Cvs Caremark Prior Auth Forms . Learn how to fill in the form with the patient’s. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. If a form for the specific medication cannot be found, please use the global prior authorization form. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? California members please use the.
from www.sampletemplates.com
Learn how to fill in the form with the patient’s. California members please use the. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If a form for the specific medication cannot be found, please use the global prior authorization form. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination?
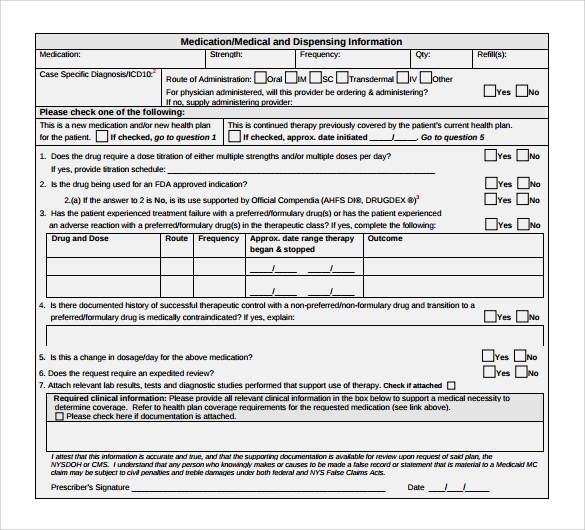
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Cvs Caremark Prior Auth Forms Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. If a form for the specific medication cannot be found, please use the global prior authorization form. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Learn how to fill in the form with the patient’s. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. California members please use the. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print Cvs Caremark Prior Auth Forms Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. California members please use the. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Learn how to fill in the form with the patient’s. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Refer. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Cvs Caremark Formulary Exception Prior Authorization Request Form Cvs Caremark Prior Auth Forms If a form for the specific medication cannot be found, please use the global prior authorization form. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. California members please use the. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Prescription benefit plan may request additional. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Auth Forms Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? California members please use the.. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email Cvs Caremark Prior Auth Forms Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Learn how to fill in the form with the patient’s. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Requests that are subject to prior authorization (or any other utilization. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Forms If a form for the specific medication cannot be found, please use the global prior authorization form. Learn how to fill in the form with the patient’s. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Did you. Cvs Caremark Prior Auth Forms.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Auth Forms California members please use the. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of.. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Form Fax Email Print Cvs Caremark Prior Auth Forms Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Learn how to fill in the form with the patient’s. California members please use the. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Cvs caremark prior authorization (pa) tools are. Cvs Caremark Prior Auth Forms.
From www.authorizationform.net
Cvs Caremark Ivig Prior Authorization Form Cvs Caremark Prior Auth Forms Learn how to fill in the form with the patient’s. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Did you know. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
9+ Sample Caremark Prior Authorization Forms Sample Templates Cvs Caremark Prior Auth Forms California members please use the. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? If. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Auth Forms Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. If a form for the specific medication cannot be found, please use the global prior authorization form. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Download a free pdf form to request coverage for a cvs/caremark. Cvs Caremark Prior Auth Forms.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Forms California members please use the. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If a form for the specific medication cannot be found,. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Forms Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Learn how to fill in the form with the patient’s. Prescription benefit plan may. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Forms Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Learn how to fill in the form with the patient’s. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2. Cvs Caremark Prior Auth Forms.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Auth Forms If a form for the specific medication cannot be found, please use the global prior authorization form. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Requests that are subject to. Cvs Caremark Prior Auth Forms.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Forms Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Learn how to fill in. Cvs Caremark Prior Auth Forms.
From www.sample-templatess123.com
Simple Caremark Prior Authorization Form Sample Templates Cvs Caremark Prior Auth Forms Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. If a form for the specific medication cannot be found, please use the global prior authorization form. Did you know submitting prior authorizations (pas) by fax or phone can. Cvs Caremark Prior Auth Forms.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Forms Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Learn how to fill in the form with the patient’s. California members please use the. If a form for the specific medication cannot be found, please use the global prior authorization form. Cvs caremark prior authorization. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print Cvs Caremark Prior Auth Forms Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. California members please use the. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Requests that are subject to prior authorization (or any other. Cvs Caremark Prior Auth Forms.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Forms Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Learn how to fill in the form with the patient’s. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Requests that are subject to prior authorization (or any other utilization. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Auth Forms Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. California members please use the. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Refer. Cvs Caremark Prior Auth Forms.
From eforms.com
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Auth Forms California members please use the. If a form for the specific medication cannot be found, please use the global prior authorization form. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Learn how to fill in the form with the patient’s. Did you know submitting prior authorizations (pas) by fax or phone can. Cvs Caremark Prior Auth Forms.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Forms Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Learn how to fill in the form with the patient’s. If a form for the specific medication cannot be found, please use the global prior authorization form. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Download a. Cvs Caremark Prior Auth Forms.
From www.authorizationform.net
Caremark Prior Authorization Form Printable Pdf Download Cvs Caremark Prior Auth Forms Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If a form for the specific medication cannot be found, please use the global prior authorization form. California members please use the.. Cvs Caremark Prior Auth Forms.
From www.formsbank.com
Caremark Prior Authorization Criteria Request Form printable pdf download Cvs Caremark Prior Auth Forms Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Learn how to fill in the form with the patient’s. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. California members please use the. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Auth Forms If a form for the specific medication cannot be found, please use the global prior authorization form. California members please use the. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Learn how to fill in the form with the patient’s. Refer to insomnia (zolpidem. Cvs Caremark Prior Auth Forms.
From www.dochub.com
Cvs caremark wegovy prior authorization criteria Fill out & sign Cvs Caremark Prior Auth Forms California members please use the. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Learn how to fill in the form with the patient’s. If a form for the specific medication cannot be found, please use the global prior authorization form. Requests that are subject to prior authorization (or any other utilization management requirement), may. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
20212024 Form CVS Caremark 10637207A Fill Online, Printable, Fillable Cvs Caremark Prior Auth Forms Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If a form for the specific medication cannot be found, please use the global prior authorization. Cvs Caremark Prior Auth Forms.
From www.formsbank.com
Caremark Prior Authorization Criteria Request Form printable pdf download Cvs Caremark Prior Auth Forms Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. California members please use the. Learn how to fill in the form with the patient’s. Requests. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Forms Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If a form for the specific medication cannot. Cvs Caremark Prior Auth Forms.
From www.authorizationform.net
Cvs Caremark Synagis Prior Authorization Form Cvs Caremark Prior Auth Forms Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. California members please use the. Requests that are subject to prior authorization (or any other utilization management. Cvs Caremark Prior Auth Forms.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Auth Forms Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. If a form for the specific medication cannot be found, please use the global prior authorization form. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere. Cvs Caremark Prior Auth Forms.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Forms Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. If a form for the specific medication cannot be found, please use the global prior authorization form. Learn how to fill in the form with the patient’s. Refer to. Cvs Caremark Prior Auth Forms.
From mungfali.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable E10 Cvs Caremark Prior Auth Forms Learn how to fill in the form with the patient’s. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of. Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. California members please use the. Prescription benefit plan may request additional information or clarification, if needed, to evaluate requests.. Cvs Caremark Prior Auth Forms.
From www.pdffiller.com
2019 Form CVS Caremark 10637207A Fill Online, Printable, Fillable Cvs Caremark Prior Auth Forms Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Did you know submitting prior authorizations (pas) by fax or phone can take anywhere from 16 hours to 2 days to receive a determination? Refer to insomnia (zolpidem sublingual, oral spray) or insomnia (belsomra, dayvigo, quviviq) prior authorization criteria. Prescription benefit plan may request additional information. Cvs Caremark Prior Auth Forms.
From www.formsbank.com
Cvs Caremark Taltz Passport Prior Authorization Request printable pdf Cvs Caremark Prior Auth Forms If a form for the specific medication cannot be found, please use the global prior authorization form. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Download a free pdf form to request coverage for a cvs/caremark plan member’s prescription. Did you know submitting prior authorizations (pas) by fax or phone can. Cvs Caremark Prior Auth Forms.