior Authorization Form.
From authorizationforms.com
Free AETNA Prior Prescription (Rx) Authorization Form PDF Aetna Medicare Specialty Pharmacy Prior Authorization Form † claims must be submitted within two years of date of purchase. In some plans, you might need prior authorization for the place where you get a. Please attach all clinical information. For part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. To get prior authorization, your doctor. Aetna Medicare Specialty Pharmacy Prior Authorization Form.