Cvs Caremark Prior Authorization Form For Tremfya . Reminders and tips when completing prior authorizations for your patients. A live representative will assist. When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. If you have questions regarding the prior authorization,.
from eforms.com
When a pa is needed for a prescription, the member will be asked to have. Reminders and tips when completing prior authorizations for your patients. If you have questions regarding the prior authorization,. A live representative will assist. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya.
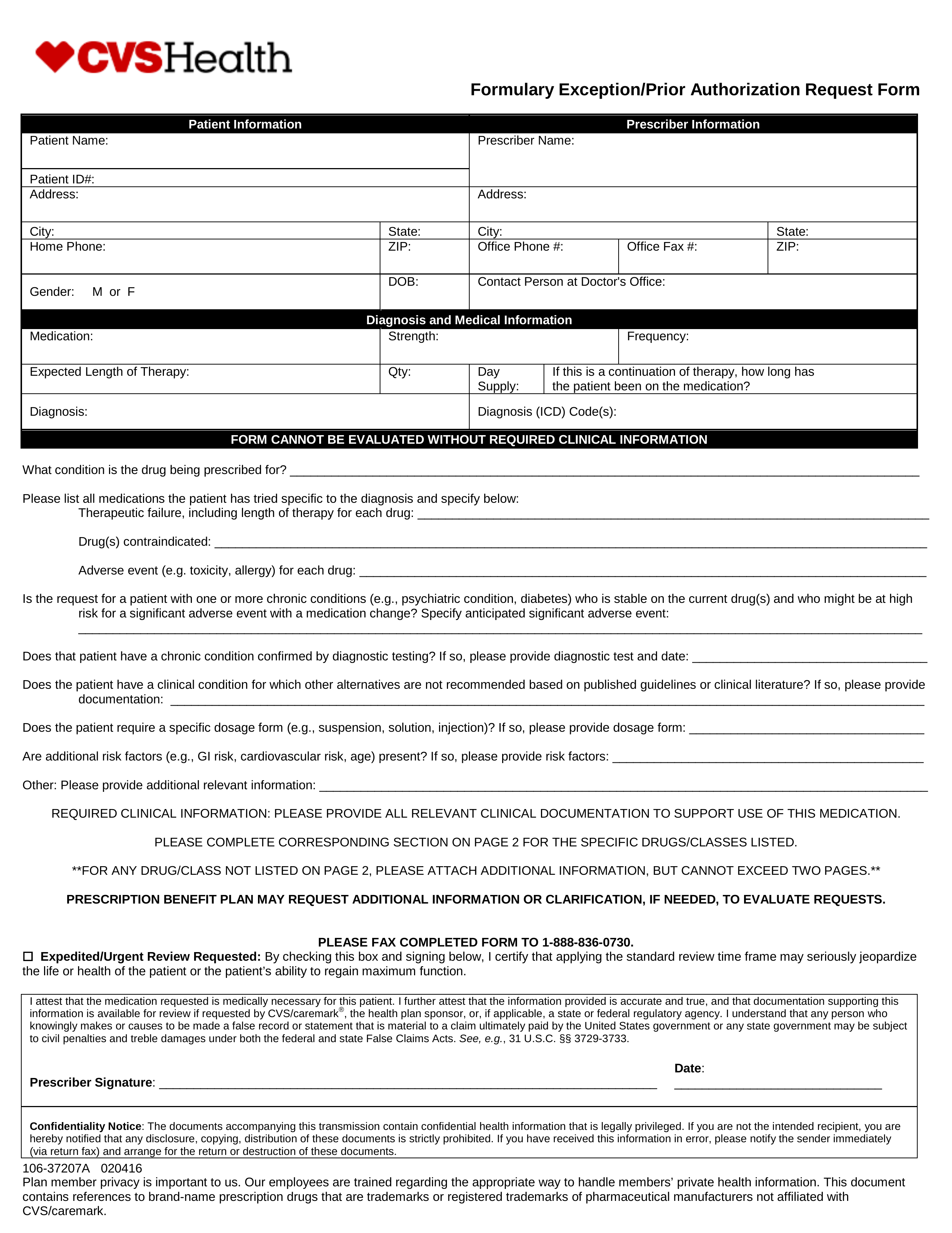
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
Cvs Caremark Prior Authorization Form For Tremfya This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Reminders and tips when completing prior authorizations for your patients. If you have questions regarding the prior authorization,. When a pa is needed for a prescription, the member will be asked to have. A live representative will assist. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form Cvs Caremark Prior Authorization Form For Tremfya A live representative will assist. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Reminders and tips when completing prior authorizations for your patients. If you have questions regarding the prior authorization,. When a pa is needed for a prescription, the member will be asked to have. Authorization of 12 months. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Tremfya Prior Authorization Request Form Fax Email Cvs Caremark Prior Authorization Form For Tremfya If you have questions regarding the prior authorization,. A live representative will assist. When a pa is needed for a prescription, the member will be asked to have. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Authorization of 12 months may be granted for adult. Cvs Caremark Prior Authorization Form For Tremfya.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Tremfya Reminders and tips when completing prior authorizations for your patients. If you have questions regarding the prior authorization,. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. When a pa is needed for a prescription, the member will be asked to have. A live representative will. Cvs Caremark Prior Authorization Form For Tremfya.
From mungfali.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable E10 Cvs Caremark Prior Authorization Form For Tremfya Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A live representative will assist. If you have questions regarding the prior authorization,. When a pa is needed for a prescription, the member will be asked to have. A completed patient authorization form, found on pages 3 and 4. Cvs Caremark Prior Authorization Form For Tremfya.
From www.uslegalforms.com
Caremark Prior Authorization Request Form Fill and Sign Printable Cvs Caremark Prior Authorization Form For Tremfya Reminders and tips when completing prior authorizations for your patients. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. When a pa is needed for a prescription, the member will be asked to have. If you have questions regarding the prior authorization,. Authorization of 12 months may be granted for adult. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization HMSA Fax Email Print Cvs Caremark Prior Authorization Form For Tremfya Reminders and tips when completing prior authorizations for your patients. A live representative will assist. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. When a pa is needed for a prescription, the member will be asked to have. If you have questions regarding the prior authorization,. A. Cvs Caremark Prior Authorization Form For Tremfya.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Tremfya Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support. Cvs Caremark Prior Authorization Form For Tremfya.
From www.dochub.com
Cvs caremark wegovy prior authorization criteria Fill out & sign Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. A live representative will assist. If you have questions regarding the prior authorization,. Reminders and tips when completing prior authorizations for your patients. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under. Cvs Caremark Prior Authorization Form For Tremfya.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. Reminders and tips when completing prior authorizations for your patients. A live representative will assist. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This patient’s benefit plan requires prior authorization for certain. Cvs Caremark Prior Authorization Form For Tremfya.
From www.templateroller.com
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online Cvs Caremark Prior Authorization Form For Tremfya If you have questions regarding the prior authorization,. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A live representative will assist. When a pa is needed for a prescription, the member will be asked to have. A completed patient authorization form, found on pages 3 and 4. Cvs Caremark Prior Authorization Form For Tremfya.
From www.formsbank.com
Caremark Prior Authorization Criteria Request Form printable pdf download Cvs Caremark Prior Authorization Form For Tremfya Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. If you have questions regarding the prior authorization,. Reminders and tips when completing prior authorizations for your patients. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support. Cvs Caremark Prior Authorization Form For Tremfya.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. Reminders and tips when completing prior authorizations for your patients. A completed patient authorization form, found on pages 3 and 4 of this document,. Cvs Caremark Prior Authorization Form For Tremfya.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Prior Authorization Form For Tremfya A live representative will assist. When a pa is needed for a prescription, the member will be asked to have. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Reminders and tips when completing prior authorizations for your patients. If you have questions regarding the prior. Cvs Caremark Prior Authorization Form For Tremfya.
From www.authorizationform.net
Cvs Caremark Ivig Prior Authorization Form Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. When a pa is needed for a prescription, the member will be asked to have. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Cvs Caremark Formulary Exception Prior Authorization Request Form Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. If you have questions regarding the prior authorization,. A live representative will assist. Reminders and tips when completing prior authorizations for your patients. This patient’s benefit plan requires prior authorization for certain medications in order for the. Cvs Caremark Prior Authorization Form For Tremfya.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. Reminders and tips when completing prior. Cvs Caremark Prior Authorization Form For Tremfya.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Tremfya Reminders and tips when completing prior authorizations for your patients. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A completed patient authorization form, found on pages 3 and 4. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A live representative will assist. Reminders and tips when completing prior authorizations for your patients. If. Cvs Caremark Prior Authorization Form For Tremfya.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Reminders and tips when completing prior authorizations for your patients. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A live representative will assist. Authorization of 12 months. Cvs Caremark Prior Authorization Form For Tremfya.
From eforms.com
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. When a pa is needed for a prescription, the member will be asked to have. Reminders and tips when completing prior authorizations for your patients. Authorization of 12 months may be granted for adult members who have. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. Reminders and tips when completing prior authorizations for your patients. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Authorization Form For Tremfya This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you have questions regarding the prior authorization,. A live representative will assist. Reminders and tips when completing prior authorizations for your patients. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Fill Online Cvs Caremark Prior Authorization Form For Tremfya This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you have questions regarding the prior authorization,. When a pa is needed for a prescription, the member will be asked to have. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic. Cvs Caremark Prior Authorization Form For Tremfya.
From www.authorizationform.net
Caremark Prior Authorization Form Printable Pdf Download Cvs Caremark Prior Authorization Form For Tremfya A live representative will assist. If you have questions regarding the prior authorization,. Reminders and tips when completing prior authorizations for your patients. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. When a pa is needed for a prescription, the member will be asked to have. This. Cvs Caremark Prior Authorization Form For Tremfya.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A completed patient authorization form, found. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. If you have questions regarding the prior authorization,. A live representative will assist. Reminders and tips when completing prior authorizations for your patients. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Authorization of 12 months. Cvs Caremark Prior Authorization Form For Tremfya.
From www.authorizationform.net
Caremark Specialty Pharmacy Prior Authorization Form Cvs Caremark Prior Authorization Form For Tremfya If you have questions regarding the prior authorization,. When a pa is needed for a prescription, the member will be asked to have. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Authorization of 12 months may be granted for adult members who have previously received. Cvs Caremark Prior Authorization Form For Tremfya.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you have questions regarding the prior authorization,. A live representative will assist. Authorization of 12 months may be granted for adult members who have previously received. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form eForms Fax Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A live representative will assist. Reminders and tips when completing prior authorizations for your patients. If. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online For purposes of this authorization form, CVS Caremark Cvs Caremark Prior Authorization Form For Tremfya A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. If you have questions regarding the prior authorization,. Reminders and tips when completing prior authorizations for your patients. When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan. Cvs Caremark Prior Authorization Form For Tremfya.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Authorization Form For Tremfya Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Reminders and tips when completing prior authorizations for your patients. A live representative will assist. When a pa is needed for. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print Cvs Caremark Prior Authorization Form For Tremfya Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. Reminders and tips when completing prior authorizations for your patients. When a pa is needed for. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Provider Resource Cvs Caremark Prior Authorization Form For Tremfya If you have questions regarding the prior authorization,. A live representative will assist. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Reminders and tips when completing prior authorizations for your patients. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain. Cvs Caremark Prior Authorization Form For Tremfya.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Form Fax Email Print Cvs Caremark Prior Authorization Form For Tremfya When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A live representative will assist. A. Cvs Caremark Prior Authorization Form For Tremfya.
From www.dochub.com
Caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form For Tremfya Authorization of 12 months may be granted for adult members who have previously received a biologic or targeted synthetic drug (e.g.,. A completed patient authorization form, found on pages 3 and 4 of this document, is necessary to access certain patient support under tremfya. When a pa is needed for a prescription, the member will be asked to have. This. Cvs Caremark Prior Authorization Form For Tremfya.