What Is A Soap Progress Note . It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are intended to capture specific information about a client and certain aspects of the session. Soap notes are a specific format for writing. What is a soap note? In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note. What is a soap note? Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Learning soap note taking can make the job of documenting progress notes and client interactions easier. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. We’ve also compiled some soap.
from www.wordtemplatesonline.net
Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific format for writing. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. It is the documentation used to record information about encounters with patients that follows a specific format. What is a soap note? Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note?
How to Write a SOAP Note (20+ SOAP Note Examples)
What Is A Soap Progress Note What is a soap note? We’ve also compiled some soap. What is a soap note? Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a specific format for writing. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are intended to capture specific information about a client and certain aspects of the session. Soap is an acronym for the 4 sections, or headings, that each progress note contains: What is a soap note? Learning soap note taking can make the job of documenting progress notes and client interactions easier. Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. It is the documentation used to record information about encounters with patients that follows a specific format.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab What Is A Soap Progress Note Soap is an acronym for the 4 sections, or headings, that each progress note contains: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a specific format for writing. We’ve also compiled some soap. Soap. What Is A Soap Progress Note.
From www.researchgate.net
An example progress note with SOAP sections annotated. Line breaks are What Is A Soap Progress Note We’ve also compiled some soap. It is the documentation used to record information about encounters with patients that follows a specific format. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Here’s how. What Is A Soap Progress Note.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is A Soap Progress Note Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are intended to capture specific information about a client and certain aspects of the session. Here’s how soap notes can help you write better, faster notes — and effectively document. What Is A Soap Progress Note.
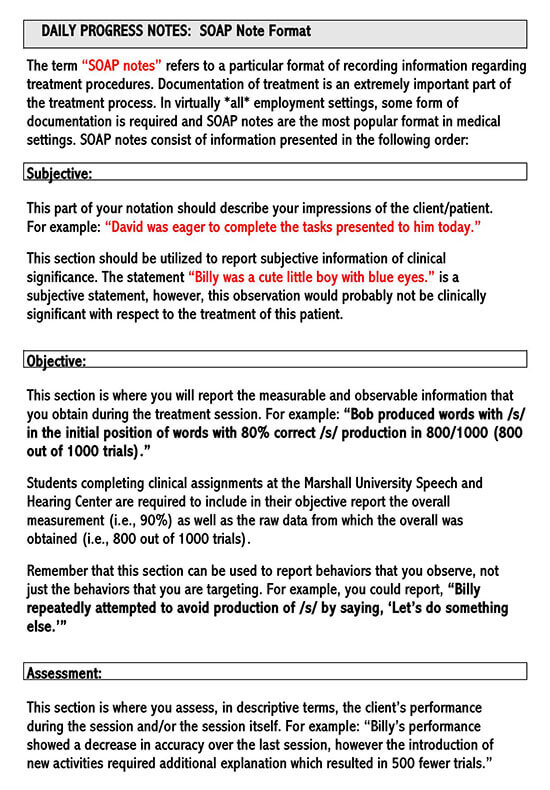
From studylib.net
PROGRESS (SOAP) NOTES What Is A Soap Progress Note Soap notes are a specific format for writing. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Learning soap note taking can make the job of documenting progress notes and client interactions easier. Soap notes are intended to capture specific information about a client and certain aspects of. What Is A Soap Progress Note.
From www.printabletemplateslab.com
10+ Soap Note Template Free Download Word, Excel, PDF Format!! What Is A Soap Progress Note Soap nursing notes are a type of patient progress note or nurse’s note. What is a soap note? Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a specific format for writing. Where a client’s subjective experiences, feelings, or perspectives are recorded. It is the documentation used to record information about. What Is A Soap Progress Note.
From www.carepatron.com
SOAP Progress Notes Template & Example Free PDF Download What Is A Soap Progress Note Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are intended to capture specific information about a client and certain aspects of the session. Here’s how soap notes can help. What Is A Soap Progress Note.
From musculoskeletalkey.com
Treatment Notes and Progress Notes Using a Modified SOAP Format What Is A Soap Progress Note What is a soap note? What is a soap note? In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Learning soap note taking can make the job of documenting progress notes and client interactions easier. Soap notes are a way for healthcare providers to document patient data more. What Is A Soap Progress Note.
From www.scribd.com
SOAP Progress Notes PDF Pain Medical Diagnosis What Is A Soap Progress Note Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are intended to capture specific information about a client and certain aspects of the session. What is a soap note? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. In this article, we’ll cover how to. What Is A Soap Progress Note.
From www.etsy.com
SOAP Progress Note for School Counselors, Editable Google Doc, School What Is A Soap Progress Note What is a soap note? What is a soap note? Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are intended to capture specific information about a client and certain aspects of the session. It is the documentation used to record information about encounters. What Is A Soap Progress Note.
From www.wordtemplatesonline.net
How to Write a SOAP Note (20+ SOAP Note Examples) What Is A Soap Progress Note Soap notes are a specific format for writing. What is a soap note? In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. We’ve also compiled some soap. The. What Is A Soap Progress Note.
From www.sampletemplates.com
FREE 9+ Sample Progress Note Templates in PDF MS Word What Is A Soap Progress Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Where a client’s subjective experiences, feelings, or perspectives are recorded. Learning soap note taking can make the job of documenting progress notes and client interactions easier. It is the documentation used to record information about encounters with patients that. What Is A Soap Progress Note.
From www.wordtemplatesonline.net
How to Write a SOAP Note (20+ SOAP Note Examples) What Is A Soap Progress Note Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. We’ve also compiled some soap. What is a soap note? Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely. What Is A Soap Progress Note.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is A Soap Progress Note What is a soap note? Learning soap note taking can make the job of documenting progress notes and client interactions easier. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Here’s how soap notes can help you write better, faster notes — and effectively document your work as. What Is A Soap Progress Note.
From www.capterra.com
Free Soap Notes Templates for Busy Healthcare Professionals Capterra What Is A Soap Progress Note What is a soap note? What is a soap note? In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are intended to capture specific information about a client and certain aspects of the session. Where a client’s subjective experiences, feelings, or perspectives are recorded. The subjective,. What Is A Soap Progress Note.
From shootersjournal.net
Soap Progress Notes Template What Is A Soap Progress Note We’ve also compiled some soap. Soap is an acronym for the 4 sections, or headings, that each progress note contains: It is the documentation used to record information about encounters with patients that follows a specific format. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. What is. What Is A Soap Progress Note.
From shootersjournal.net
Soap Progress Notes Template What Is A Soap Progress Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. What is a soap note? In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note.. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note What is a soap note? What is a soap note? Where a client’s subjective experiences, feelings, or perspectives are recorded. It is the documentation used to record information about encounters with patients that follows a specific format. Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. Soap notes are. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note Learning soap note taking can make the job of documenting progress notes and client interactions easier. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a specific format for writing. We’ve also compiled some soap. What is a soap note? What is a soap note? It is the documentation used to record information about encounters with. What Is A Soap Progress Note.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is A Soap Progress Note Learning soap note taking can make the job of documenting progress notes and client interactions easier. Where a client’s subjective experiences, feelings, or perspectives are recorded. We’ve also compiled some soap. Soap is an acronym for the 4 sections, or headings, that each progress note contains: In this article, we’ll cover how to write soap notes, describing the soap format. What Is A Soap Progress Note.
From www.vrogue.co
Sample Soap Notes Occupational Therapy Pdf Fill Out A vrogue.co What Is A Soap Progress Note Learning soap note taking can make the job of documenting progress notes and client interactions easier. It is the documentation used to record information about encounters with patients that follows a specific format. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Here’s how soap notes can help. What Is A Soap Progress Note.
From www.sampletemplates.com
16+ Sample SOAP Note Examples PDF, Word Sample Templates What Is A Soap Progress Note What is a soap note? Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap nursing notes are a type of patient progress note or nurse’s note. What is a soap note? Soap is an acronym for the 4 sections, or headings, that each progress note contains: Here’s how soap notes can help you write better, faster notes —. What Is A Soap Progress Note.
From idtcenter.org
Sample Physical Therapist Soap Notes Example Soap Note Notes Ot What Is A Soap Progress Note Soap notes are a specific format for writing. Where a client’s subjective experiences, feelings, or perspectives are recorded. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. It is the documentation used to record information about encounters with patients that follows a specific format. What. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Where a client’s subjective experiences, feelings, or perspectives are recorded. What is a soap note? Soap is an acronym. What Is A Soap Progress Note.
From www.theraplatform.com
Occupational therapy SOAP note What Is A Soap Progress Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a specific format for writing. Learning soap note taking can make the job of documenting progress notes and client interactions easier. Soap nursing notes are a type of patient progress note or nurse’s note. It is. What Is A Soap Progress Note.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] What Is A Soap Progress Note Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note? In this article, we’ll cover how to write soap. What Is A Soap Progress Note.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary What Is A Soap Progress Note We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are intended to capture specific information about a client and certain aspects of the session. What is a soap note? Soap notes are a specific format for writing. Soap is an acronym. What Is A Soap Progress Note.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download What Is A Soap Progress Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are intended to capture specific information about a client and certain aspects of the session. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note? Where. What Is A Soap Progress Note.
From lesboucans.com
Therapy Progress Note Template Free For Your Needs What Is A Soap Progress Note Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a specific format for writing. Soap is an acronym for. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note Learning soap note taking can make the job of documenting progress notes and client interactions easier. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The subjective, objective,. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Here’s how soap notes can help you write better, faster notes — and effectively document your work as a clinician. Learning. What Is A Soap Progress Note.
From www.artemisaba.com
ABA SOAP Notes Tips, Examples & Template Artemis ABA What Is A Soap Progress Note What is a soap note? In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Learning soap note taking can make the job of documenting progress notes and client interactions easier. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are. What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note What is a soap note? Soap notes are intended to capture specific information about a client and certain aspects of the session. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap). What Is A Soap Progress Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is A Soap Progress Note It is the documentation used to record information about encounters with patients that follows a specific format. What is a soap note? We’ve also compiled some soap. Soap nursing notes are a type of patient progress note or nurse’s note. What is a soap note? Soap notes are a way for healthcare providers to document patient data more efficiently and. What Is A Soap Progress Note.
From www.wordtemplatesonline.net
How to Write a SOAP Note (with SOAP Note Examples) What Is A Soap Progress Note We’ve also compiled some soap. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. What is a soap note? Soap notes are a. What Is A Soap Progress Note.