Soap Notes Def . — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — what is a soap note? A soap note is a form of written documentation many healthcare professions use to. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many.
from mavink.com
soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note? A soap note is a form of written documentation many healthcare professions use to. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many.
Ejemplos De Notas Soap
Soap Notes Def soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. A soap note is a form of written documentation many healthcare professions use to. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note?
From www.browsegrades.net
PEDIATRIC FILLABLE SOAP NOTE TEMPLATE Browsegrades Soap Notes Def soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note is a form of written documentation many healthcare professions use to. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment. Soap Notes Def.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an. Soap Notes Def.
From www.pinterest.com
Jones Tasha Soap Note Complete soap Note in 2022 Dental exam, Soap Soap Notes Def — what is a soap note? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. A soap note is a form of written documentation many healthcare professions. Soap Notes Def.
From martinlindelof.com
Soap Notes Speech Therapy Martin Lindelof Soap Notes Def soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note? A soap. Soap Notes Def.
From datafinch-catalyst.zendesk.com
Create an Enhanced SOAP Note Template (Catalyst) Catalyst Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a. Soap Notes Def.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Notes Def soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. A soap note is a form of written documentation. Soap Notes Def.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a highly structured format for documenting the progress of. Soap Notes Def.
From www.studocu.com
Guide to writing SOAP Notes Over time, SOAP notes were adopted by Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many.. Soap Notes Def.
From www.studocu.com
Mixed Soapnote SOAP Note SOAP Note Form S/ Identifying Information Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. A soap note is a form of written documentation. Soap Notes Def.
From practicebetter.io
Mastering SOAP Notes as a Wellness Professional Practice Better Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap stands for. Soap Notes Def.
From www.pinterest.com
Image result for SOAP note examples Soap note, Dr orders, Internal Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of. Soap Notes Def.
From www.wordtemplatesonline.net
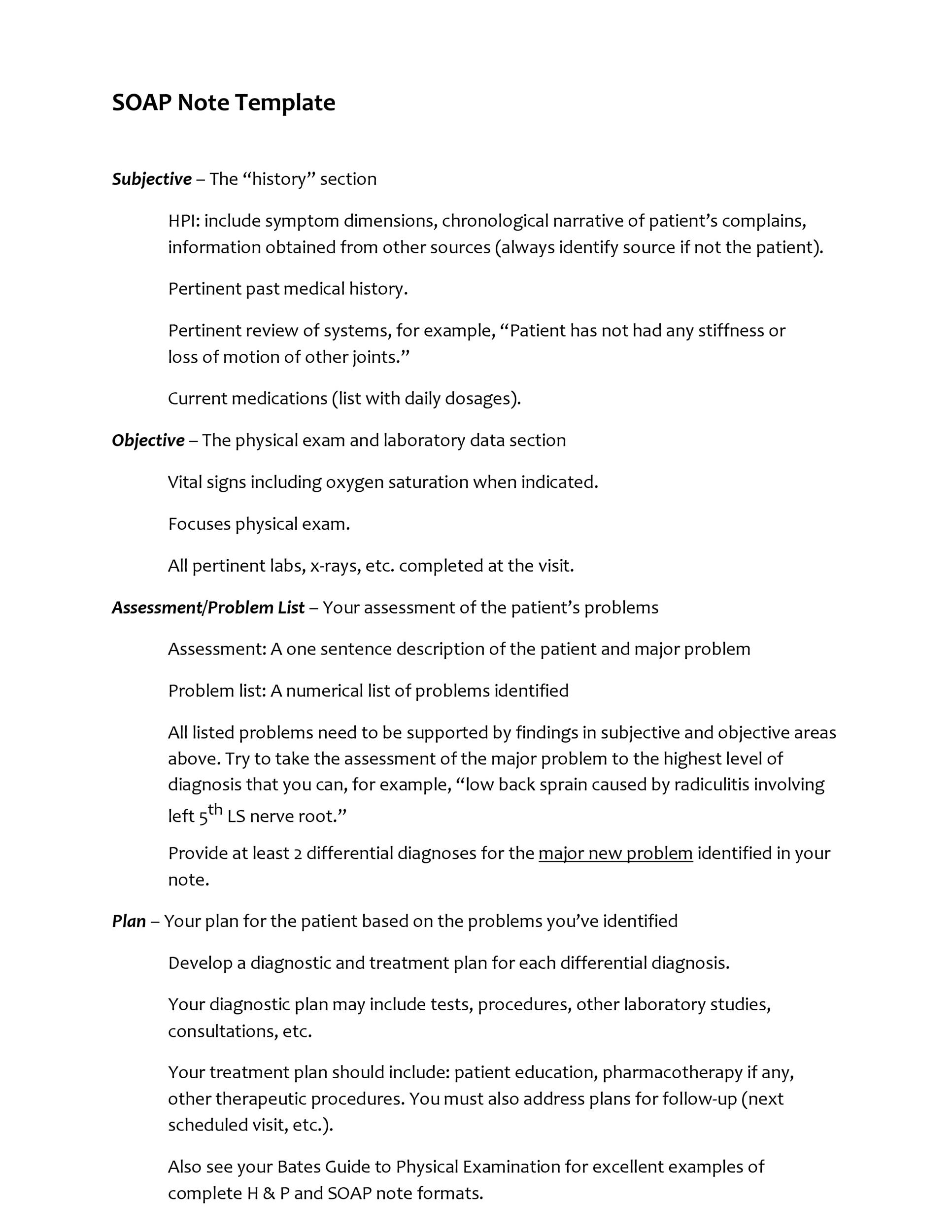
28 Best Soap Note Examples Free Templates Soap Notes Def soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap. Soap Notes Def.
From www.flickr.com
How SOAP Notes Enhance Communication in Healthcare Flickr Soap Notes Def soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — the subjective, objective, assessment and plan (soap). Soap Notes Def.
From clinicsense.com
How To Write Occupational Therapy SOAP Notes Soap Notes Def soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — what is a soap note? soap notes are a structured method for documenting patient information in healthcare settings, which stands for. soap notes are a highly structured format for documenting the progress of a patient during treatment and. Soap Notes Def.
From www.studocu.com
Depression soap note 1 Description Patient Information 68yearold Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note? soap notes are a highly. Soap Notes Def.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Soap Notes Def — what is a soap note? soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is a form of written documentation many healthcare professions use to. soap notes are a. Soap Notes Def.
From www.pinterest.com.au
SOAP Note Examples Soap note, Occupational therapy schools Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap notes are a structured method for documenting patient information in healthcare settings,. Soap Notes Def.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — what is a soap note? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only. Soap Notes Def.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — the subjective, objective, assessment and plan (soap). Soap Notes Def.
From www.scribd.com
Sample Soap Note PDF Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — what is a soap note? soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. . Soap Notes Def.
From mavink.com
Ejemplos De Notas Soap Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a structured method for documenting patient information in healthcare settings, which stands for. A soap note is a form of written documentation. Soap Notes Def.
From www.studocu.com
SOAP NOTEex 212 SOAP summary SOAP Notes Each student will complete Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. A soap note is a form of written documentation many healthcare professions use to. — what is a soap note? soap notes are a. Soap Notes Def.
From www.carepatron.com
SOAP Notes for Chiropractic Template & Example Free PDF Download Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — what is a soap note? A soap note is a form of written documentation many healthcare professions use to. soap stands for subjective, objective,. Soap Notes Def.
From canadianpa.ca
How to write a SOAP note — CANADIAN PA Soap Notes Def — what is a soap note? soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. — the subjective, objective,. Soap Notes Def.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Nutrition Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — what is a soap note? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap. Soap Notes Def.
From www.carepatron.com
SOAP Notes for ABA Template & Example Free PDF Download Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap notes are a. Soap Notes Def.
From www.studypool.com
SOLUTION Pediatric Soap Notes 3 Studypool Soap Notes Def soap notes are a structured method for documenting patient information in healthcare settings, which stands for. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a highly structured format for documenting. Soap Notes Def.
From globalccm.us
What Are SOAP Notes? Components How to Use Example Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — what is a soap note?. Soap Notes Def.
From therapistsmarket.com
Simple SOAP Note Template by a Licensed Therapist Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — what is a soap note? A soap note is a form of written documentation many healthcare professions use to. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are. Soap Notes Def.
From mavink.com
Ejemplos De Notas Soap Soap Notes Def soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note. Soap Notes Def.
From www.pinterest.de
SOAP notes are a standardized form of note taking that can serve as Soap Notes Def — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is a form of written documentation many healthcare professions use to. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — what is a soap. Soap Notes Def.
From clinicsense.com
Free SOAP Notes Template ClinicSense Soap Notes Def A soap note is a form of written documentation many healthcare professions use to. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a highly structured format for documenting the. Soap Notes Def.
From datafinch-catalyst.zendesk.com
Create an Enhanced SOAP Note Template (Catalyst) Catalyst Soap Notes Def soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. — what is a soap note? — the subjective, objective, assessment and plan (soap) note is an. Soap Notes Def.
From www.slideshare.net
SOAP Notes Dentistry Pages format Soap Notes Def — what is a soap note? soap notes are a structured method for documenting patient information in healthcare settings, which stands for. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. soap stands for subjective, objective, assessment, and plan—a standardized method for documenting. Soap Notes Def.
From npchartingschool.com
Examples of a SOAP note plus 7 tips for charting! Soap Notes Def — what is a soap note? soap stands for subjective, objective, assessment, and plan—a standardized method for documenting patient encounters within ehr software. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note is a form of written documentation many healthcare professions. Soap Notes Def.