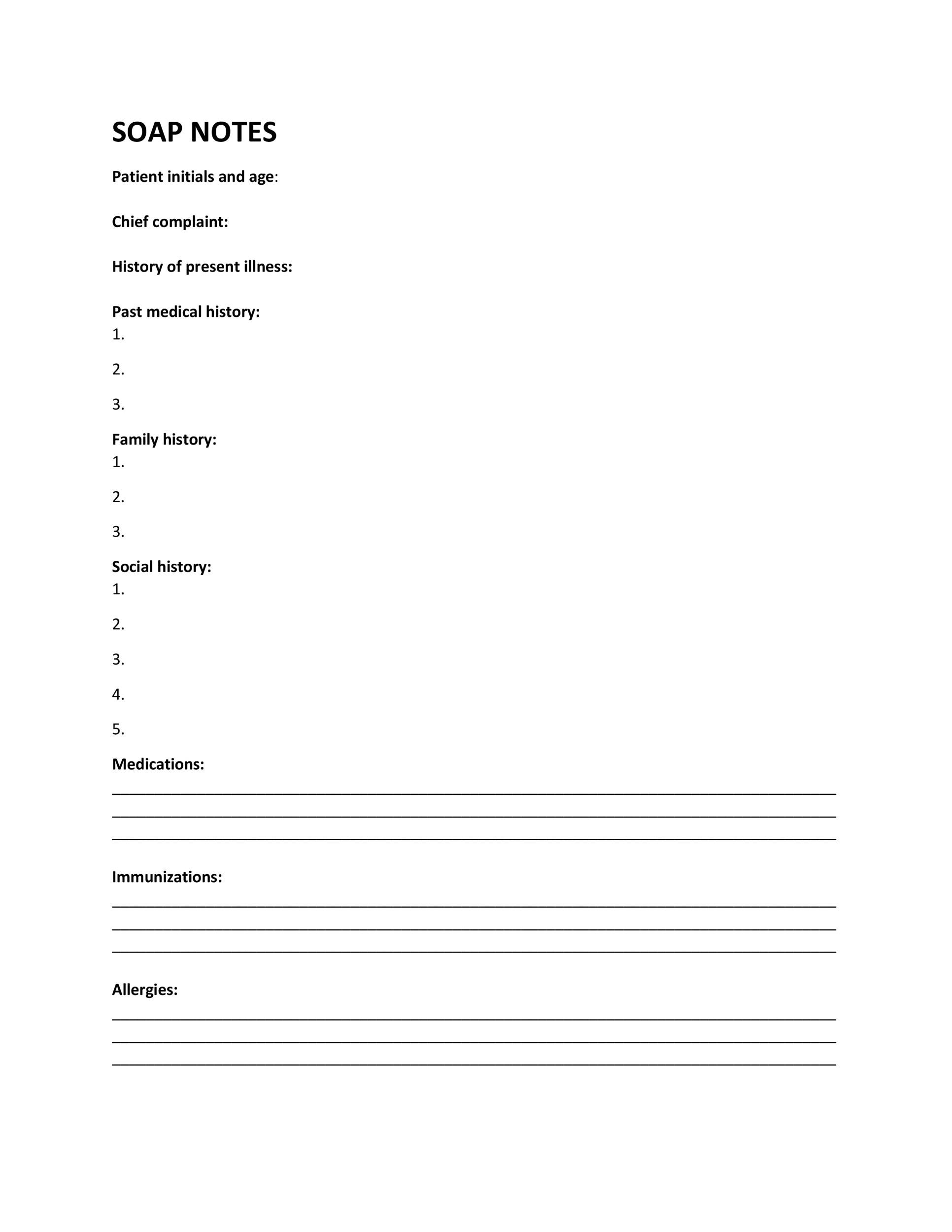
Soap Form Example . We’ve also compiled some soap. Our website have dozens soap note examples, templates & samples! It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes template is a form of measure of progression. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. Soap notes are written documentation made during the course of treatment of a patient.
from templatelab.com
Soap notes template is a form of measure of progression. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Our website have dozens soap note examples, templates & samples! Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap nursing notes are a type of patient progress note or nurse’s note. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. They contain four primary sections, represented by its acronym: Soap notes are written documentation made during the course of treatment of a patient. It is the documentation used to record information about encounters with patients that follows a specific format. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of.
40 Fantastic SOAP Note Examples & Templates Template Lab
Soap Form Example However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. Our website have dozens soap note examples, templates & samples! The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: We’ve also compiled some soap. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap nursing notes are a type of patient progress note or nurse’s note. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap notes are written documentation made during the course of treatment of a patient. Soap notes template is a form of measure of progression. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Form Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap nursing notes are a type of patient progress note or nurse’s note. We’ve also compiled some soap. Soap notes are a specific. Soap Form Example.
From www.printablee.com
Counseling Soap Note Templates 10 Free PDF Printables Printablee Soap Form Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. We’ve also compiled some soap. Soap nursing notes are a type of patient progress note or nurse’s note. It. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are written documentation made during the course of treatment of a patient. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes template is a form of measure of progression. In this article, we’ll cover how to write. Soap Form Example.
From www.printabletemplateslab.com
10+ Soap Note Template Free Download Word, Excel, PDF Format!! Soap Form Example Soap notes are written documentation made during the course of treatment of a patient. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. Our website have dozens soap note examples, templates & samples! Soap notes are a specific format for writing progress notes as a behavioral health clinician. We’ve. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Form Example It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap notes template is a form of measure of progression. The subjective, objective, assessment. Soap Form Example.
From dl-uk.apowersoft.com
Printable Dental Soap Note Template Soap Form Example Our website have dozens soap note examples, templates & samples! It is the documentation used to record information about encounters with patients that follows a specific format. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Form Example Soap notes template is a form of measure of progression. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. We’ve. Soap Form Example.
From www.sampletemplates.com
FREE 8+ Sample Soap Note Templates in MS Word PDF Soap Form Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. It is the documentation used to record information about encounters with patients that follows a specific format. Our website have dozens soap note examples, templates & samples! In this article, we’ll cover how to write soap notes, describing the soap format and what. Soap Form Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Form Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Our website have dozens soap note examples, templates & samples! They contain four primary sections, represented by its acronym: However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. Soap notes are a. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example It is the documentation used to record information about encounters with patients that follows a specific format. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes are a specific format for writing progress notes as a behavioral health clinician. However, not all sections are needed for every note, so healthcare. Soap Form Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Form Example It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes template is a form of measure of progression. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The subjective, objective, assessment and plan (soap) note is an acronym representing. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. We’ve also compiled some soap. Soap notes are a specific format for writing progress notes as a behavioral health clinician. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their.. Soap Form Example.
From www.capterra.com
Free SOAP Notes Templates for Busy Healthcare Professionals Capterra Soap Form Example It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: Soap notes are written documentation made during the course of treatment of a patient. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data.. Soap Form Example.
From www.sampletemplates.com
SOAP Note Example 12 + Free Samples , Examples , Format Soap Form Example However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented. Soap Form Example.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Form Example It is the documentation used to record information about encounters with patients that follows a specific format. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Our website have dozens soap note examples, templates & samples! Soap notes template is a form of measure of progression. They contain four primary sections, represented. Soap Form Example.
From www.template.net
11+ Soap Note Templates Free Sample, Example, Format Download! Soap Form Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. Soap notes are written documentation made during the course of treatment of a patient. They contain four primary sections, represented by its acronym: Soap nursing. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example Soap notes are written documentation made during the course of treatment of a patient. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. Our website have dozens soap note examples, templates & samples! We’ve also compiled some soap. Soap nursing notes are a type of patient progress note or. Soap Form Example.
From www.studocu.com
Comprehensive SOAP Template Comprehensive SOAP Template Patient Soap Form Example We’ve also compiled some soap. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. It is the. Soap Form Example.
From www.theraplatform.com
Occupational therapy SOAP note Soap Form Example It is the documentation used to record information about encounters with patients that follows a specific format. Soap nursing notes are a type of patient progress note or nurse’s note. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes template is a form of measure of progression. Soap notes are. Soap Form Example.
From kelitbanganwonogiri.org
Soap Assessment Template Soap Form Example Soap notes template is a form of measure of progression. Soap nursing notes are a type of patient progress note or nurse’s note. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. It is the documentation used to record information about encounters with patients that follows a specific format.. Soap Form Example.
From www.pinterest.com
Soap Notes for Massage Therapists Doctors note template, Soap note Soap Form Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. They contain four primary sections, represented by its acronym: However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. In this article, we’ll cover how to write soap notes, describing the soap format. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Form Example Our website have dozens soap note examples, templates & samples! Soap notes template is a form of measure of progression. We’ve also compiled some soap. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. They contain four primary sections, represented by its acronym: It is the documentation used to record information about. Soap Form Example.
From sarseh.com
Soap Report Template Soap Form Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Our website. Soap Form Example.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Soap Form Example However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. It is the documentation used to record information about encounters with patients that follows. Soap Form Example.
From www.carepatron.com
SOAP Progress Notes Template & Example Free PDF Download Soap Form Example Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes template is a form of measure of progression. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan. Soap Form Example.
From www.formsbank.com
17 Soap Note Templates free to download in PDF Soap Form Example We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Form Example Our website have dozens soap note examples, templates & samples! In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: It is the documentation used to record information about encounters with patients that follows a specific format. However, not all. Soap Form Example.
From www.printabletemplateslab.com
10+ Soap Note Template Free Download Word, Excel, PDF Format!! Soap Form Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes template is a form. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Form Example The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Our website have dozens soap note examples, templates & samples! However, not all sections are needed for every note,. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap notes template is a form of measure of progression. In this article, we’ll cover how. Soap Form Example.
From www.carecloud.com
Free SOAP Notes Template CareCloud Continuum Soap Form Example We’ve also compiled some soap. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Our website have dozens soap note examples, templates & samples! They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap notes template is a form of measure of progression. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their. It is the documentation. Soap Form Example.
From www.massagebook.com
Free Massage SOAP Notes Forms MassageBook Soap Form Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. It is the documentation used to record. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Form Example They contain four primary sections, represented by its acronym: In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap (subjective, objective, assessment, plan) notes provide a comprehensive overview of the client’s condition, including both subjective and objective data. Soap notes template is a form of measure of progression.. Soap Form Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Form Example We’ve also compiled some soap. Soap notes are written documentation made during the course of treatment of a patient. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: However, not all sections are needed for every note, so healthcare. Soap Form Example.