Soap Note Objective Example . Here are soap note examples. It is the documentation used to record information about encounters with patients. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. the objective section of the soap notes includes patient data collected through tests, measurements, and. soap notes include a statement about relevant client behaviors or status (subjective), observable,. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes are a specific format for writing progress notes as a behavioral health clinician. wondering how to write soap notes? Getting the soap format right is essential for therapists.
from templatelab.com
soap notes are a specific format for writing progress notes as a behavioral health clinician. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. It is the documentation used to record information about encounters with patients. soap notes include a statement about relevant client behaviors or status (subjective), observable,. Getting the soap format right is essential for therapists. soap nursing notes are a type of patient progress note or nurse’s note. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. They contain four primary sections, represented by its. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. Here are soap note examples.
40 Fantastic SOAP Note Examples & Templates Template Lab
Soap Note Objective Example here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. wondering how to write soap notes? soap notes include a statement about relevant client behaviors or status (subjective), observable,. They contain four primary sections, represented by its. the objective section of the soap notes includes patient data collected through tests, measurements, and. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. Here are soap note examples. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Getting the soap format right is essential for therapists.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. the objective section of the soap notes includes patient data collected through tests, measurements, and. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap (subjective, objective, assessment, plan) notes provide a comprehensive. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable,. They contain four primary sections, represented by its. Here are soap note examples. Getting the soap format right is essential for therapists. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. soap notes are a specific format. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example Here are soap note examples. It is the documentation used to record information about encounters with patients. soap notes include a statement about relevant client behaviors or status (subjective), observable,. wondering how to write soap notes? They contain four primary sections, represented by its. here’s how to write the objective in soap notes, what information to include,. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Objective Example soap notes are a specific format for writing progress notes as a behavioral health clinician. the objective section of the soap notes includes patient data collected through tests, measurements, and. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. Getting the soap format right is essential for therapists. Here are. Soap Note Objective Example.
From www.studocu.com
Asthma SOAP Note soap note S.O.A. Note Template Case ID 005 Subjective Objective Soap Note Objective Example Getting the soap format right is essential for therapists. It is the documentation used to record information about encounters with patients. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. Here are soap note examples. They contain four primary sections, represented by its. The subjective, objective, assessment and plan (soap) note is. Soap Note Objective Example.
From www.carepatron.com
SOAP Progress Notes Template & Example Free PDF Download Soap Note Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable,. It is the documentation used to record information about encounters with patients. soap nursing notes are a type of patient progress note or nurse’s note. Here are soap note examples. soap notes are a specific format for writing progress notes as a behavioral health. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example It is the documentation used to record information about encounters with patients. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. Getting the soap format right is essential for therapists. soap notes are a specific format for writing progress notes as a behavioral health clinician. here’s how to write the. Soap Note Objective Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Note Objective Example wondering how to write soap notes? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its. It is the documentation used to record information about encounters with patients. . Soap Note Objective Example.
From www.printabletemplateslab.com
10+ Soap Note Template Free Download Word, Excel, PDF Format!! Soap Note Objective Example Here are soap note examples. It is the documentation used to record information about encounters with patients. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. soap notes. Soap Note Objective Example.
From moussyusa.com
46+ Free Download SOAP Note Template for Your Medical Note Mous Syusa Soap Note Objective Example the objective section of the soap notes includes patient data collected through tests, measurements, and. wondering how to write soap notes? They contain four primary sections, represented by its. Here are soap note examples. soap notes include a statement about relevant client behaviors or status (subjective), observable,. soap (subjective, objective, assessment, plan) notes provide a comprehensive. Soap Note Objective Example.
From www.wordtemplatesonline.net
35+ SOAP Note Examples (Blank Formats & Writing Tips) Soap Note Objective Example soap notes are a specific format for writing progress notes as a behavioral health clinician. soap nursing notes are a type of patient progress note or nurse’s note. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. It is the documentation used to record. Soap Note Objective Example.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Progress Notes Social Work Portal Soap Note Objective Example the objective section of the soap notes includes patient data collected through tests, measurements, and. soap notes are a specific format for writing progress notes as a behavioral health clinician. wondering how to write soap notes? here’s how to write the objective in soap notes, what information to include, and examples of what to put in. Soap Note Objective Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Note Objective Example It is the documentation used to record information about encounters with patients. They contain four primary sections, represented by its. soap notes include a statement about relevant client behaviors or status (subjective), observable,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap notes are a specific format for. Soap Note Objective Example.
From ncmin.org
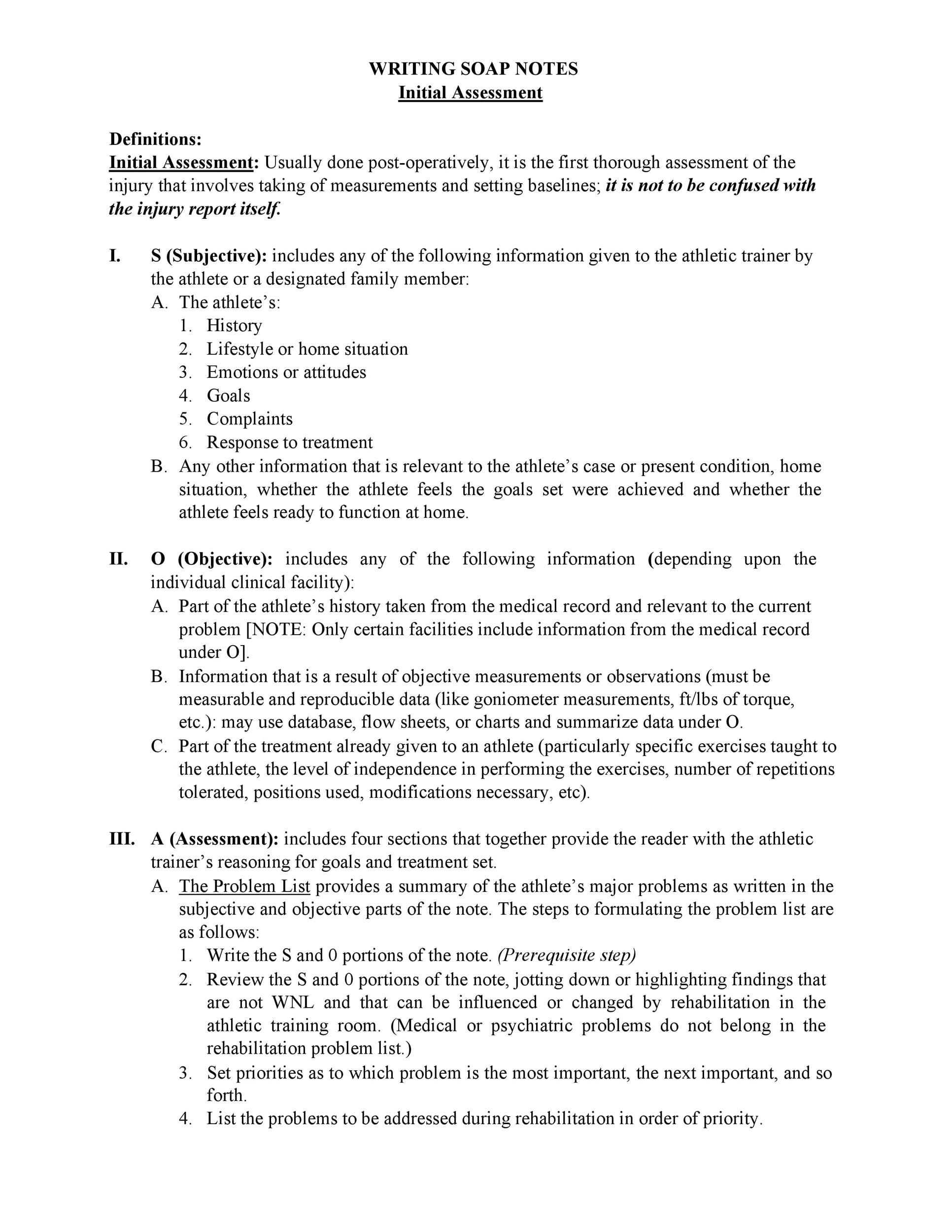
Writing Soap Notes SOAP Note and Documentation Templates & Examples Soap Note Objective Example Here are soap note examples. soap notes include a statement about relevant client behaviors or status (subjective), observable,. the objective section of the soap notes includes patient data collected through tests, measurements, and. Getting the soap format right is essential for therapists. They contain four primary sections, represented by its. It is the documentation used to record information. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example the objective section of the soap notes includes patient data collected through tests, measurements, and. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. soap nursing notes are a type of patient progress note or nurse’s note. here’s how to write the objective in soap notes, what information to. Soap Note Objective Example.
From www.studocu.com
Soap Note 1 Soap Note SOAP NOTE 1 Clinical Objective Clinical Objective To document in a Soap Note Objective Example wondering how to write soap notes? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. Getting the soap format right is essential for therapists. They contain four primary sections, represented by its. . Soap Note Objective Example.
From mavink.com
Ejemplo De Nota Soap Soap Note Objective Example Getting the soap format right is essential for therapists. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Here are soap note examples. They contain four primary sections, represented by its. wondering how to write soap notes? here’s how to write the objective in soap notes, what information to. Soap Note Objective Example.
From www.sampletemplates.com
16+ Sample SOAP Note Examples PDF, Word Sample Templates Soap Note Objective Example the objective section of the soap notes includes patient data collected through tests, measurements, and. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap nursing notes are a type of patient progress note or nurse’s note. soap notes are a specific format for writing progress notes as. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example It is the documentation used to record information about encounters with patients. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its. Here are soap note examples. soap notes. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example soap notes are a specific format for writing progress notes as a behavioral health clinician. wondering how to write soap notes? soap notes include a statement about relevant client behaviors or status (subjective), observable,. They contain four primary sections, represented by its. soap nursing notes are a type of patient progress note or nurse’s note. . Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Objective Example here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. Getting the soap format right is essential for therapists. soap notes include a statement about relevant client behaviors or status (subjective), observable,. It is the documentation used to record information about encounters with patients. soap. Soap Note Objective Example.
From doctemplates.us
Soap Note Objective Example DocTemplates Soap Note Objective Example the objective section of the soap notes includes patient data collected through tests, measurements, and. Here are soap note examples. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. It is the documentation used to record information about encounters with patients. wondering how to write soap notes? Getting the. Soap Note Objective Example.
From doctemplates.us
Soap Note Objective Example DocTemplates Soap Note Objective Example They contain four primary sections, represented by its. Here are soap note examples. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. the objective section of the soap. Soap Note Objective Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Note Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable,. soap nursing notes are a type of patient progress note or nurse’s note. wondering how to write soap notes? Getting the soap format right is essential for therapists. here’s how to write the objective in soap notes, what information to include, and examples. Soap Note Objective Example.
From studylib.net
Patient SOAP Note Charting Procedures Soap Note Objective Example Getting the soap format right is essential for therapists. soap nursing notes are a type of patient progress note or nurse’s note. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. They contain four primary sections, represented by its. It is the documentation used to. Soap Note Objective Example.
From doctemplates.us
Soap Note Objective Example DocTemplates Soap Note Objective Example the objective section of the soap notes includes patient data collected through tests, measurements, and. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap notes include a statement about relevant client behaviors or status (subjective), observable,. wondering how to write soap notes? It is the documentation used. Soap Note Objective Example.
From musculoskeletalkey.com
Treatment Notes and Progress Notes Using a Modified SOAP Format Musculoskeletal Key Soap Note Objective Example soap nursing notes are a type of patient progress note or nurse’s note. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes include a statement about relevant client behaviors or status (subjective), observable,. The subjective, objective, assessment and plan (soap) note is. Soap Note Objective Example.
From www.carepatron.com
SOAP Notes for ABA Template & Example Free PDF Download Soap Note Objective Example soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. Getting the soap format right is essential for therapists. wondering how to write soap notes? soap notes include a statement about relevant client behaviors or status (subjective), observable,. the objective section of the soap notes includes patient data collected through. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example soap nursing notes are a type of patient progress note or nurse’s note. Here are soap note examples. They contain four primary sections, represented by its. It is the documentation used to record information about encounters with patients. Getting the soap format right is essential for therapists. the objective section of the soap notes includes patient data collected. Soap Note Objective Example.
From doctemplates.us
Objective Soap Note Example DocTemplates Soap Note Objective Example here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. It is the documentation used to record information about encounters with patients. Here are soap note examples. Getting the soap format right is essential for therapists. soap notes are a specific format for writing progress notes. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Objective Example soap notes are a specific format for writing progress notes as a behavioral health clinician. the objective section of the soap notes includes patient data collected through tests, measurements, and. Getting the soap format right is essential for therapists. wondering how to write soap notes? It is the documentation used to record information about encounters with patients.. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable,. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. They contain four primary sections,. Soap Note Objective Example.
From www.pinterest.com.au
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely Soap Note Objective Example Getting the soap format right is essential for therapists. the objective section of the soap notes includes patient data collected through tests, measurements, and. It is the documentation used to record information about encounters with patients. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap nursing notes are a type. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Objective Example wondering how to write soap notes? the objective section of the soap notes includes patient data collected through tests, measurements, and. soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Here are. Soap Note Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Objective Example Here are soap note examples. It is the documentation used to record information about encounters with patients. wondering how to write soap notes? soap nursing notes are a type of patient progress note or nurse’s note. the objective section of the soap notes includes patient data collected through tests, measurements, and. soap notes are a specific. Soap Note Objective Example.