What Is The Soap Method In Medical Terms . Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. In the soap format, soap stands for subjective, objective, assessment, and plan.
from nursing-professor.com
In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Each letter refers to one of four sections in the document. Exactly what is a soap note?. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of.
SOAP Note for Stroke Nursing Professor
What Is The Soap Method In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan.
From medfitnetwork.org
Using the SOAP Note Format for Medical Fitness Clients What Is The Soap Method In Medical Terms Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers. What Is The Soap Method In Medical Terms.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For What Is The Soap Method In Medical Terms The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in. What Is The Soap Method In Medical Terms.
From positivepsychology.com
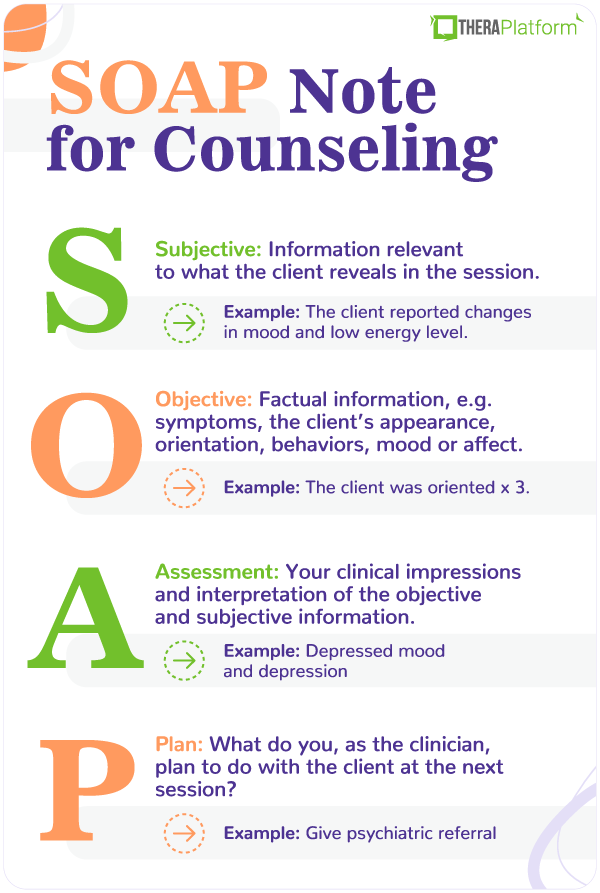
What are SOAP Notes in Counseling? (+ Examples) What Is The Soap Method In Medical Terms Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT Patient Medical Records PowerPoint Presentation, free download What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in. What Is The Soap Method In Medical Terms.
From www.pinterest.com
First Aid CPD SOAP 👀⠀ ⠀ SOAP is a medical acronym used to remember What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap—or subjective, objective, assessment and plan—notes allow clinicians to. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT How is Soap Made? PowerPoint Presentation, free download ID2530430 What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. What Is The Soap Method In Medical Terms.
From www.process.st
SOAP Note Template Process Street What Is The Soap Method In Medical Terms Each letter refers to one of four sections in the document. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in. What Is The Soap Method In Medical Terms.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary What Is The Soap Method In Medical Terms Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.. What Is The Soap Method In Medical Terms.
From nursing-professor.com
SOAP Note for Stroke Nursing Professor What Is The Soap Method In Medical Terms Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.. What Is The Soap Method In Medical Terms.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Each letter refers to one of four sections in the document. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment,. What Is The Soap Method In Medical Terms.
From www.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract What Is The Soap Method In Medical Terms Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT PATIENT MEDICAL RECORDS PowerPoint Presentation, free download What Is The Soap Method In Medical Terms Exactly what is a soap note?. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an. What Is The Soap Method In Medical Terms.
From www.pinterest.com
SOAP vs SBAR Nursing school tips, Nursing school survival, Nursing What Is The Soap Method In Medical Terms Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment,. What Is The Soap Method In Medical Terms.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. Exactly what is a soap note?. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. In the soap format, soap stands for subjective, objective, assessment, and plan.. What Is The Soap Method In Medical Terms.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide What Is The Soap Method In Medical Terms Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 What Is The Soap Method In Medical Terms Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Each letter refers to one of four sections in the document. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In. What Is The Soap Method In Medical Terms.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Is The Soap Method In Medical Terms Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a way for healthcare providers to document patient. What Is The Soap Method In Medical Terms.
From www.capterra.com
Free SOAP Notes Templates for Busy Healthcare Professionals Capterra What Is The Soap Method In Medical Terms Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Exactly. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT Medical Records and Documentation PowerPoint Presentation, free What Is The Soap Method In Medical Terms Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document.. What Is The Soap Method In Medical Terms.
From covenantlifecog.com
SOAPmethodposter What Is The Soap Method In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Exactly what is a soap note?. Each letter refers to one of four sections in the document. Soap notes are a standardized method of documenting patient encounters in medical and healthcare. What Is The Soap Method In Medical Terms.
From topanswerideas.com
The Importance of Soap Notes in Well Woman Exams A Comprehensive Guide What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. In the soap format,. What Is The Soap Method In Medical Terms.
From www.pinterest.com
Soap Note Template Pendidikan, Penyakit, Rumah sakit What Is The Soap Method In Medical Terms Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Each letter refers to one of four sections in the document. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment, and. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT Communication of the Nursing Process Documentation PowerPoint What Is The Soap Method In Medical Terms The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Exactly what is a soap note?. Soap notes are a way for healthcare providers to document. What Is The Soap Method In Medical Terms.
From www.theraplatform.com
Occupational therapy SOAP note What Is The Soap Method In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. What Is The Soap Method In Medical Terms.
From hellorache.com
How to Handle Medical Documentation? Hello Rache What Is The Soap Method In Medical Terms Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing. What Is The Soap Method In Medical Terms.
From musculoskeletalkey.com
Treatment Notes and Progress Notes Using a Modified SOAP Format What Is The Soap Method In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap—or subjective, objective, assessment and. What Is The Soap Method In Medical Terms.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox What Is The Soap Method In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. Each letter refers to one of four sections in the document. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. What Is The Soap Method In Medical Terms.
From www.slideshare.net
Nursing Skills Charting What Is The Soap Method In Medical Terms The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Exactly what is a soap note?. Each letter refers to. What Is The Soap Method In Medical Terms.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education What Is The Soap Method In Medical Terms Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a way. What Is The Soap Method In Medical Terms.
From www.studocu.com
Med Info SOAPnote Jobaid \cluster1\home\nancy\1 Training\EMR\SOAP What Is The Soap Method In Medical Terms Each letter refers to one of four sections in the document. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient. What Is The Soap Method In Medical Terms.
From viewpoint.online
How to put the patient first in your eye examinations Viewpoint What Is The Soap Method In Medical Terms In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. What Is The Soap Method In Medical Terms.
From www.pinterest.com
soap notes with the words soap on it What Is The Soap Method In Medical Terms Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Each letter refers to one of four sections in the document. Soap notes are. What Is The Soap Method In Medical Terms.
From studylib.net
Patient SOAP Note Charting Procedures What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings.. What Is The Soap Method In Medical Terms.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is The Soap Method In Medical Terms Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing. What Is The Soap Method In Medical Terms.
From www.slideserve.com
PPT Lesson 1.8 The SOAP Note PowerPoint Presentation, free download What Is The Soap Method In Medical Terms Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. Each letter refers to one of. What Is The Soap Method In Medical Terms.