Utilization Review Insurance . The skillset gained popularity within. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. The purpose of the review is to confirm. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. insurance companies and payers: a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. utilization review is a health insurance company's opportunity to review a request for medical treatment. The review confirms that the insurance company will provide appropriate financial coverage for medical services. utilization review (ur) is the process of reviewing an episode of care.
from templates.rjuuc.edu.np
utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The skillset gained popularity within. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. insurance companies and payers: The review confirms that the insurance company will provide appropriate financial coverage for medical services. utilization review (ur) is the process of reviewing an episode of care. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. The purpose of the review is to confirm. utilization review is a health insurance company's opportunity to review a request for medical treatment.
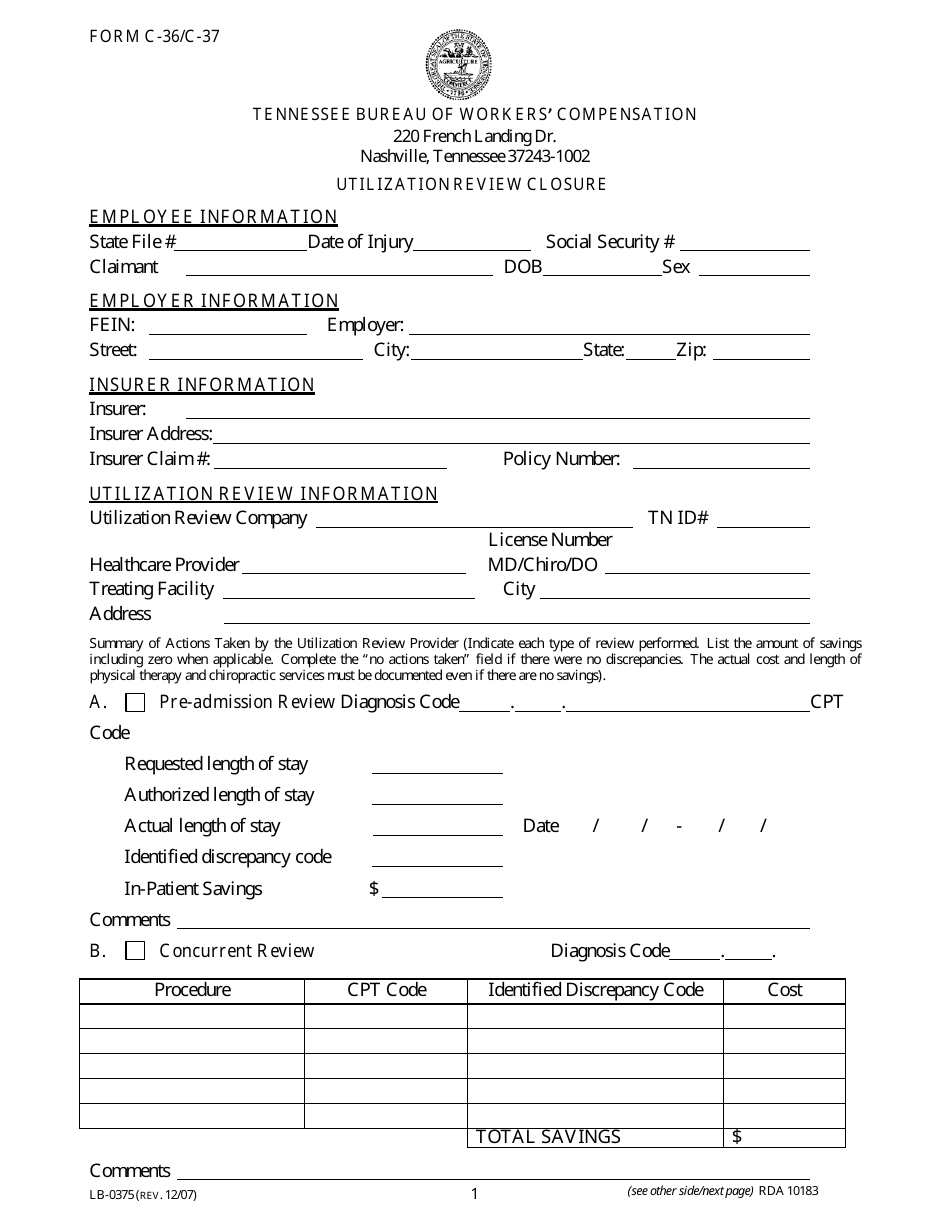
Utilization Review Template
Utilization Review Insurance The purpose of the review is to confirm. utilization review is a health insurance company's opportunity to review a request for medical treatment. The purpose of the review is to confirm. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The skillset gained popularity within. insurance companies and payers: The review confirms that the insurance company will provide appropriate financial coverage for medical services. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. utilization review (ur) is the process of reviewing an episode of care.
From zealie.com
Utilization Review in 2021 What You Should Know Zealie Utilization Review Insurance utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The purpose of the review is to confirm. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. a utilization review is a process in. Utilization Review Insurance.
From www.avabilling.com
Utilization Review AVA Billing & Consulting Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. The skillset gained popularity within. utilization review (ur) is the process of reviewing an episode of care. utilization review is a health insurance company's opportunity to review a request for medical treatment. a utilization review is a process in which. Utilization Review Insurance.
From injurymanagement.com
Utilization Review Injury Management Organization Utilization Review Insurance The skillset gained popularity within. utilization review (ur) is the process of reviewing an episode of care. The review confirms that the insurance company will provide appropriate financial coverage for medical services. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services.. Utilization Review Insurance.
From www.michiganautolaw.com
Utilization Review For Nurses, Doctors and Hospitals Michigan Auto Law Utilization Review Insurance insurance companies and payers: The review confirms that the insurance company will provide appropriate financial coverage for medical services. The purpose of the review is to confirm. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization reviews, also known as utilization management, is used by insurance companies and healthcare. Utilization Review Insurance.
From www.financestrategists.com
Insurance Policy Reviews Definition, Benefits, and Key Tips Utilization Review Insurance insurance companies and payers: utilization review is a health insurance company's opportunity to review a request for medical treatment. The skillset gained popularity within. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review (ur) is the process. Utilization Review Insurance.
From www.verywellhealth.com
How Utilization Review Works Utilization Review Insurance The purpose of the review is to confirm. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review is a health insurance company's opportunity to review a request for medical treatment. insurance companies and payers: the utilization review. Utilization Review Insurance.
From argodata.com
Behavioral Health Utilization Review Utilization Review Insurance The skillset gained popularity within. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review (ur) is the process of reviewing an episode of care. The review confirms that the insurance company will provide appropriate financial coverage for medical services.. Utilization Review Insurance.
From chartexamples.com
Utilization Review Process Flowchart Chart Examples Utilization Review Insurance a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. utilization review (ur) is the process of reviewing an episode of care. insurance companies and payers: utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments. Utilization Review Insurance.
From www.ziprecruiter.com
3359/hr Insurance Utilization Review Jobs (NOW HIRING) Utilization Review Insurance The purpose of the review is to confirm. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review is a health insurance company's. Utilization Review Insurance.
From autonofaultlaw.com
Utilization Review Process Auto No Fault Law Utilization Review Insurance The review confirms that the insurance company will provide appropriate financial coverage for medical services. The skillset gained popularity within. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. insurance companies and payers: a utilization review is a process in. Utilization Review Insurance.
From www.mcg.com
The Utilization Review Process and the Origins of Medical Necessity Utilization Review Insurance The skillset gained popularity within. utilization review (ur) is the process of reviewing an episode of care. utilization review is a health insurance company's opportunity to review a request for medical treatment. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. the utilization review function was initially performed by. Utilization Review Insurance.
From bhmpc.com
Art of Utilization Review Balancing Care and Resources BHM Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. insurance companies and payers: The review confirms that the insurance company will provide appropriate financial coverage for medical services. The skillset gained popularity within. The purpose of the review is to confirm. utilization review (ur) is the process of reviewing an. Utilization Review Insurance.
From www.revwerxbilling.com
Importance of Utilization Review in Healthcare Healthcare UR Utilization Review Insurance utilization review is a health insurance company's opportunity to review a request for medical treatment. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The review confirms that the insurance company will provide appropriate financial coverage for medical services. The purpose. Utilization Review Insurance.
From donegalgroup-blog.com
How to Review Your Insurance Policies Donegal Insurance Group Blog Utilization Review Insurance The purpose of the review is to confirm. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. utilization review is a health insurance company's opportunity to review a request for medical treatment. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the. Utilization Review Insurance.
From zealie.com
Utilization Review in 2021 What You Should Know Zealie Utilization Review Insurance a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. The review confirms that the insurance company will provide appropriate financial coverage for medical services. utilization review is a health insurance company's opportunity to review a request for medical treatment. The purpose of the review is to confirm. The skillset gained popularity. Utilization Review Insurance.
From www.amalgamatedbenefits.com
Utilization Reviews Uncover New Revenue Opportunities AMCM Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. insurance companies and payers: utilization review (ur) is the process of reviewing an episode of care. The purpose of the review is to confirm. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for.. Utilization Review Insurance.
From www.researchgate.net
(PDF) A Guide for the Utilization of Health Insurance Review and Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization review (ur) is the process of reviewing an episode of care. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. The skillset gained popularity within. utilization reviews, also known as utilization management,. Utilization Review Insurance.
From slideplayer.com
Utilization Review and Executive Health Resources ppt download Utilization Review Insurance utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review is a health insurance company's opportunity to review a request for medical treatment. insurance companies and payers: The purpose of the review is to confirm. The review confirms that. Utilization Review Insurance.
From www.templateroller.com
Form FIS2358 Download Fillable PDF or Fill Online Auto Insurance Utilization Review Insurance The purpose of the review is to confirm. utilization review (ur) is the process of reviewing an episode of care. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The review confirms that the insurance company will provide appropriate financial coverage. Utilization Review Insurance.
From www.youtube.com
Utilization Review (UR) / Insurance Case Management Resume and Utilization Review Insurance utilization review is a health insurance company's opportunity to review a request for medical treatment. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The review confirms that the insurance company will provide appropriate financial coverage for medical services. The purpose. Utilization Review Insurance.
From www.templateroller.com
Kansas Application for Utilization Review Certificate Fill Out, Sign Utilization Review Insurance a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. insurance companies and payers: utilization review (ur) is the process of reviewing an episode of care. The skillset gained popularity within. The purpose of. Utilization Review Insurance.
From www.youtube.com
Remote Nursing Jobs Utilization Review (UR) Insurance YouTube Utilization Review Insurance a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. The skillset gained popularity within. utilization review is a health insurance company's opportunity to review a request for medical treatment. utilization review (ur) is the process of reviewing an episode of care. the utilization review function was initially performed by. Utilization Review Insurance.
From www.slideshare.net
Utilization Management Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization review (ur) is the process of reviewing an episode of care. The review confirms that the insurance company will provide appropriate financial coverage for medical services. a utilization review is a process in which a patient's care plan undergoes evaluation,. Utilization Review Insurance.
From www.sunlitcovehealthcare.com
Benefits Of Partnering In Utilization Review Sunlit Cove Healthcare Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization review (ur) is the process of reviewing an episode of care. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. insurance companies and payers: utilization review is a health insurance company's. Utilization Review Insurance.
From sevafirm.com
Utilization Review Seva Law Firm Utilization Review Insurance The purpose of the review is to confirm. The review confirms that the insurance company will provide appropriate financial coverage for medical services. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization review (ur) is the process of reviewing an episode of care. insurance companies and payers: a. Utilization Review Insurance.
From www.youtube.com
A guide for the utilization of Health Insurance Review and Assessment Utilization Review Insurance utilization review is a health insurance company's opportunity to review a request for medical treatment. The purpose of the review is to confirm. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review (ur) is the process of reviewing. Utilization Review Insurance.
From vdocuments.mx
UTILIZATION REVIEW CHECKLIST in REVIEW CHECKLIST . Fill in "Located Utilization Review Insurance utilization review (ur) is the process of reviewing an episode of care. The purpose of the review is to confirm. The review confirms that the insurance company will provide appropriate financial coverage for medical services. utilization review is a health insurance company's opportunity to review a request for medical treatment. utilization reviews, also known as utilization management,. Utilization Review Insurance.
From luvfasr239.weebly.com
Insurance Utilization Report luvfasr Utilization Review Insurance The purpose of the review is to confirm. utilization review is a health insurance company's opportunity to review a request for medical treatment. utilization review (ur) is the process of reviewing an episode of care. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. The skillset gained popularity within. . Utilization Review Insurance.
From templates.rjuuc.edu.np
Utilization Review Template Utilization Review Insurance The review confirms that the insurance company will provide appropriate financial coverage for medical services. utilization review (ur) is the process of reviewing an episode of care. utilization review is a health insurance company's opportunity to review a request for medical treatment. The skillset gained popularity within. a utilization review is a process in which a patient's. Utilization Review Insurance.
From bhmpc.com
Understanding Utilization Review Utilization Review Insurance utilization review (ur) is the process of reviewing an episode of care. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. utilization review is a health insurance company's opportunity to review a request for medical treatment. The purpose of the review is to confirm. The review confirms that the insurance. Utilization Review Insurance.
From info.argodata.com
Improving Utilization Review Workflow Efficiency Utilization Review Insurance The purpose of the review is to confirm. The review confirms that the insurance company will provide appropriate financial coverage for medical services. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. utilization review (ur) is the process of reviewing an episode of care. the utilization review function was initially. Utilization Review Insurance.
From bhmpc.com
Utilization Review vs Utilization Management BHM Healthcare Utilization Review Insurance the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. The review confirms that the insurance company will provide appropriate financial coverage for medical services. The. Utilization Review Insurance.
From medium.com
What Is Utilization Review. Utilization review is the process that Utilization Review Insurance The purpose of the review is to confirm. The skillset gained popularity within. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization reviews, also known as utilization management, is used by insurance companies and healthcare providers to evaluate the necessity and appropriateness of medical treatments and services. utilization review. Utilization Review Insurance.
From www.pdffiller.com
Fillable Online Insurance Carrier/Utilization Review Fax Email Print Utilization Review Insurance The review confirms that the insurance company will provide appropriate financial coverage for medical services. a utilization review is a process in which a patient's care plan undergoes evaluation, typically for. The purpose of the review is to confirm. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. insurance companies. Utilization Review Insurance.
From thenonclinicalpt.com
Utilization Review Careers How to Get Started The NonClinical PT Utilization Review Insurance The review confirms that the insurance company will provide appropriate financial coverage for medical services. The skillset gained popularity within. The purpose of the review is to confirm. the utilization review function was initially performed by registered nurses (rns) in the acute hospital setting. utilization reviews, also known as utilization management, is used by insurance companies and healthcare. Utilization Review Insurance.