Example Of Subjective In Soap Note . Understanding how to write the subjective. Subjective, objective, assessment, and plan. There are four basic components of a soap note: The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. The acronym soap lays out the four sections of the note: Record the patient's verbal description of their symptoms and medical history. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Ensure to capture the patient's own. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),.
from sampletemplates.com
Subjective, objective, assessment, and plan. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. A soap note is standard across all types of chart notes and can be used in any area of healthcare. The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. The acronym soap lays out the four sections of the note: There are four basic components of a soap note: Ensure to capture the patient's own. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Subjective, objective, assessment, and plan.
8+ Sample Subjective Objective Assessment Planning Notes Sample Templates
Example Of Subjective In Soap Note There are four basic components of a soap note: Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. There are four basic components of a soap note: We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. Ensure to capture the patient's own. The acronym soap lays out the four sections of the note: If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Record the patient's verbal description of their symptoms and medical history. Subjective, objective, assessment, and plan. Understanding how to write the subjective. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),.
From studylib.net
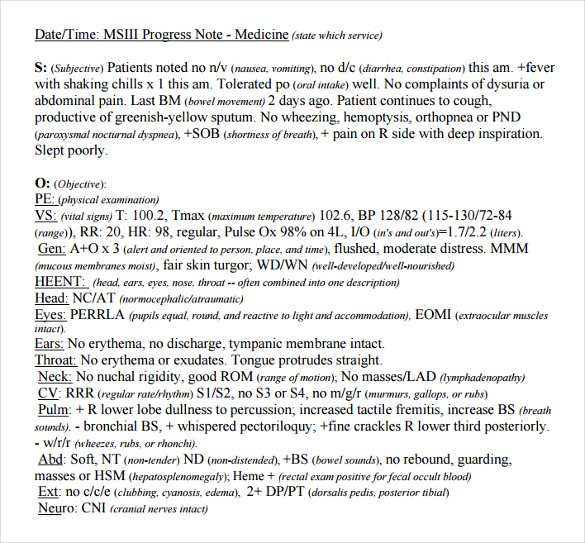
Patient SOAP Note Charting Procedures Example Of Subjective In Soap Note There are four basic components of a soap note: The acronym soap lays out the four sections of the note: A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment, and plan. Subjective, objective, assessment, and plan. Record the patient's verbal description of their symptoms and medical. Example Of Subjective In Soap Note.
From sampletemplates.com
8+ Sample Subjective Objective Assessment Planning Notes Sample Templates Example Of Subjective In Soap Note A soap note is standard across all types of chart notes and can be used in any area of healthcare. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. Subjective, objective,. Example Of Subjective In Soap Note.
From practicebetter.io
Mastering SOAP Notes as a Wellness Professional Practice Better Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. We will break down each component of a soap note and explain how to write a soap note. Record the patient's verbal description of their symptoms and medical history. The subjective section is where you document what. Example Of Subjective In Soap Note.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. Ensure to capture the patient's own. A soap note is standard across all types of chart notes and can be used in any area of healthcare. If you’re looking for an example for writing soap notes, here’s. Example Of Subjective In Soap Note.
From sampletemplates.com
8+ Sample Subjective Objective Assessment Planning Notes Sample Templates Example Of Subjective In Soap Note Ensure to capture the patient's own. Record the patient's verbal description of their symptoms and medical history. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. There are four basic components of a soap note: The subjective section is where you document what your client is telling you about. Example Of Subjective In Soap Note.
From www.sampletemplates.com
FREE 9+ Sample Subjective Objective Assessment Planning Notes in PDF Example Of Subjective In Soap Note We will break down each component of a soap note and explain how to write a soap note. There are four basic components of a soap note: Subjective, objective, assessment, and plan. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. The acronym soap lays out the four sections of the. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Example Of Subjective In Soap Note The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. We will break down each component of a soap note and explain how to write a soap note. Understanding how to write the subjective. Record the patient's verbal description of their symptoms and medical history. Despite the potential. Example Of Subjective In Soap Note.
From sampletemplates.com
8+ Sample Subjective Objective Assessment Planning Notes Sample Templates Example Of Subjective In Soap Note We will break down each component of a soap note and explain how to write a soap note. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Understanding how to write the subjective. There are four basic components of a soap note: Soap notes include a statement about relevant. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Example Of Subjective In Soap Note The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. There are four basic components of a soap note: Ensure to capture the patient's own. The acronym soap lays out the four sections of the note: Understanding how to write the subjective. Subjective, objective, assessment, and plan. Record. Example Of Subjective In Soap Note.
From mavink.com
Ejemplo De Nota Soap Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. Ensure to capture the patient's own. Understanding how to write the subjective. Subjective, objective, assessment, and plan. A soap note is standard across all types of chart notes and can be used in. Example Of Subjective In Soap Note.
From www.wordtemplatesonline.net
How to Write a SOAP Note (with SOAP Note Examples) Example Of Subjective In Soap Note Understanding how to write the subjective. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. The acronym soap lays out the four sections of the note: A soap note is standard across all types of chart notes and can be used in any area of healthcare. The subjective section is where. Example Of Subjective In Soap Note.
From template.mapadapalavra.ba.gov.br
Occupational Therapy Soap Note Template Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment, and plan. We will break down each component of a soap note and explain how to write a soap note. If you’re looking for an example for writing soap notes, here’s a. Example Of Subjective In Soap Note.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. Subjective, objective, assessment, and plan. There are four basic components of a soap. Example Of Subjective In Soap Note.
From www.studocu.com
Asthma SOAP Note soap note S.O.A. Note Template Case ID 005 Example Of Subjective In Soap Note The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. There are four basic components of a soap note: Subjective, objective, assessment, and plan. Subjective, objective, assessment, and plan. Soap. Example Of Subjective In Soap Note.
From www.studocu.com
Soap (subjective, objective, assessment, and plan) notes template Example Of Subjective In Soap Note Understanding how to write the subjective. Record the patient's verbal description of their symptoms and medical history. Subjective, objective, assessment, and plan. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. Subjective, objective, assessment, and plan. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. Example Of Subjective In Soap Note.
From sampletemplates.com
8+ Sample Subjective Objective Assessment Planning Notes Sample Templates Example Of Subjective In Soap Note There are four basic components of a soap note: Subjective, objective, assessment, and plan. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. The acronym soap lays out the four sections of the note: Understanding how to write the subjective. Despite the potential to vary their style format, all. Example Of Subjective In Soap Note.
From www.tutorsploit.com
How to Write SOAP NotesWith Examples Tutorsploit Example Of Subjective In Soap Note We will break down each component of a soap note and explain how to write a soap note. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. The acronym soap lays out the four sections of the note: Record the patient's verbal description of their symptoms and medical history. There are. Example Of Subjective In Soap Note.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Example Of Subjective In Soap Note Understanding how to write the subjective. We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. Ensure to capture the patient's own. Despite the potential. Example Of Subjective In Soap Note.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. Understanding how to write the subjective. Subjective, objective, assessment, and plan. Record the patient's verbal description of their symptoms and medical history. A soap note is standard across all types of chart notes and can be used in any area of healthcare. The acronym soap lays out the four sections of the note: We will. Example Of Subjective In Soap Note.
From doctemplates.us
Soap Note Subjective Example DocTemplates Example Of Subjective In Soap Note Ensure to capture the patient's own. There are four basic components of a soap note: A soap note is standard across all types of chart notes and can be used in any area of healthcare. Understanding how to write the subjective. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral. Example Of Subjective In Soap Note.
From www.slideserve.com
PPT SOAP Notes PowerPoint Presentation, free download ID1111245 Example Of Subjective In Soap Note Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. There are four basic components of a soap note: Subjective, objective, assessment, and plan. Record the patient's verbal description of their symptoms and medical history. A soap note is standard across all types of chart notes and can be used in any. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Example Of Subjective In Soap Note There are four basic components of a soap note: The acronym soap lays out the four sections of the note: Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. Subjective, objective,. Example Of Subjective In Soap Note.
From www.scribd.com
Sample Soap Note Subjective PDF Example Of Subjective In Soap Note Record the patient's verbal description of their symptoms and medical history. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Ensure to capture the patient's own. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Despite the potential to vary. Example Of Subjective In Soap Note.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Example Of Subjective In Soap Note Record the patient's verbal description of their symptoms and medical history. Ensure to capture the patient's own. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We will break down each component of a soap note and explain how to write a soap note. Understanding how to write the subjective. Despite. Example Of Subjective In Soap Note.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Example Of Subjective In Soap Note Record the patient's verbal description of their symptoms and medical history. The acronym soap lays out the four sections of the note: If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. Subjective, objective, assessment, and plan. Despite the potential to vary their style format, all soap notes must include. Example Of Subjective In Soap Note.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Example Of Subjective In Soap Note We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. There are four basic components of a soap note: Understanding how to write the subjective. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. Subjective, objective, assessment, and. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Example Of Subjective In Soap Note Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Record the patient's verbal description of their symptoms and medical history. Subjective, objective, assessment, and plan. The acronym soap lays out the four sections of the note: If you’re looking for an example for writing soap notes, here’s a soap format example. Example Of Subjective In Soap Note.
From doctemplates.us
Soap Note Subjective Example DocTemplates Example Of Subjective In Soap Note Ensure to capture the patient's own. A soap note is standard across all types of chart notes and can be used in any area of healthcare. There are four basic components of a soap note: Subjective, objective, assessment, and plan. Subjective, objective, assessment, and plan. Record the patient's verbal description of their symptoms and medical history. Despite the potential to. Example Of Subjective In Soap Note.
From clinicsense.com
How To Write Occupational Therapy SOAP Notes Example Of Subjective In Soap Note We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. There are four basic components of a soap note: Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Record the patient's verbal description of their symptoms and medical. Example Of Subjective In Soap Note.
From www.slideserve.com
PPT Lesson 1.8 The SOAP Note PowerPoint Presentation, free download Example Of Subjective In Soap Note Record the patient's verbal description of their symptoms and medical history. Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. Ensure to capture the patient's own. Understanding how to write the subjective. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral. Example Of Subjective In Soap Note.
From www.wikihow.com
How to Write a Soap Note (with Pictures) wikiHow Example Of Subjective In Soap Note The acronym soap lays out the four sections of the note: Subjective, objective, assessment, and plan. Ensure to capture the patient's own. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Record the patient's verbal description of their symptoms and medical history. Subjective, objective, assessment, and plan. Understanding how. Example Of Subjective In Soap Note.
From www.sampletemplates.com
FREE 8+ SOAP Note Samples in PDF, Word Example Of Subjective In Soap Note Despite the potential to vary their style format, all soap notes must include subjective, objective, assessment, and plan. The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms. There are four basic components of a soap note: A soap note is standard across all types of chart notes. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Example Of Subjective In Soap Note There are four basic components of a soap note: Subjective, objective, assessment, and plan. If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. We will break down each component of a soap note and explain how to write a soap note. The subjective section is where you document what. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Example Of Subjective In Soap Note Understanding how to write the subjective. There are four basic components of a soap note: If you’re looking for an example for writing soap notes, here’s a soap format example that may help behavioral health. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Soap notes include a statement. Example Of Subjective In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Example Of Subjective In Soap Note Subjective, objective, assessment, and plan. There are four basic components of a soap note: Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. Ensure to capture the patient's. Example Of Subjective In Soap Note.