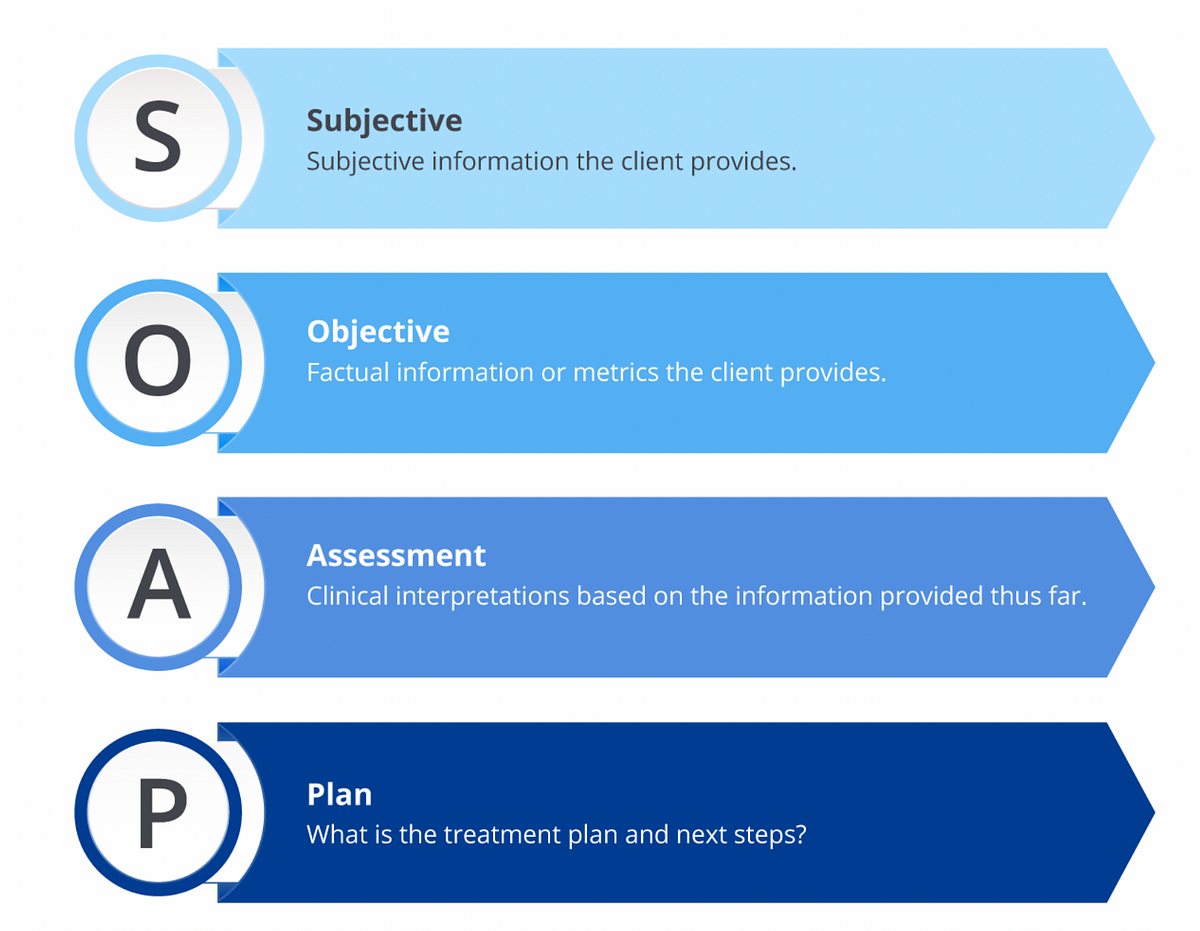
Soap Meaning Nursing . Soap notes are a standardized method for documenting patient information in healthcare. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Documenting a patient assessment in the notes is something all medical students need to practice. Soap nursing notes are a type of patient progress note or nurse’s note. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. This guide discusses the soapframework (subjective, objective,. The acronym stands for subjective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings.
from medium.com
Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The acronym stands for subjective,. Documenting a patient assessment in the notes is something all medical students need to practice. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. It is the documentation used to record information about encounters with patients that follows a specific format. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method for documenting patient information in healthcare.
What is a Soap Note. According to Physiopedia SOAP notes are… by
Soap Meaning Nursing Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. It is the documentation used to record information about encounters with patients that follows a specific format. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Soap nursing notes are a type of patient progress note or nurse’s note. This guide discusses the soapframework (subjective, objective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Documenting a patient assessment in the notes is something all medical students need to practice.
From www.pinterest.com
SOAP Notes 101 Teaching Medical Charting! Great for Health Science Soap Meaning Nursing The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. It is the documentation. Soap Meaning Nursing.
From www.pinterest.com
Soap Note Template Nurse Practitioner Lovely What is A soap Note Soap Meaning Nursing Documenting a patient assessment in the notes is something all medical students need to practice. The acronym stands for subjective,. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap—or subjective, objective, assessment and plan—notes allow. Soap Meaning Nursing.
From www.pinterest.com
SOAP vs SBAR Nursing school survival, Nursing school tips, Nursing Soap Meaning Nursing Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers to document patient data more. Soap Meaning Nursing.
From www.flickr.com
The Role of SOAP Notes in Nursing Practice The SOAP note i… Flickr Soap Meaning Nursing Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. This guide discusses the soapframework (subjective, objective,. The subjective, objective, assessment. Soap Meaning Nursing.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Meaning Nursing Soap nursing notes are a type of patient progress note or nurse’s note. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Soap notes are a standardized method of documenting patient encounters in medical. Soap Meaning Nursing.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soapframework (subjective, objective,. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a standardized. Soap Meaning Nursing.
From www.pinterest.ca
SOAP Note Examples Occupational therapy quotes, Clinical social work Soap Meaning Nursing Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. This guide discusses the soapframework (subjective, objective,. Documenting a patient assessment in the notes is something all medical students need to practice. The subjective, objective, assessment and plan (soap) note is an. Soap Meaning Nursing.
From www.pinterest.com
Pin on Salud Soap Meaning Nursing Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. This guide discusses the soapframework (subjective, objective,. The acronym stands for subjective,. Soap notes are a. Soap Meaning Nursing.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Meaning Nursing Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Soap notes are a standardized method for documenting patient information in healthcare. This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap nursing notes are a type of patient progress note. Soap Meaning Nursing.
From www.carecloud.com
Free SOAP Notes Template CareCloud Continuum Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. It is the documentation used to. Soap Meaning Nursing.
From viewpoint.online
How to put the patient first in your eye examinations Viewpoint Soap Meaning Nursing Documenting a patient assessment in the notes is something all medical students need to practice. It is the documentation used to record information about encounters with patients that follows a specific format. The acronym stands for subjective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians. Soap Meaning Nursing.
From www.pinterest.ca
Soap Note Etsy Soap note, Nursing student tips, Nursing school notes Soap Meaning Nursing The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a standardized method for documenting patient information in healthcare. It is the documentation used to record information about encounters with patients that follows a specific. Soap Meaning Nursing.
From www.slideshare.net
Nursing Skills Charting Soap Meaning Nursing The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap nursing notes are a type of patient progress. Soap Meaning Nursing.
From www.slideserve.com
PPT Medical Records and Documentation PowerPoint Presentation, free Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soapframework (subjective, objective,. It is the documentation used to record information about encounters with patients that. Soap Meaning Nursing.
From www.youtube.com
How to Write SOAP Notes YouTube Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Documenting a patient assessment in the notes is something all. Soap Meaning Nursing.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. This guide discusses the soapframework (subjective, objective,. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and. Soap Meaning Nursing.
From in.pinterest.com
First Aid CPD SOAP 👀⠀ ⠀ SOAP is a medical acronym used to remember Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document. Soap Meaning Nursing.
From keski.condesan-ecoandes.org
soap charting Keski Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Documenting a patient assessment in the notes is something all medical students need to practice. The acronym stands for subjective,. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a standardized method of. Soap Meaning Nursing.
From www.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract Soap Meaning Nursing Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The acronym stands for subjective,. Documenting a patient assessment. Soap Meaning Nursing.
From topanswerideas.com
The Importance of Soap Notes in Well Woman Exams A Comprehensive Guide Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soapframework (subjective, objective,. Documenting a patient. Soap Meaning Nursing.
From www.osmosis.org
Administering an enema Clinical skills notes Osmosis Soap Meaning Nursing The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Documenting a patient assessment in the notes is. Soap Meaning Nursing.
From www.pinterest.com.au
progress soap nursing diagnosis Saferbrowser Image Search Results Soap Meaning Nursing This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method for documenting patient information in healthcare. It is the documentation used to record information about encounters with patients that follows a specific format. Documenting a patient assessment in the notes is something all medical students need to practice. The acronym stands for subjective,. Soap nursing notes are. Soap Meaning Nursing.
From quizzmediasophie.z13.web.core.windows.net
The E Entry In The Soaper Charting Method Means Soap Meaning Nursing Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap notes are a standardized method for documenting patient information. Soap Meaning Nursing.
From www.pinterest.com
Medical Mnemonics Diagnostic Criteria for SLE Soap Brain MD Soap Meaning Nursing It is the documentation used to record information about encounters with patients that follows a specific format. This guide discusses the soapframework (subjective, objective,. Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized. Soap Meaning Nursing.
From www.powerdiary.com
SOAP Notes for Occupational Therapy OT SOAP Note Examples Soap Meaning Nursing This guide discusses the soapframework (subjective, objective,. Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a standardized method for documenting patient information in healthcare. Soap nursing notes are a type of patient progress note or nurse’s note. The acronym stands for subjective,. Soap notes are a standardized method of documenting. Soap Meaning Nursing.
From studylib.net
Patient SOAP Note Charting Procedures Soap Meaning Nursing It is the documentation used to record information about encounters with patients that follows a specific format. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Documenting a patient assessment in. Soap Meaning Nursing.
From www.pinterest.com
Occupational Therapy Documentation Tips The OT Toolbox Occupational Soap Meaning Nursing It is the documentation used to record information about encounters with patients that follows a specific format. Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soapframework (subjective, objective,. The acronym stands for subjective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. Soap Meaning Nursing.
From www.registerednursern.com
How to Perform Hand Hygiene with Soap and Water Soap Meaning Nursing This guide discusses the soapframework (subjective, objective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Documenting a patient assessment in the notes is something all medical students need to practice. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap—or subjective, objective,. Soap Meaning Nursing.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education Soap Meaning Nursing Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. This guide discusses the soapframework (subjective, objective,. Documenting a patient assessment in the notes is something all medical students need to practice. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Soap nursing notes are a type. Soap Meaning Nursing.
From medium.com
Improve Patient Care The Importance of Accurate Nursing SOAP Notes Soap Meaning Nursing Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. Soap notes are a standardized method of documenting patient encounters in medical. Soap Meaning Nursing.
From www.pinterest.com
Nursing SOAP Note Example Nursing notes, Medical prescription, Soap note Soap Meaning Nursing Soap notes are a standardized method for documenting patient information in healthcare. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Documenting a patient assessment in the notes is something all medical students need to practice. Soap nursing notes are a type of patient progress note or nurse’s note. The acronym stands for. Soap Meaning Nursing.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners, Physician Soap Meaning Nursing Soap notes are a standardized method for documenting patient information in healthcare. Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes. Soap Meaning Nursing.
From www.theraplatform.com
Occupational therapy SOAP note Soap Meaning Nursing Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers to document patient data more. Soap Meaning Nursing.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Meaning Nursing Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. This guide discusses the soapframework (subjective, objective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap nursing notes are a type of patient progress note or nurse’s note. The subjective, objective, assessment and plan (soap) note is. Soap Meaning Nursing.
From www.pinterest.com
SOAP Notes Etsy Soap note, Nursing notes, Soap Soap Meaning Nursing Soap notes are a standardized method for documenting patient information in healthcare. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The. Soap Meaning Nursing.