Cvs Caremark Prior Authorization Form For Wegovy . Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When a pa is needed for a prescription, the member will be asked to have. Our employees are trained regarding the appropriate way to handle members’ private health information. When conditions are met, we will. Instructions for completing this form 1. • the requested drug will be used with a reduced. Submit a separate form for each medication. The requested drug will be covered with prior authorization when the following criteria are met: Your health care provider will need to submit a form to your insurance. When conditions are met, we will. Authorization does not guarantee payment.
from www.sampletemplates.com
• the requested drug will be used with a reduced. When a pa is needed for a prescription, the member will be asked to have. Instructions for completing this form 1. Authorization does not guarantee payment. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Submit a separate form for each medication. Your health care provider will need to submit a form to your insurance. The requested drug will be covered with prior authorization when the following criteria are met: Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. When conditions are met, we will.
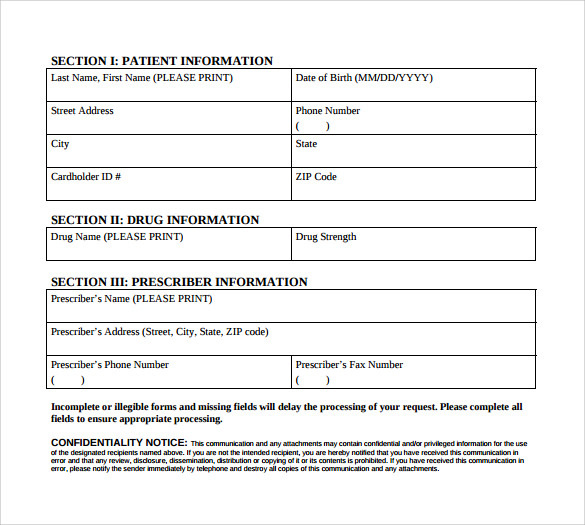
9+ Sample Caremark Prior Authorization Forms Sample Templates
Cvs Caremark Prior Authorization Form For Wegovy • the requested drug will be used with a reduced. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. The requested drug will be covered with prior authorization when the following criteria are met: Our employees are trained regarding the appropriate way to handle members’ private health information. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When conditions are met, we will. • the requested drug will be used with a reduced. When a pa is needed for a prescription, the member will be asked to have. Authorization does not guarantee payment. When conditions are met, we will. Submit a separate form for each medication. Your health care provider will need to submit a form to your insurance. Instructions for completing this form 1.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Form For . Cvs Caremark Prior Authorization Cvs Caremark Prior Authorization Form For Wegovy When a pa is needed for a prescription, the member will be asked to have. When conditions are met, we will. Your health care provider will need to submit a form to your insurance. Our employees are trained regarding the appropriate way to handle members’ private health information. Authorization does not guarantee payment. Submit a separate form for each medication.. Cvs Caremark Prior Authorization Form For Wegovy.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. Submit a separate form for each medication. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Our employees are trained regarding the appropriate way to handle members’ private health information. When a pa is needed for a prescription, the member will. Cvs Caremark Prior Authorization Form For Wegovy.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. Our employees are trained regarding the appropriate way to handle members’ private health information. When a pa is needed for a prescription, the member will be asked to have. Your health care provider will need to submit a form to your insurance. When conditions are met, we will. The requested drug will be covered. Cvs Caremark Prior Authorization Form For Wegovy.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Wegovy Authorization does not guarantee payment. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When conditions are met, we will. The requested drug will be covered with prior authorization when the following criteria. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form PDFeFormsCaremarkCaremarkPATIENT Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. Submit a separate form for each medication. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When conditions are met, we will. • the requested drug will be used with a reduced. Our employees are trained regarding the appropriate way to. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Prior Authorization Form For Wegovy When a pa is needed for a prescription, the member will be asked to have. Submit a separate form for each medication. • the requested drug will be used with a reduced. When conditions are met, we will. Your health care provider will need to submit a form to your insurance. Authorization does not guarantee payment. Has the patient completed. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form eForms Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy When conditions are met, we will. Authorization does not guarantee payment. Your health care provider will need to submit a form to your insurance. Submit a separate form for each medication. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Prior authorizations (pas) are required by some. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Cvs Caremark Formulary Exception Prior Authorization Request Form Fill Online, Printable Cvs Caremark Prior Authorization Form For Wegovy • the requested drug will be used with a reduced. When a pa is needed for a prescription, the member will be asked to have. When conditions are met, we will. Instructions for completing this form 1. Your health care provider will need to submit a form to your insurance. Our employees are trained regarding the appropriate way to handle. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When conditions are met, we will. Authorization does not guarantee payment. Submit a separate form for each medication. Instructions for completing this form 1.. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Prior Authorization Form For Wegovy • the requested drug will be used with a reduced. When conditions are met, we will. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Our employees are trained regarding the appropriate way to handle members’ private health information. Submit a separate form for each medication. Has the patient completed at least 16 weeks of. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Your health care provider will need to submit a form to your insurance. When conditions are met, we will. Our employees are trained regarding. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Caremark Prior Authorization Form Printable Pdf Download Cvs Caremark Prior Authorization Form For Wegovy • the requested drug will be used with a reduced. When a pa is needed for a prescription, the member will be asked to have. When conditions are met, we will. Submit a separate form for each medication. Instructions for completing this form 1. When conditions are met, we will. Prior authorizations (pas) are required by some prescription insurance plans. Cvs Caremark Prior Authorization Form For Wegovy.
From www.formsbank.com
Cvs Aveed Prior Authorization Request Form printable pdf download Cvs Caremark Prior Authorization Form For Wegovy When conditions are met, we will. When conditions are met, we will. Your health care provider will need to submit a form to your insurance. The requested drug will be covered with prior authorization when the following criteria are met: When a pa is needed for a prescription, the member will be asked to have. Submit a separate form for. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization HMSA Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy • the requested drug will be used with a reduced. When conditions are met, we will. When a pa is needed for a prescription, the member will be asked to have. When conditions are met, we will. Instructions for completing this form 1. Submit a separate form for each medication. The requested drug will be covered with prior authorization when. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy When conditions are met, we will. Submit a separate form for each medication. Our employees are trained regarding the appropriate way to handle members’ private health information. When a pa is needed for a prescription, the member will be asked to have. • the requested drug will be used with a reduced. When conditions are met, we will. Instructions for. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online wegovy prior authorization request prescriber fax form Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy Our employees are trained regarding the appropriate way to handle members’ private health information. Submit a separate form for each medication. The requested drug will be covered with prior authorization when the following criteria are met: • the requested drug will be used with a reduced. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications.. Cvs Caremark Prior Authorization Form For Wegovy.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Form For Wegovy When a pa is needed for a prescription, the member will be asked to have. The requested drug will be covered with prior authorization when the following criteria are met: Your health care provider will need to submit a form to your insurance. Submit a separate form for each medication. When conditions are met, we will. Prior authorizations (pas) are. Cvs Caremark Prior Authorization Form For Wegovy.
From www.templateroller.com
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online and Download PDF Cvs Caremark Prior Authorization Form For Wegovy Your health care provider will need to submit a form to your insurance. Instructions for completing this form 1. When a pa is needed for a prescription, the member will be asked to have. The requested drug will be covered with prior authorization when the following criteria are met: When conditions are met, we will. When conditions are met, we. Cvs Caremark Prior Authorization Form For Wegovy.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Form For Wegovy Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. When conditions are met, we will. • the requested drug will be used with a reduced. Authorization does not guarantee payment. Your health care provider will need to submit a form to your insurance. When a pa is needed for a prescription, the member will be. Cvs Caremark Prior Authorization Form For Wegovy.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form For Wegovy Your health care provider will need to submit a form to your insurance. Submit a separate form for each medication. Instructions for completing this form 1. The requested drug will be covered with prior authorization when the following criteria are met: Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Fax Email Print Cvs Caremark Prior Authorization Form For Wegovy Our employees are trained regarding the appropriate way to handle members’ private health information. Instructions for completing this form 1. • the requested drug will be used with a reduced. Your health care provider will need to submit a form to your insurance. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at. Cvs Caremark Prior Authorization Form For Wegovy.
From mungfali.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable E10 Cvs Caremark Prior Authorization Form For Wegovy Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When conditions are met, we will. Instructions for completing this form 1. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Submit a separate form for each medication. When conditions are met, we. Cvs Caremark Prior Authorization Form For Wegovy.
From www.dochub.com
Cvs caremark wegovy prior authorization criteria Fill out & sign online DocHub Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Your health care provider will need to submit a form to your insurance. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. When conditions are met, we. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Aetna Cvs Caremark Prior Authorization Form Cvs Caremark Prior Authorization Form For Wegovy Submit a separate form for each medication. Our employees are trained regarding the appropriate way to handle members’ private health information. Authorization does not guarantee payment. Instructions for completing this form 1. When conditions are met, we will. The requested drug will be covered with prior authorization when the following criteria are met: When conditions are met, we will. Has. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. When conditions are met, we will. • the requested drug will be used with a reduced. When conditions are met, we will. Our employees are trained regarding the appropriate way to handle members’ private health information. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a. Cvs Caremark Prior Authorization Form For Wegovy.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. When conditions are met, we will. • the requested drug will be used with a reduced. Authorization does not guarantee payment. Submit a separate form for each medication. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. When conditions are met, we will. When a pa is needed for. Cvs Caremark Prior Authorization Form For Wegovy.
From www.dochub.com
Caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form For Wegovy The requested drug will be covered with prior authorization when the following criteria are met: Instructions for completing this form 1. Submit a separate form for each medication. When a pa is needed for a prescription, the member will be asked to have. • the requested drug will be used with a reduced. Prior authorizations (pas) are required by some. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Cvs Caremark Ivig Prior Authorization Form Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. Submit a separate form for each medication. Our employees are trained regarding the appropriate way to handle members’ private health information. When a pa is needed for a prescription, the member will be asked to have. • the requested drug will be used with a reduced. Has the patient completed at least 16 weeks. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Authorization Form For Wegovy Authorization does not guarantee payment. When conditions are met, we will. • the requested drug will be used with a reduced. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. When conditions are met, we will. Our employees are trained regarding the appropriate way to handle members’. Cvs Caremark Prior Authorization Form For Wegovy.
From www.sampletemplates.com
9+ Sample Caremark Prior Authorization Forms Sample Templates Cvs Caremark Prior Authorization Form For Wegovy When a pa is needed for a prescription, the member will be asked to have. Your health care provider will need to submit a form to your insurance. When conditions are met, we will. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. • the requested drug. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Fill Online, Printable Fax Email Print Cvs Caremark Prior Authorization Form For Wegovy • the requested drug will be used with a reduced. Instructions for completing this form 1. When a pa is needed for a prescription, the member will be asked to have. Authorization does not guarantee payment. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. Your health care provider will need to submit a form. Cvs Caremark Prior Authorization Form For Wegovy.
From www.authorizationform.net
Cvs Caremark Synagis Prior Authorization Form Cvs Caremark Prior Authorization Form For Wegovy Authorization does not guarantee payment. The requested drug will be covered with prior authorization when the following criteria are met: When a pa is needed for a prescription, the member will be asked to have. • the requested drug will be used with a reduced. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. When. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Provider Resource Center Fax Email Print Cvs Caremark Prior Authorization Form For Wegovy Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Prior authorizations (pas) are required by some prescription insurance plans to cover certain medications. The requested drug will be covered with prior authorization when the following criteria are met: When conditions are met, we will. Submit a separate. Cvs Caremark Prior Authorization Form For Wegovy.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form For Wegovy Instructions for completing this form 1. Our employees are trained regarding the appropriate way to handle members’ private health information. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Authorization does not guarantee payment. • the requested drug will be used with a reduced. The requested drug. Cvs Caremark Prior Authorization Form For Wegovy.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Form Fax Email Print pdfFiller Cvs Caremark Prior Authorization Form For Wegovy Submit a separate form for each medication. Has the patient completed at least 16 weeks of therapy (saxenda, contrave), 3 months of therapy at a stable maintenance dose (wegovy,. Our employees are trained regarding the appropriate way to handle members’ private health information. Authorization does not guarantee payment. The requested drug will be covered with prior authorization when the following. Cvs Caremark Prior Authorization Form For Wegovy.