What Is Soap In Medical Terms . Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Learn how to write soap notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Each letter refers to one of four sections in the document.
from www.slideshare.net
Each letter refers to one of four sections in the document. Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for: Learn how to write soap notes. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare.
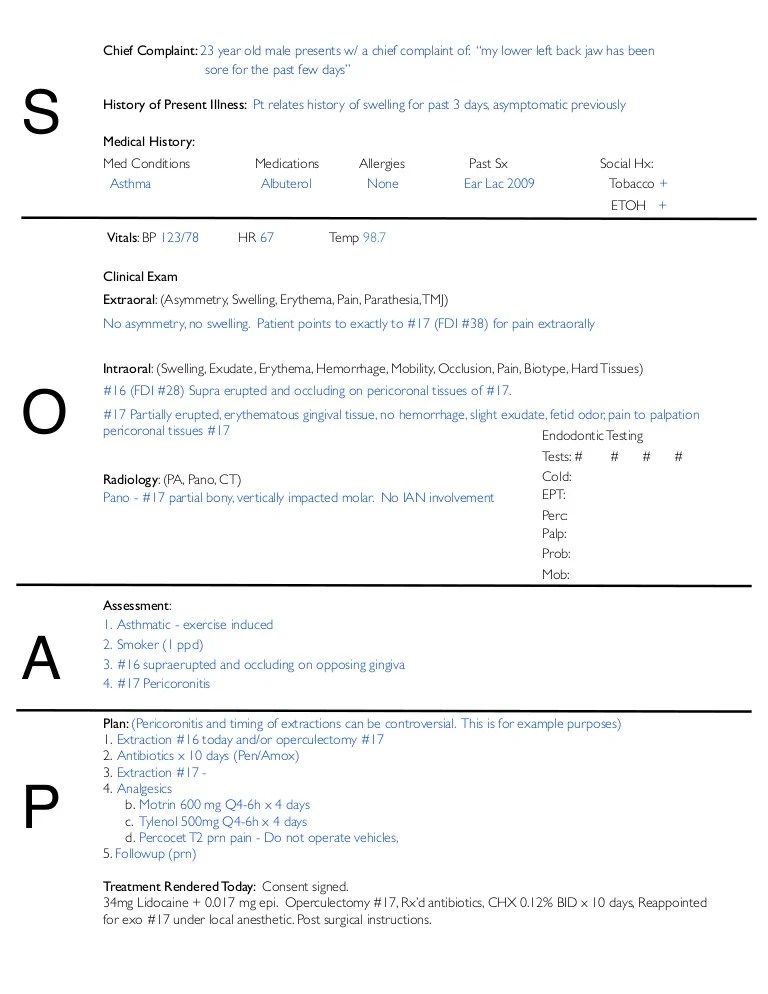
SOAP Notes Dentistry Example
What Is Soap In Medical Terms Soap is an acronym for: Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Learn how to write soap notes. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers.
From viewpoint.online
How to put the patient first in your eye examinations Viewpoint What Is Soap In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is. What Is Soap In Medical Terms.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by What Is Soap In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. The soap note (an acronym for subjective, objective, assessment,. What Is Soap In Medical Terms.
From medicalaid.org
Understanding SOAP Notes for Clinical Rotations International Medical Aid What Is Soap In Medical Terms Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for: Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap notes are a. What Is Soap In Medical Terms.
From www.slideshare.net
Nursing Skills Charting What Is Soap In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a method of documentation in medical and healthcare settings,. What Is Soap In Medical Terms.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education What Is Soap In Medical Terms Each letter refers to one of four sections in the document. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap is an acronym for: The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes are a way for healthcare. What Is Soap In Medical Terms.
From www.process.st
SOAP Note Template Process Street What Is Soap In Medical Terms Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Each letter refers to one of four sections in the document. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes are a way for healthcare providers to document patient data. What Is Soap In Medical Terms.
From snipe.fm
😊 Pharmacy soap note example. How to Write a SOAP Note With Obstetric What Is Soap In Medical Terms Learn how to write soap notes. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective,. What Is Soap In Medical Terms.
From covenantlifecog.com
SOAPmethodposter What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: Soap notes are a structured. What Is Soap In Medical Terms.
From www.youtube.com
How to Write SOAP Notes YouTube What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap is an acronym for: Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more. What Is Soap In Medical Terms.
From in.pinterest.com
First Aid CPD SOAP 👀⠀ ⠀ SOAP is a medical acronym used to remember What Is Soap In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Learn how to write soap notes. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note (an acronym for subjective, objective,. What Is Soap In Medical Terms.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Learn how to write soap notes.. What Is Soap In Medical Terms.
From musculoskeletalkey.com
Treatment Notes and Progress Notes Using a Modified SOAP Format What Is Soap In Medical Terms Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap is an acronym for: Learn how to write soap notes. Each letter refers to one of four sections in the document. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. The. What Is Soap In Medical Terms.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For What Is Soap In Medical Terms Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Learn how to write soap notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and. What Is Soap In Medical Terms.
From www.slideserve.com
PPT PATIENT MEDICAL RECORDS PowerPoint Presentation, free download What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Each letter refers to. What Is Soap In Medical Terms.
From exyvqkqfp.blob.core.windows.net
What Is A Soap Note In Medical Terms at Clarence Bohannon blog What Is Soap In Medical Terms Each letter refers to one of four sections in the document. Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap is an acronym for: The soap note (an acronym for subjective,. What Is Soap In Medical Terms.
From knowmedge.com
Medical Mnemonics Diagnostic Criteria for SLE Soap Brain MD USMLE What Is Soap In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Learn how to write soap notes. Soap notes are a method of documentation in medical and healthcare settings,. What Is Soap In Medical Terms.
From gioizlnut.blob.core.windows.net
Medical Record Terms at Vivian Smith blog What Is Soap In Medical Terms The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Each letter refers to one of four sections in the document. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes are a way for healthcare providers to. What Is Soap In Medical Terms.
From exyvqkqfp.blob.core.windows.net
What Is A Soap Note In Medical Terms at Clarence Bohannon blog What Is Soap In Medical Terms The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Learn how to write soap notes. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. The soap. What Is Soap In Medical Terms.
From www.youtube.com
What is Saponification? Structure and Action of Soaps and Detergents What Is Soap In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: Learn how to write soap notes. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Each letter. What Is Soap In Medical Terms.
From www.theraplatform.com
Occupational therapy SOAP note What Is Soap In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for: Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap notes are a. What Is Soap In Medical Terms.
From www.pinterest.com
Soap Note Template Nurse Practitioner Lovely What is A soap Note What Is Soap In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Learn how to write soap notes. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for: Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap notes. What Is Soap In Medical Terms.
From canadianpa.ca
How to write a SOAP note — CANADIAN PA What Is Soap In Medical Terms Learn how to write soap notes. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Each letter refers to one of four. What Is Soap In Medical Terms.
From www.slideshare.net
SOAP Notes Dentistry Example What Is Soap In Medical Terms Soap is an acronym for: Learn how to write soap notes. Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The. What Is Soap In Medical Terms.
From fyoqjvbid.blob.core.windows.net
Soap Note Example Diabetes at Amanda Fleming blog What Is Soap In Medical Terms Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Soap is an acronym for: Learn how to write soap notes. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. What Is Soap In Medical Terms.
From www.pinterest.com.au
Medical Soap Note Template SOAP Note Guide YouTube Soap note What Is Soap In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Each letter refers to one of four sections in. What Is Soap In Medical Terms.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] What Is Soap In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. Soap is an acronym for: Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. The soap note (an acronym for subjective, objective, assessment, and. What Is Soap In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is Soap In Medical Terms Learn how to write soap notes. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for: Soap notes are a way. What Is Soap In Medical Terms.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for: Learn how to write soap notes. In the soap format, soap stands for subjective, objective,. What Is Soap In Medical Terms.
From www.pinterest.com
soap notes with the words soap on it What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap is an acronym for: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each. What Is Soap In Medical Terms.
From exyvqkqfp.blob.core.windows.net
What Is A Soap Note In Medical Terms at Clarence Bohannon blog What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. Learn how to write soap notes. The soap note (an acronym. What Is Soap In Medical Terms.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Is Soap In Medical Terms Soap is an acronym for: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. In the. What Is Soap In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is Soap In Medical Terms Learn how to write soap notes. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Soap notes are. What Is Soap In Medical Terms.
From www.youtube.com
HCM210 Medical Terminology SOAP Notes YouTube What Is Soap In Medical Terms Soap is an acronym for: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. In the soap format, soap stands for subjective, objective, assessment, and plan. Learn how to. What Is Soap In Medical Terms.
From www.henryford.com
What’s the Dirt On Antibacterial Soap? Henry Ford Health Detroit, MI What Is Soap In Medical Terms Soap notes are a method of documentation in medical and healthcare settings, consisting of subjective, objective, assessment, and plan. Soap is an acronym for: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note (an acronym for subjective, objective,. What Is Soap In Medical Terms.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Is Soap In Medical Terms Soap notes are a structured way of recording patient encounters, consisting of subjective, objective, assessment and plan sections. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. The subjective, objective, assessment and plan (soap) note is an acronym. What Is Soap In Medical Terms.