Acronym Soap Charting . Any palliating or provoking factors. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The onset of the patient’s symptoms. Where a client’s subjective experiences, feelings, or perspectives are recorded. To standardize your reporting across notes, include information using the acronym opqrst: In this article, the soap or soapie method will be described. Soap nursing notes are a type of patient progress note or nurse’s note. Nurses spend a lot of time. It is the documentation used to record information about encounters with.
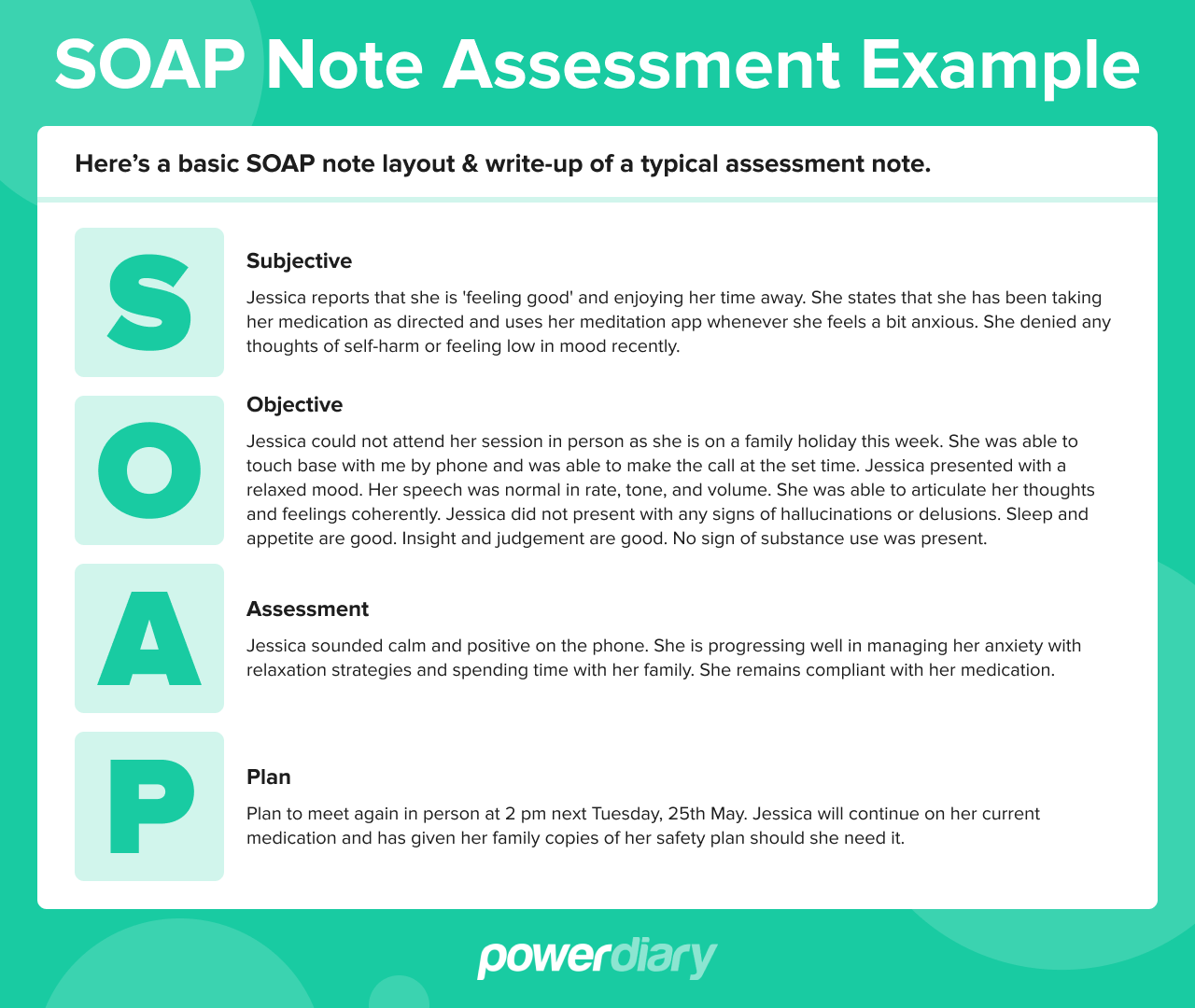
from www.powerdiary.com
Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with. Nurses spend a lot of time. Soap nursing notes are a type of patient progress note or nurse’s note. In this article, the soap or soapie method will be described. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: To standardize your reporting across notes, include information using the acronym opqrst: The onset of the patient’s symptoms. Any palliating or provoking factors.
Essential Guide to SOAP Notes SOAP Notes Example
Acronym Soap Charting In this article, the soap or soapie method will be described. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or perspectives are recorded. In this article, the soap or soapie method will be described. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Nurses spend a lot of time. It is the documentation used to record information about encounters with. Any palliating or provoking factors. The onset of the patient’s symptoms. Soap nursing notes are a type of patient progress note or nurse’s note. To standardize your reporting across notes, include information using the acronym opqrst:
From www.etsy.com
SOAP Notes Etsy Acronym Soap Charting It is the documentation used to record information about encounters with. Nurses spend a lot of time. Any palliating or provoking factors. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or. Acronym Soap Charting.
From slideplayer.com
Chapter 6 Documentation ppt download Acronym Soap Charting In this article, the soap or soapie method will be described. Nurses spend a lot of time. It is the documentation used to record information about encounters with. Soap is an acronym for the 4 sections, or headings, that each progress note contains: The onset of the patient’s symptoms. Soap notes are a way for healthcare providers to document patient. Acronym Soap Charting.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Acronym Soap Charting Any palliating or provoking factors. Where a client’s subjective experiences, feelings, or perspectives are recorded. Nurses spend a lot of time. To standardize your reporting across notes, include information using the acronym opqrst: The onset of the patient’s symptoms. Soap nursing notes are a type of patient progress note or nurse’s note. Soap is an acronym for the 4 sections,. Acronym Soap Charting.
From www.valant.io
What Are SOAP Notes and How Do You Write Them? Valant Acronym Soap Charting To standardize your reporting across notes, include information using the acronym opqrst: It is the documentation used to record information about encounters with. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Nurses spend a lot of time. Soap nursing notes are a type of patient progress note or nurse’s note. In this article,. Acronym Soap Charting.
From www.vrogue.co
How To Write A Soap Note With Soap Note Examples vrogue.co Acronym Soap Charting Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Where a client’s subjective experiences, feelings, or perspectives are recorded. The onset of the patient’s symptoms. Nurses spend a lot of time. Any palliating or provoking factors. In this. Acronym Soap Charting.
From lucadavies.z19.web.core.windows.net
The R Entry In The Soaper Charting Method Means Acronym Soap Charting Where a client’s subjective experiences, feelings, or perspectives are recorded. In this article, the soap or soapie method will be described. Nurses spend a lot of time. Soap nursing notes are a type of patient progress note or nurse’s note. Any palliating or provoking factors. It is the documentation used to record information about encounters with. Soap notes are a. Acronym Soap Charting.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Acronym Soap Charting Nurses spend a lot of time. It is the documentation used to record information about encounters with. Any palliating or provoking factors. The onset of the patient’s symptoms. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. To standardize your reporting across notes,. Acronym Soap Charting.
From aliciawatts.z13.web.core.windows.net
Soap Chart Note Is An Acronym For Acronym Soap Charting The onset of the patient’s symptoms. In this article, the soap or soapie method will be described. Soap nursing notes are a type of patient progress note or nurse’s note. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation. Acronym Soap Charting.
From practicebetter.io
Mastering SOAP Notes as a Wellness Professional Practice Better Acronym Soap Charting Nurses spend a lot of time. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap nursing notes are a type of patient progress note or nurse’s note. In this article, the soap or soapie method will be described. Soap is an acronym for the 4 sections, or headings, that each progress note. Acronym Soap Charting.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Acronym Soap Charting Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with. Where a client’s subjective experiences, feelings, or perspectives are recorded. To standardize your reporting across notes, include information using the. Acronym Soap Charting.
From www.studypool.com
SOLUTION Soapie medical abbreviations Studypool Acronym Soap Charting It is the documentation used to record information about encounters with. The onset of the patient’s symptoms. Soap is an acronym for the 4 sections, or headings, that each progress note contains: In this article, the soap or soapie method will be described. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where. Acronym Soap Charting.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 Acronym Soap Charting Nurses spend a lot of time. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap nursing notes are a type of patient progress note or nurse’s note. In this article, the soap or soapie method will be described. Any palliating or provoking factors. The onset of the patient’s symptoms. To standardize your reporting. Acronym Soap Charting.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by Acronym Soap Charting It is the documentation used to record information about encounters with. To standardize your reporting across notes, include information using the acronym opqrst: Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Nurses spend a lot of time. In this article, the soap. Acronym Soap Charting.
From www.advantismed.com
How to Master Nurse Charting & Avoid Mistakes Acronym Soap Charting The onset of the patient’s symptoms. Soap is an acronym for the 4 sections, or headings, that each progress note contains: In this article, the soap or soapie method will be described. To standardize your reporting across notes, include information using the acronym opqrst: Nurses spend a lot of time. Soap notes are a way for healthcare providers to document. Acronym Soap Charting.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Acronym Soap Charting Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with. To standardize your reporting across notes, include information using the acronym opqrst: The onset of the patient’s symptoms. Any palliating or provoking factors. Soap is an acronym for the 4 sections, or headings,. Acronym Soap Charting.
From www.pinterest.com
How to Make Soap Notes Soap note, Physical therapy, Massage therapy Acronym Soap Charting Any palliating or provoking factors. Where a client’s subjective experiences, feelings, or perspectives are recorded. It is the documentation used to record information about encounters with. In this article, the soap or soapie method will be described. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a way for healthcare providers. Acronym Soap Charting.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Acronym Soap Charting To standardize your reporting across notes, include information using the acronym opqrst: Any palliating or provoking factors. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Nurses spend a lot of time. Where a client’s subjective experiences, feelings,. Acronym Soap Charting.
From in.pinterest.com
First Aid CPD SOAP 👀⠀ ⠀ SOAP is a medical acronym used to remember Acronym Soap Charting To standardize your reporting across notes, include information using the acronym opqrst: In this article, the soap or soapie method will be described. Where a client’s subjective experiences, feelings, or perspectives are recorded. Nurses spend a lot of time. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap nursing notes are a. Acronym Soap Charting.
From www.pinterest.ca
This picture is an example of a mnemonic strategy. This particular Acronym Soap Charting Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with. Nurses spend a lot of time. The onset of the patient’s symptoms. In this article, the soap or soapie method will be described. Soap notes are a way for healthcare providers to document patient data more. Acronym Soap Charting.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] Acronym Soap Charting It is the documentation used to record information about encounters with. Any palliating or provoking factors. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or perspectives are recorded. Nurses spend a lot of time. Soap is an acronym for the 4 sections, or headings, that each. Acronym Soap Charting.
From www.pinterest.jp
Beginner’s Guide to Writing a SOAP Note (with SOAP note template) My Acronym Soap Charting Soap is an acronym for the 4 sections, or headings, that each progress note contains: Nurses spend a lot of time. The onset of the patient’s symptoms. Any palliating or provoking factors. To standardize your reporting across notes, include information using the acronym opqrst: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.. Acronym Soap Charting.
From mavink.com
Occupational Therapy Soap Notes Examples Acronym Soap Charting Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The onset of the patient’s symptoms. Nurses spend a lot of time. In this article, the soap or soapie method will be described. Soap is an acronym for the 4 sections, or headings, that each progress note contains: To standardize your reporting across notes,. Acronym Soap Charting.
From es.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract Acronym Soap Charting The onset of the patient’s symptoms. It is the documentation used to record information about encounters with. Nurses spend a lot of time. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap is an acronym for the 4 sections, or headings, that. Acronym Soap Charting.
From npchartingschool.com
Examples of a SOAP note plus 7 tips for charting! Acronym Soap Charting In this article, the soap or soapie method will be described. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The onset of the patient’s symptoms. Soap nursing notes are a type of patient progress note or nurse’s note. Any palliating or provoking factors. It is the documentation used to record information about. Acronym Soap Charting.
From www.pinterest.com
Occupational Therapy Documentation Tips The OT Toolbox Occupational Acronym Soap Charting Where a client’s subjective experiences, feelings, or perspectives are recorded. In this article, the soap or soapie method will be described. It is the documentation used to record information about encounters with. Any palliating or provoking factors. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Nurses spend a lot of time. Soap nursing. Acronym Soap Charting.
From www.pinterest.com
SOAP Note Speech therapy tools, Speech language activities, Speech Acronym Soap Charting To standardize your reporting across notes, include information using the acronym opqrst: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or perspectives are recorded. The onset of the patient’s symptoms. Soap nursing notes are a type of patient progress note or nurse’s note. Any palliating or. Acronym Soap Charting.
From www.eslprintables.com
English worksheets SOAPS Acronym Acronym Soap Charting Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with. Where a client’s subjective experiences, feelings, or perspectives are recorded. To standardize your reporting across notes, include information using the acronym opqrst: In this article, the soap or soapie method will be described.. Acronym Soap Charting.
From eloisewilkinson.z21.web.core.windows.net
Soap Note Abbreviations List Acronym Soap Charting The onset of the patient’s symptoms. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Where a client’s subjective experiences, feelings, or perspectives are recorded. To standardize your reporting across notes, include information using the acronym opqrst: Nurses. Acronym Soap Charting.
From www.pinterest.com.au
The Subjective, Objective, Assessment and Plan (SOAP) note is an Acronym Soap Charting Nurses spend a lot of time. Any palliating or provoking factors. In this article, the soap or soapie method will be described. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters. Acronym Soap Charting.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Acronym Soap Charting Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: In this article, the soap or soapie method will be described. Soap nursing notes are a type of patient progress note or nurse’s note. Nurses spend a lot of time. Any palliating or provoking factors.. Acronym Soap Charting.
From www.tosurg.ca
Notes and Templates TOsurg Acronym Soap Charting Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. To standardize your reporting across notes, include information using the acronym opqrst: Where a client’s subjective experiences, feelings, or perspectives are recorded. The onset of the patient’s symptoms. Nurses spend a lot of time. Soap nursing notes are a type of patient progress note. Acronym Soap Charting.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Acronym Soap Charting It is the documentation used to record information about encounters with. Soap nursing notes are a type of patient progress note or nurse’s note. In this article, the soap or soapie method will be described. The onset of the patient’s symptoms. Where a client’s subjective experiences, feelings, or perspectives are recorded. Nurses spend a lot of time. Soap notes are. Acronym Soap Charting.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For Acronym Soap Charting In this article, the soap or soapie method will be described. To standardize your reporting across notes, include information using the acronym opqrst: Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains: Soap notes are a way for healthcare providers to document patient data. Acronym Soap Charting.
From www.rxnt.com
What exactly are SOAP notes? For Medical Practices RXNT Acronym Soap Charting It is the documentation used to record information about encounters with. Any palliating or provoking factors. In this article, the soap or soapie method will be described. To standardize your reporting across notes, include information using the acronym opqrst: The onset of the patient’s symptoms. Soap is an acronym for the 4 sections, or headings, that each progress note contains:. Acronym Soap Charting.
From eloisewilkinson.z21.web.core.windows.net
Soap Chart Note Is An Acronym For Acronym Soap Charting Any palliating or provoking factors. Soap nursing notes are a type of patient progress note or nurse’s note. Nurses spend a lot of time. In this article, the soap or soapie method will be described. Where a client’s subjective experiences, feelings, or perspectives are recorded. Soap is an acronym for the 4 sections, or headings, that each progress note contains:. Acronym Soap Charting.