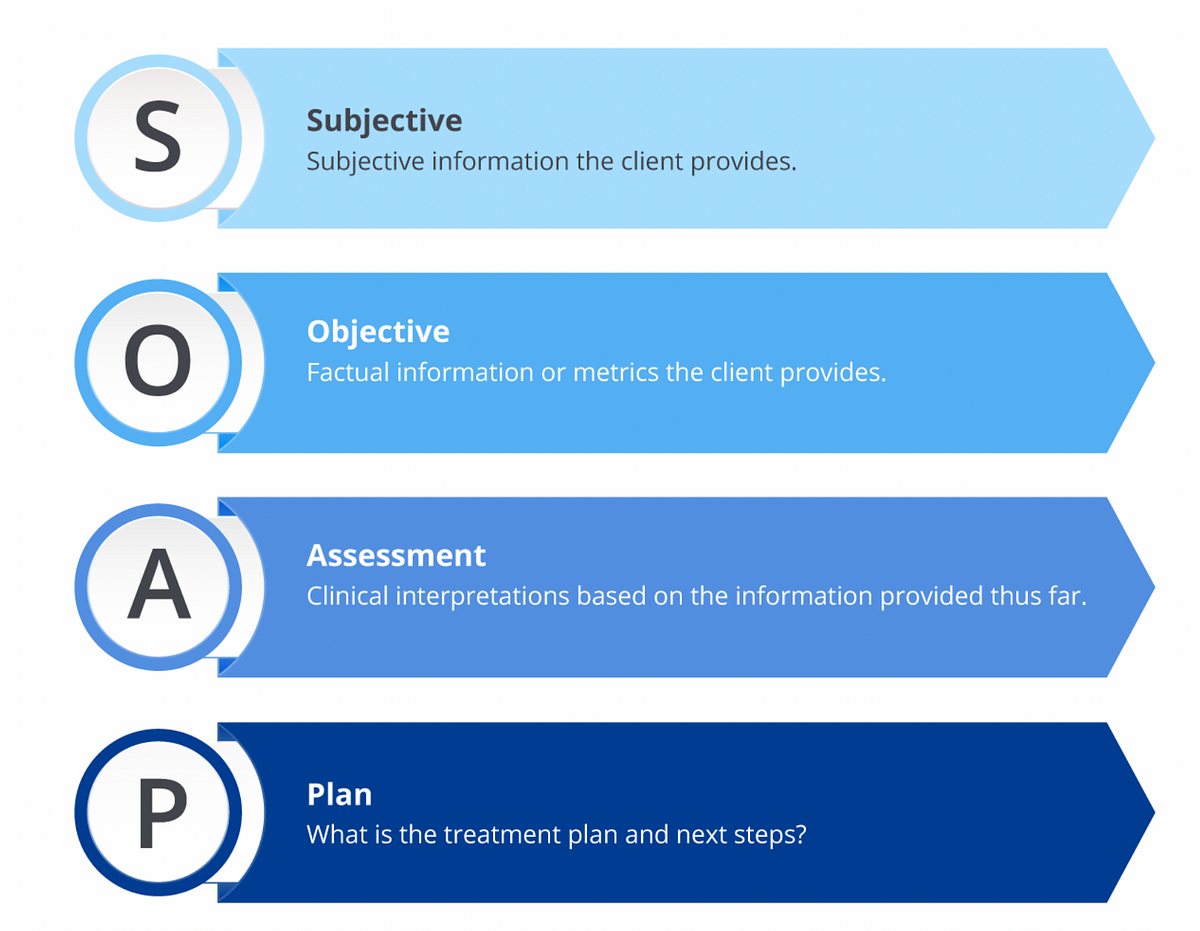
What Is Assessment In Soap . Soap is an acronym for: Each letter refers to one of four sections in the document. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. In the soap format, soap stands for subjective, objective, assessment, and plan.
from medium.com
Each letter refers to one of four sections in the document. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes.
What is a Soap Note. According to Physiopedia SOAP notes are… by
What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for.
From www.slideserve.com
PPT Injury Evaluation Basics PowerPoint Presentation, free download What Is Assessment In Soap Each letter refers to one of four sections in the document. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Soap is an acronym for: The subjective, objective,. What Is Assessment In Soap.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Here’s what you need to know about what goes. What Is Assessment In Soap.
From mavink.com
Ejemplo De Nota Soap What Is Assessment In Soap The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Each letter refers to one of four sections in the document. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The assessment section, also known as impression or diagnoses outside of. What Is Assessment In Soap.
From www.pinterest.com
Example of SOAP Note Soap note, Notes template, Medical history What Is Assessment In Soap Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap is an acronym for: The assessment section, also known as impression or diagnoses outside of cda, is. What Is Assessment In Soap.
From www.slideserve.com
PPT Patient Medical Records PowerPoint Presentation, free download What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Each letter refers to one of four sections in the document. Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a. What Is Assessment In Soap.
From www.youtube.com
SOAP Assessment Format(Part3)Soap Assessment & PlanPhysiotherapy What Is Assessment In Soap Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The assessment is the therapist's professional evaluation of the client’s condition, as. What Is Assessment In Soap.
From peaceofmindhomehealthcaref.blogspot.com
Soap Note Assessment Example Physical Therapy Peace Of Mind Home What Is Assessment In Soap Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Each letter. What Is Assessment In Soap.
From www.studocu.com
SOAP guide Subjective, Objective, Assessment, Plan SOAP INITIAL What Is Assessment In Soap The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The assessment is the therapist's professional evaluation of the client’s. What Is Assessment In Soap.
From www.studocu.com
Soap (subjective, objective, assessment, and plan) notes template What Is Assessment In Soap The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Here’s what. What Is Assessment In Soap.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by What Is Assessment In Soap Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. The assessment. What Is Assessment In Soap.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment,. What Is Assessment In Soap.
From www.slideteam.net
Comparative Assessment Of Soap And Rest API Testing What Is Assessment In Soap Each letter refers to one of four sections in the document. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The assessment section, also. What Is Assessment In Soap.
From mikekelvin.home.blog
Reasons why SAP S4HANA assessment is important? What Is Assessment In Soap Soap is an acronym for: Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Each letter refers to one of four sections in the document. In the soap. What Is Assessment In Soap.
From musculoskeletalkey.com
Treatment Notes and Progress Notes Using a Modified SOAP Format What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The assessment section,. What Is Assessment In Soap.
From www.wikihow.com
How to Write a Soap Note (with Pictures) wikiHow What Is Assessment In Soap Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: Each letter refers to one of four sections in the document. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. In the soap format,. What Is Assessment In Soap.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Each letter. What Is Assessment In Soap.
From topanswerideas.com
The Importance of Soap Notes in Well Woman Exams A Comprehensive Guide What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. Here’s what you need to. What Is Assessment In Soap.
From www.slideserve.com
PPT Sports Injury Assessment PowerPoint Presentation, free download What Is Assessment In Soap The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Here’s what you need to know about what goes. What Is Assessment In Soap.
From www.theraplatform.com
Occupational therapy SOAP note What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: Each letter refers. What Is Assessment In Soap.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] What Is Assessment In Soap Each letter refers to one of four sections in the document. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The assessment is the therapist's professional evaluation of the client’s. What Is Assessment In Soap.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example What Is Assessment In Soap Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Each letter refers to one of four sections in the document. Soap is an acronym for: The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The subjective, objective, assessment. What Is Assessment In Soap.
From clinicsense.com
How To Write Occupational Therapy SOAP Notes What Is Assessment In Soap The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Each letter refers to one of four sections in the document. The assessment section, also known as impression or diagnoses outside of. What Is Assessment In Soap.
From www.studocu.com
Comprehensive SOAP Exemplar Comprehensive SOAP Exemplar Purpose To What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. In the soap format, soap stands for subjective, objective, assessment, and plan. The assessment section, also known as impression or. What Is Assessment In Soap.
From www.slideserve.com
PPT Lesson 1.8 The SOAP Note PowerPoint Presentation, free download What Is Assessment In Soap Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: The assessment section,. What Is Assessment In Soap.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary What Is Assessment In Soap The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Each letter refers to one of four sections in the document. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. The assessment section, also known as impression or diagnoses outside of. What Is Assessment In Soap.
From www.pinterest.ca
an image of a computer user's profile page What Is Assessment In Soap Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Soap. What Is Assessment In Soap.
From nursing-professor.com
SOAP Note for Stroke Nursing Professor What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Each letter refers to one of four sections. What Is Assessment In Soap.
From www.pinterest.nz
Infographic S.O.A.P. Notes Vet tech student, Vet tech school What Is Assessment In Soap The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective,. What Is Assessment In Soap.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Each letter refers to one of four sections in the document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. What Is Assessment In Soap.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide What Is Assessment In Soap Each letter refers to one of four sections in the document. The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The subjective, objective, assessment and plan (soap) note. What Is Assessment In Soap.
From kelitbanganwonogiri.org
Soap Assessment Template What Is Assessment In Soap The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections. What Is Assessment In Soap.
From happiertherapy.com
SOAP Assessment Template HappierTHERAPY What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Each letter refers. What Is Assessment In Soap.
From www.studocu.com
Health Assessment Skin Condition SOAP NOTE Differential Diagnosis for What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. Soap is an acronym for: The assessment section, also known as impression or diagnoses outside of cda, is a crucial component of the soap notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Here’s what you need. What Is Assessment In Soap.
From www.lmteq.com
What is SAP S/4 HANA Assessment and what are its benefits? SAP What Is Assessment In Soap Each letter refers to one of four sections in the document. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. In the soap format, soap stands for subjective, objective,. What Is Assessment In Soap.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox What Is Assessment In Soap In the soap format, soap stands for subjective, objective, assessment, and plan. Here’s what you need to know about what goes in the soap note assessment section, along with soap note assessment examples. Soap is an acronym for: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The assessment section,. What Is Assessment In Soap.