Cvs Caremark Prior Auth Form For Medication . The requested drug will be covered with prior authorization when the following criteria are met: A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. • the patient has a diagnosis of type 2 diabetes. Please provide all relevant clinical documentation to support use of this medication. Epa is a fully electronic solution that processes pas, formulary and quantity. When a pa is needed for a prescription, the member will be asked to have. Contact cvs caremark prior authorization department medicare part d. Initial prior authorization with quantity limit. Please list all medications the patient has tried specific to the diagnosis and specify below: Submit a prior authorization request electronically. Therapeutic failure, including length of therapy for each drug:
from www.formsbank.com
When a pa is needed for a prescription, the member will be asked to have. Submit a prior authorization request electronically. Please list all medications the patient has tried specific to the diagnosis and specify below: Therapeutic failure, including length of therapy for each drug: Please provide all relevant clinical documentation to support use of this medication. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. • the patient has a diagnosis of type 2 diabetes. The requested drug will be covered with prior authorization when the following criteria are met: Epa is a fully electronic solution that processes pas, formulary and quantity. Contact cvs caremark prior authorization department medicare part d.
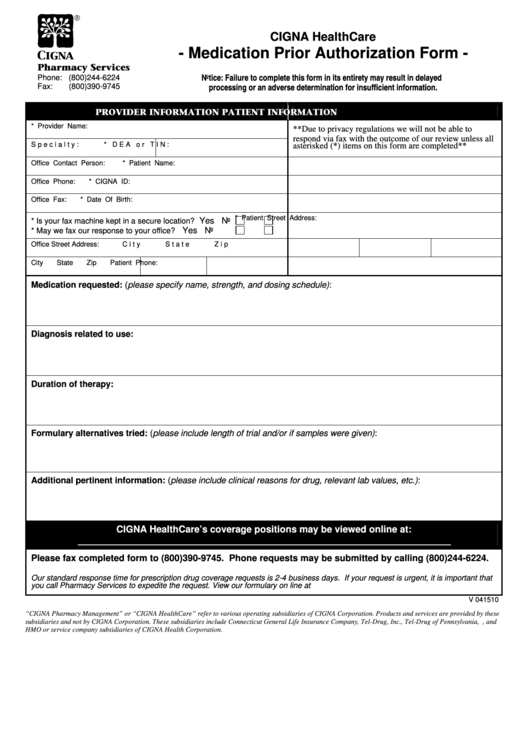
Medication Prior Authorization Form printable pdf download
Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. Initial prior authorization with quantity limit. Please list all medications the patient has tried specific to the diagnosis and specify below: Please provide all relevant clinical documentation to support use of this medication. Submit a prior authorization request electronically. The requested drug will be covered with prior authorization when the following criteria are met: Contact cvs caremark prior authorization department medicare part d. • the patient has a diagnosis of type 2 diabetes. When a pa is needed for a prescription, the member will be asked to have. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Epa is a fully electronic solution that processes pas, formulary and quantity. Therapeutic failure, including length of therapy for each drug:
From www.signnow.com
Cvs Caremark Appeal PDF 20032024 Form Fill Out and Sign Printable Cvs Caremark Prior Auth Form For Medication The requested drug will be covered with prior authorization when the following criteria are met: Initial prior authorization with quantity limit. Epa is a fully electronic solution that processes pas, formulary and quantity. Please list all medications the patient has tried specific to the diagnosis and specify below: When a pa is needed for a prescription, the member will be. Cvs Caremark Prior Auth Form For Medication.
From www.signnow.com
Cvs Caremark Fax Number Edit & Share airSlate SignNow Cvs Caremark Prior Auth Form For Medication The requested drug will be covered with prior authorization when the following criteria are met: Contact cvs caremark prior authorization department medicare part d. Please provide all relevant clinical documentation to support use of this medication. When a pa is needed for a prescription, the member will be asked to have. Therapeutic failure, including length of therapy for each drug:. Cvs Caremark Prior Auth Form For Medication.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Form For Medication When a pa is needed for a prescription, the member will be asked to have. Submit a prior authorization request electronically. Therapeutic failure, including length of therapy for each drug: The requested drug will be covered with prior authorization when the following criteria are met: Epa is a fully electronic solution that processes pas, formulary and quantity. • the patient. Cvs Caremark Prior Auth Form For Medication.
From eforms.com
Free Medicare Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Auth Form For Medication Therapeutic failure, including length of therapy for each drug: Please list all medications the patient has tried specific to the diagnosis and specify below: Contact cvs caremark prior authorization department medicare part d. When a pa is needed for a prescription, the member will be asked to have. The requested drug will be covered with prior authorization when the following. Cvs Caremark Prior Auth Form For Medication.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Auth Form For Medication Submit a prior authorization request electronically. • the patient has a diagnosis of type 2 diabetes. Epa is a fully electronic solution that processes pas, formulary and quantity. Please provide all relevant clinical documentation to support use of this medication. Contact cvs caremark prior authorization department medicare part d. Therapeutic failure, including length of therapy for each drug: The requested. Cvs Caremark Prior Auth Form For Medication.
From www.sampleforms.com
FREE 41+ Authorization Forms in PDF Excel MS word Cvs Caremark Prior Auth Form For Medication Initial prior authorization with quantity limit. Epa is a fully electronic solution that processes pas, formulary and quantity. The requested drug will be covered with prior authorization when the following criteria are met: Please list all medications the patient has tried specific to the diagnosis and specify below: Therapeutic failure, including length of therapy for each drug: Please provide all. Cvs Caremark Prior Auth Form For Medication.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Form For Medication Therapeutic failure, including length of therapy for each drug: Please provide all relevant clinical documentation to support use of this medication. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. The requested drug will be covered with prior authorization when the following criteria are met: Contact cvs caremark. Cvs Caremark Prior Auth Form For Medication.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Submit a prior authorization request electronically. Initial prior authorization with quantity limit. Please list all medications the patient has tried specific to the diagnosis and specify below:. Cvs Caremark Prior Auth Form For Medication.
From eforms.com
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Auth Form For Medication Please list all medications the patient has tried specific to the diagnosis and specify below: A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Contact cvs caremark prior authorization department medicare part d. • the patient has a diagnosis of type 2 diabetes. When a pa is needed. Cvs Caremark Prior Auth Form For Medication.
From exobjyvlx.blob.core.windows.net
Cvs Caremark Prior Auth Forms Pdf at Milly Hicks blog Cvs Caremark Prior Auth Form For Medication The requested drug will be covered with prior authorization when the following criteria are met: When a pa is needed for a prescription, the member will be asked to have. Contact cvs caremark prior authorization department medicare part d. Therapeutic failure, including length of therapy for each drug: Please list all medications the patient has tried specific to the diagnosis. Cvs Caremark Prior Auth Form For Medication.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print Cvs Caremark Prior Auth Form For Medication Initial prior authorization with quantity limit. Please provide all relevant clinical documentation to support use of this medication. Please list all medications the patient has tried specific to the diagnosis and specify below: Submit a prior authorization request electronically. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s.. Cvs Caremark Prior Auth Form For Medication.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Form For Medication • the patient has a diagnosis of type 2 diabetes. Please list all medications the patient has tried specific to the diagnosis and specify below: Initial prior authorization with quantity limit. Therapeutic failure, including length of therapy for each drug: Please provide all relevant clinical documentation to support use of this medication. When a pa is needed for a prescription,. Cvs Caremark Prior Auth Form For Medication.
From www.reddit.com
CVS Caremark Prior Auth Denial r/Zepbound Cvs Caremark Prior Auth Form For Medication When a pa is needed for a prescription, the member will be asked to have. Please provide all relevant clinical documentation to support use of this medication. • the patient has a diagnosis of type 2 diabetes. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Therapeutic failure,. Cvs Caremark Prior Auth Form For Medication.
From www.uslegalforms.com
CVS Caremark 10637207A 20192021 Fill and Sign Printable Template Cvs Caremark Prior Auth Form For Medication Therapeutic failure, including length of therapy for each drug: A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Please list all medications the patient has tried specific to the diagnosis and specify below: Epa is a fully electronic solution that processes pas, formulary and quantity. When a pa. Cvs Caremark Prior Auth Form For Medication.
From mungfali.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable E10 Cvs Caremark Prior Auth Form For Medication The requested drug will be covered with prior authorization when the following criteria are met: Initial prior authorization with quantity limit. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. • the patient has a diagnosis of type 2 diabetes. Contact cvs caremark prior authorization department medicare part. Cvs Caremark Prior Auth Form For Medication.
From www.contrapositionmagazine.com
Molina Medicare Medication Prior Authorization Form Form Resume Cvs Caremark Prior Auth Form For Medication Epa is a fully electronic solution that processes pas, formulary and quantity. The requested drug will be covered with prior authorization when the following criteria are met: • the patient has a diagnosis of type 2 diabetes. Please list all medications the patient has tried specific to the diagnosis and specify below: Initial prior authorization with quantity limit. Contact cvs. Cvs Caremark Prior Auth Form For Medication.
From www.dochub.com
Cvs caremark wegovy prior authorization criteria Fill out & sign Cvs Caremark Prior Auth Form For Medication Initial prior authorization with quantity limit. Therapeutic failure, including length of therapy for each drug: When a pa is needed for a prescription, the member will be asked to have. The requested drug will be covered with prior authorization when the following criteria are met: Epa is a fully electronic solution that processes pas, formulary and quantity. Submit a prior. Cvs Caremark Prior Auth Form For Medication.
From www.sampleforms.com
FREE 10+ Sample Medicare Forms in PDF MS Word Cvs Caremark Prior Auth Form For Medication Epa is a fully electronic solution that processes pas, formulary and quantity. Contact cvs caremark prior authorization department medicare part d. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Please list all medications the patient has tried specific to the diagnosis and specify below: When a pa. Cvs Caremark Prior Auth Form For Medication.
From whatismedicaresurtaxreharui.blogspot.com
What Is Medicare Surtax Prior Authorization For Medication For Medicare Cvs Caremark Prior Auth Form For Medication Contact cvs caremark prior authorization department medicare part d. Submit a prior authorization request electronically. When a pa is needed for a prescription, the member will be asked to have. The requested drug will be covered with prior authorization when the following criteria are met: • the patient has a diagnosis of type 2 diabetes. Please provide all relevant clinical. Cvs Caremark Prior Auth Form For Medication.
From www.uslegalforms.com
Cvs Caremark Prescription Form 20202022 Fill and Sign Printable Cvs Caremark Prior Auth Form For Medication • the patient has a diagnosis of type 2 diabetes. Epa is a fully electronic solution that processes pas, formulary and quantity. The requested drug will be covered with prior authorization when the following criteria are met: Initial prior authorization with quantity limit. Submit a prior authorization request electronically. Please provide all relevant clinical documentation to support use of this. Cvs Caremark Prior Auth Form For Medication.
From www.signnow.com
Cvs Caremark Non Medicare Ulary Exception Prior Authorization Request Cvs Caremark Prior Auth Form For Medication Epa is a fully electronic solution that processes pas, formulary and quantity. Contact cvs caremark prior authorization department medicare part d. • the patient has a diagnosis of type 2 diabetes. Initial prior authorization with quantity limit. The requested drug will be covered with prior authorization when the following criteria are met: A cvs/caremark prior authorization form is to be. Cvs Caremark Prior Auth Form For Medication.
From www.formsbank.com
Medication Prior Authorization Form printable pdf download Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. The requested drug will be covered with prior authorization when the following criteria are met: Initial prior authorization with quantity limit. Contact cvs caremark prior authorization department medicare part d. Submit a prior authorization request electronically. Please list all medications the patient has tried specific to the diagnosis. Cvs Caremark Prior Auth Form For Medication.
From eforms.com
Free Medicaid (Rx) Prior Authorization Forms PDF eForms Cvs Caremark Prior Auth Form For Medication When a pa is needed for a prescription, the member will be asked to have. • the patient has a diagnosis of type 2 diabetes. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Therapeutic failure, including length of therapy for each drug: Contact cvs caremark prior authorization. Cvs Caremark Prior Auth Form For Medication.
From eforms.com
Free SilverScript Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Epa is a fully electronic solution that processes pas, formulary and quantity. When a pa is needed for a prescription, the member will be asked to have.. Cvs Caremark Prior Auth Form For Medication.
From www.pdffiller.com
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email Cvs Caremark Prior Auth Form For Medication Contact cvs caremark prior authorization department medicare part d. Please provide all relevant clinical documentation to support use of this medication. When a pa is needed for a prescription, the member will be asked to have. Therapeutic failure, including length of therapy for each drug: • the patient has a diagnosis of type 2 diabetes. Please list all medications the. Cvs Caremark Prior Auth Form For Medication.
From cvs-prior-auth-form.pdffiller.com
Cvs Caremark Prior Authorization Form Fill Online, Printable Cvs Caremark Prior Auth Form For Medication When a pa is needed for a prescription, the member will be asked to have. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Contact cvs caremark prior authorization department medicare part d. • the patient has a diagnosis of type 2 diabetes. Please provide all relevant clinical. Cvs Caremark Prior Auth Form For Medication.
From www.sampletemplates.com
9+ Sample Caremark Prior Authorization Forms Sample Templates Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. Therapeutic failure, including length of therapy for each drug: • the patient has a diagnosis of type 2 diabetes. Please list all medications the patient has tried specific to the diagnosis and specify below: When a pa is needed for a prescription, the member will be asked to. Cvs Caremark Prior Auth Form For Medication.
From www.signnow.com
Cvs Caremark Appeal Form Edit & Share airSlate SignNow Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. • the patient has a diagnosis of type 2 diabetes. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Contact cvs caremark prior authorization department medicare part d. Therapeutic failure, including length of therapy for each. Cvs Caremark Prior Auth Form For Medication.
From www.templateroller.com
Botox Passport Prior Authorization Request Form Cvs Caremark Fill Cvs Caremark Prior Auth Form For Medication A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Contact cvs caremark prior authorization department medicare part d. • the patient has a diagnosis of type 2 diabetes. When a pa is needed for a prescription, the member will be asked to have. Please list all medications the. Cvs Caremark Prior Auth Form For Medication.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Auth Form For Medication Please provide all relevant clinical documentation to support use of this medication. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Please list all medications the patient has tried specific to the diagnosis and specify below: Submit a prior authorization request electronically. The requested drug will be covered. Cvs Caremark Prior Auth Form For Medication.
From www.formsbank.com
Cvs Aveed Prior Authorization Request Form printable pdf download Cvs Caremark Prior Auth Form For Medication Submit a prior authorization request electronically. The requested drug will be covered with prior authorization when the following criteria are met: A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s. Please list all medications the patient has tried specific to the diagnosis and specify below: Therapeutic failure, including. Cvs Caremark Prior Auth Form For Medication.
From promo.sanmanuel.com
Wegovy Consent Form Printable Find A Word Cvs Caremark Prior Auth Form For Medication Therapeutic failure, including length of therapy for each drug: When a pa is needed for a prescription, the member will be asked to have. • the patient has a diagnosis of type 2 diabetes. Initial prior authorization with quantity limit. The requested drug will be covered with prior authorization when the following criteria are met: Epa is a fully electronic. Cvs Caremark Prior Auth Form For Medication.
From www.pdffiller.com
Cvs Caremark Formulary Exception Prior Authorization Request Form Cvs Caremark Prior Auth Form For Medication Epa is a fully electronic solution that processes pas, formulary and quantity. Please list all medications the patient has tried specific to the diagnosis and specify below: Submit a prior authorization request electronically. When a pa is needed for a prescription, the member will be asked to have. A cvs/caremark prior authorization form is to be used by a medical. Cvs Caremark Prior Auth Form For Medication.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Auth Form For Medication When a pa is needed for a prescription, the member will be asked to have. Please list all medications the patient has tried specific to the diagnosis and specify below: • the patient has a diagnosis of type 2 diabetes. Therapeutic failure, including length of therapy for each drug: Submit a prior authorization request electronically. The requested drug will be. Cvs Caremark Prior Auth Form For Medication.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Auth Form For Medication Submit a prior authorization request electronically. Please list all medications the patient has tried specific to the diagnosis and specify below: Epa is a fully electronic solution that processes pas, formulary and quantity. The requested drug will be covered with prior authorization when the following criteria are met: Contact cvs caremark prior authorization department medicare part d. Therapeutic failure, including. Cvs Caremark Prior Auth Form For Medication.