Soap Notes Ros . approximately 154 views in the last month. Adult full exam (just copy and paste) general. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Open an existing soapnote or create a new soapnote. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. Create a soapnote for help. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Denies changes in vision and. Denies weight loss, fever and chills.
from www.studocu.com
the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. approximately 154 views in the last month. Denies changes in vision and. Adult full exam (just copy and paste) general. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Open an existing soapnote or create a new soapnote. Denies weight loss, fever and chills. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical.
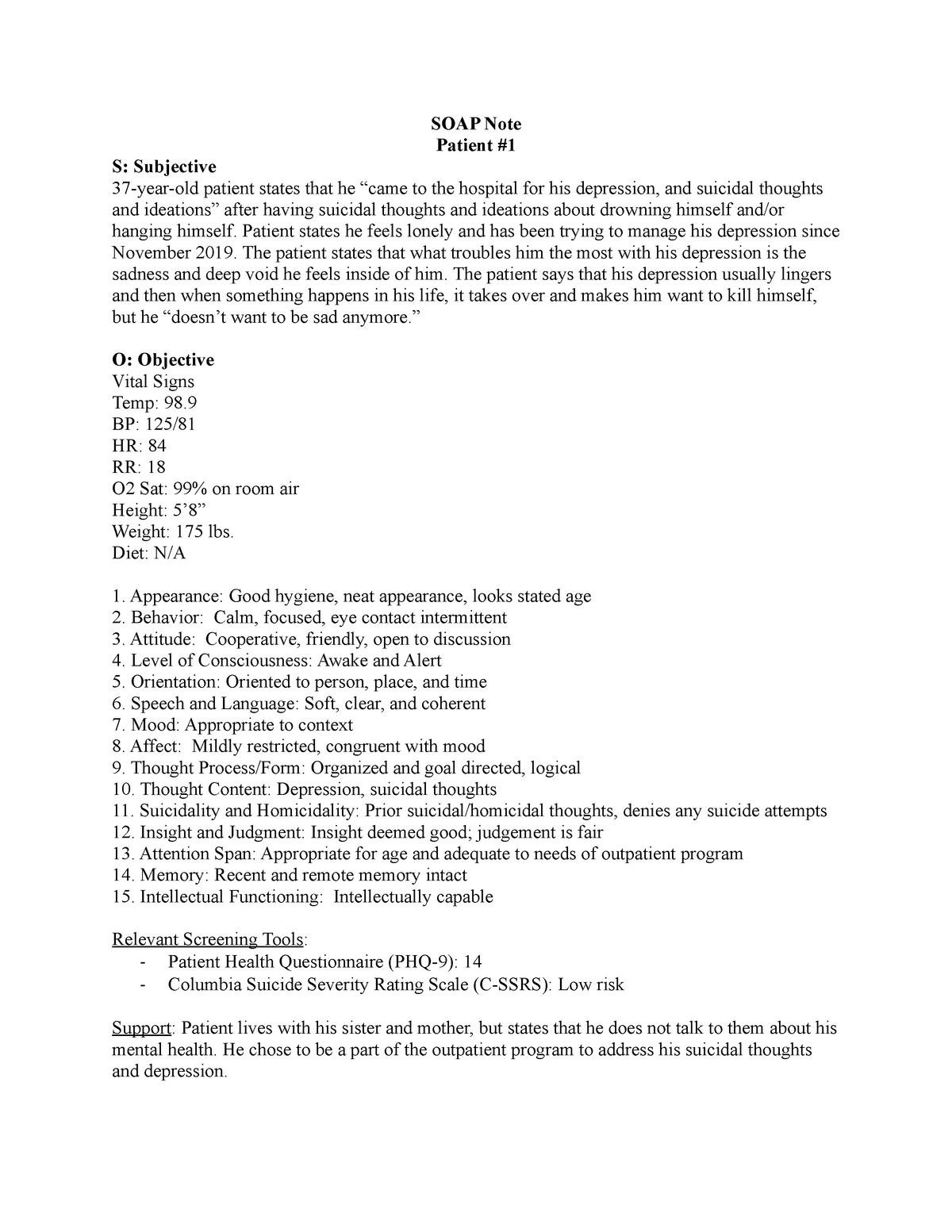
SOAP Note SOAP Notes for Psych SOAP Note Patient S Subjective 37
Soap Notes Ros the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Adult full exam (just copy and paste) general. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Denies changes in vision and. approximately 154 views in the last month. Create a soapnote for help. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies weight loss, fever and chills. Open an existing soapnote or create a new soapnote. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical.
From www.studocu.com
SOAP Note 2 Graded.docx Sample SOAP Note 2 Graded NURS 6210 July 12 Soap Notes Ros in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Open an existing soapnote or create a new soapnote. soap notes are a systematic method of documenting patient encounters, capturing. Soap Notes Ros.
From www.studocu.com
SOAP Note Abdominal Pain EP Identifying Information Focused Soap Notes Ros in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. approximately 154 views in the last month. Adult full exam (just copy and paste) general. . Soap Notes Ros.
From www.pinterest.com
Image result for SOAP note examples Soap note, Dr orders, Internal Soap Notes Ros Adult full exam (just copy and paste) general. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies weight loss, fever and chills. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. soap notes are a systematic method of documenting patient. Soap Notes Ros.
From www.printabletemplateslab.com
10+ Soap Note Template Free Download Word, Excel, PDF Format!! Soap Notes Ros Open an existing soapnote or create a new soapnote. Denies changes in vision and. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Create a soapnote for help. Adult full exam (just copy and paste) general.. Soap Notes Ros.
From moussyusa.com
46+ Free Download SOAP Note Template for Your Medical Note Mous Syusa Soap Notes Ros review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. approximately 154 views in the last month. Open an. Soap Notes Ros.
From idtcenter.org
Editable Soap Note Ashpmedia Diabetic Soap Note Template IDTcenter Soap Notes Ros in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. Adult full exam (just copy and paste) general. approximately 154 views in the last month. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Denies weight loss,. Soap Notes Ros.
From www.studocu.com
SOAP Note SOAP Notes for Psych SOAP Note Patient S Subjective 37 Soap Notes Ros review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. approximately 154 views in the last month. in addition to the problem at hand, soap notes generally address important past medical history,. Soap Notes Ros.
From writeness-training.blogspot.com
Nurse Practitioner Example Of Soap Note Soap Notes Ros Denies changes in vision and. Adult full exam (just copy and paste) general. Create a soapnote for help. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. approximately 154 views in the last. Soap Notes Ros.
From giofysjkx.blob.core.windows.net
Charting Soap Examples at Betty Gutierrez blog Soap Notes Ros in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. approximately 154 views in the last month. Create a soapnote for help. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Denies weight loss, fever and chills. Open an. Soap Notes Ros.
From www.studocu.com
Heent soap example Soap note © 2019 Walden University Page 1 of 2 Soap Notes Ros Adult full exam (just copy and paste) general. Denies changes in vision and. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Denies weight loss, fever and chills. Open an existing soapnote or create a. Soap Notes Ros.
From www.etsy.com
SOAP Note Template for Nps/pas/mds // NP Students // NP School Help Etsy Soap Notes Ros approximately 154 views in the last month. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. . Soap Notes Ros.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Diet & Nutrition Soap Notes Ros soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Denies changes in vision and. Denies weight loss, fever and chills. Create a soapnote for help. Adult full exam (just copy and paste) general. Open an existing soapnote or create a new soapnote. review of systems, ros, normal template transcription examples for reference. Soap Notes Ros.
From www.detrester.com
Soap Notes Counseling Template Soap Notes Ros Create a soapnote for help. Adult full exam (just copy and paste) general. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. soap notes are a systematic method of documenting patient encounters, capturing essential information, and. Soap Notes Ros.
From www.studypool.com
SOLUTION Nsg 6420 Soap Note Studypool Soap Notes Ros review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health.. Soap Notes Ros.
From www.studocu.com
GYN PAP SOAP Note soap SCR 110 Studocu Soap Notes Ros in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Create a soapnote for help. review of systems or ros medical report template example format for reference by. Soap Notes Ros.
From www.studocu.com
Health Assessment Skin Condition SOAP NOTE Differential Diagnosis for Soap Notes Ros review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies changes in vision and. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history,. Soap Notes Ros.
From studylib.net
SOAP NOTE S The patient is a 70 year old female complaining of Soap Notes Ros Open an existing soapnote or create a new soapnote. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Adult full exam (just copy and paste) general. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Denies weight loss, fever and chills. review of. Soap Notes Ros.
From www.pinterest.fr
soap note examples for nurse practitioners Nursing Documentation Soap Notes Ros Open an existing soapnote or create a new soapnote. Create a soapnote for help. Denies weight loss, fever and chills. approximately 154 views in the last month. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. soap notes are a systematic method of. Soap Notes Ros.
From www.studocu.com
Soapnote Sample With complete review of systems SOAP Note Focused Soap Notes Ros Denies changes in vision and. approximately 154 views in the last month. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Adult full exam (just copy and paste) general. Create a soapnote for help. . Soap Notes Ros.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Ros Denies weight loss, fever and chills. Denies changes in vision and. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. review of systems, ros, normal template transcription examples for. Soap Notes Ros.
From www.studocu.com
Episodic SOAP Note Template Rx1 EPISODIC SOAP Note Template Student Soap Notes Ros Denies changes in vision and. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Open an existing soapnote or create a new soapnote. Create a soapnote for help. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. Denies. Soap Notes Ros.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners, Physician Soap Notes Ros soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Open an existing soapnote or create a new soapnote. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social. Soap Notes Ros.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Ros the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Create a soapnote for help. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Adult full exam (just copy and paste) general. approximately 154 views in the last month. review of systems or ros medical. Soap Notes Ros.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Ros review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Adult full exam (just copy and paste) general. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Denies changes in vision and. in addition to the problem at hand, soap notes generally address important past medical. Soap Notes Ros.
From www.carepatron.com
SOAP Notes for Dental Template & Example Free PDF Download Soap Notes Ros Adult full exam (just copy and paste) general. Open an existing soapnote or create a new soapnote. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. approximately 154 views in the last. Soap Notes Ros.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Notes Ros review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so.. Soap Notes Ros.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Notes Ros the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies changes in vision and. approximately 154 views in the last month. Adult full exam (just copy and paste) general. in addition to the. Soap Notes Ros.
From www.etsy.com
SOAP Note FNP School 28 Yo Well Woman With Ros/obj./assessment & Plan W Soap Notes Ros approximately 154 views in the last month. Adult full exam (just copy and paste) general. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies changes in vision and. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Create a soapnote for help.. Soap Notes Ros.
From www.youtube.com
5 Tips in 10 Minutes SOAP Notes YouTube Soap Notes Ros Adult full exam (just copy and paste) general. Denies changes in vision and. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. soap notes are a systematic method of. Soap Notes Ros.
From www.studocu.com
Heent SOAP Note Practicum Episodic/Focus Note Template Patient Soap Notes Ros review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Adult full exam (just copy and paste) general. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies changes in vision and. Create a soapnote for help. the subjective, objective, assessment and. Soap Notes Ros.
From studylib.net
SOAP Note Instructions Soap Notes Ros Denies weight loss, fever and chills. Open an existing soapnote or create a new soapnote. Adult full exam (just copy and paste) general. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. Denies changes in vision and. approximately 154 views in the last month. review of systems, ros,. Soap Notes Ros.
From studylib.net
pediatric soap note Soap Notes Ros approximately 154 views in the last month. Adult full exam (just copy and paste) general. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Create a soapnote for help. review of systems,. Soap Notes Ros.
From mavink.com
Ejemplos De Notas Soap Soap Notes Ros Denies changes in vision and. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Create a soapnote for help. in addition to the problem at hand, soap notes generally address important past medical history, relevant family history, social history, albeit briefly so. Adult full exam (just copy and paste) general. Open an. Soap Notes Ros.
From hellorache.com
How to Handle Medical Documentation? Hello Rache Soap Notes Ros soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Denies changes in vision and. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Create a soapnote for help. review of systems, ros, normal template transcription examples for reference by allied health professionals and medical. Open an. Soap Notes Ros.
From templatearchive.com
30 Blank SOAP Note Templates (+Examples) TemplateArchive Soap Notes Ros Create a soapnote for help. Denies weight loss, fever and chills. soap notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating. Open an existing soapnote or create a new soapnote. Denies changes in vision and. review of systems or ros medical report template example format for reference by medical transcriptionists and allied health.. Soap Notes Ros.