Where Do Labs Go In Soap Note . Vital signs including oxygen saturation when indicated. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. september 10, 2015 | evidence in integrative healthcare. In the outpatient clinic, soap is the traditional note structure: In a previous post, we reviewed the necessity of basic best practices for. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. S ubjective, o bjective, a ssessment, p lan. soap notes are a specific format for writing progress notes as a behavioral health clinician.
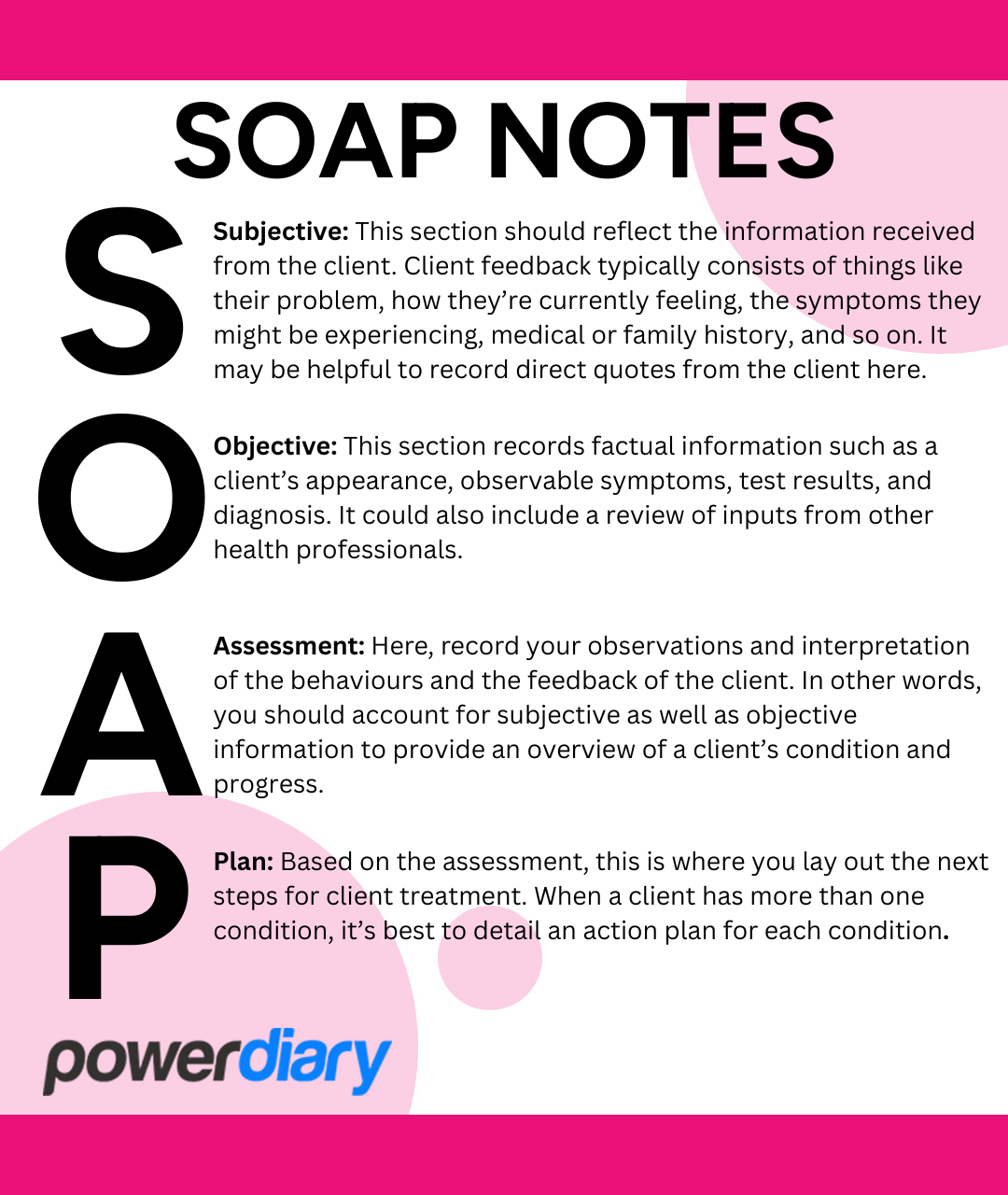
from www.powerdiary.com
In the outpatient clinic, soap is the traditional note structure: S ubjective, o bjective, a ssessment, p lan. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Vital signs including oxygen saturation when indicated. In a previous post, we reviewed the necessity of basic best practices for. september 10, 2015 | evidence in integrative healthcare. soap notes are a specific format for writing progress notes as a behavioral health clinician.
What’s the Difference SOAP Notes vs DAP Notes Power Diary
Where Do Labs Go In Soap Note In a previous post, we reviewed the necessity of basic best practices for. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. In the outpatient clinic, soap is the traditional note structure: soap notes are a specific format for writing progress notes as a behavioral health clinician. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Vital signs including oxygen saturation when indicated. In a previous post, we reviewed the necessity of basic best practices for. september 10, 2015 | evidence in integrative healthcare. S ubjective, o bjective, a ssessment, p lan.
From www.studocu.com
SOAP Note Hypothyroid Treatment of Hypothyroidism Discussion Prompt Where Do Labs Go In Soap Note In a previous post, we reviewed the necessity of basic best practices for. september 10, 2015 | evidence in integrative healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Vital signs including oxygen saturation when indicated. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of. Where Do Labs Go In Soap Note.
From www.etsy.com
Lab Values Cheat Sheet Nursing Notes NCLEX Review Mark Etsy México Where Do Labs Go In Soap Note In the outpatient clinic, soap is the traditional note structure: Vital signs including oxygen saturation when indicated. soap notes are a specific format for writing progress notes as a behavioral health clinician. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. S ubjective, o bjective, a ssessment, p. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Where Do Labs Go In Soap Note learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. In a previous post, we reviewed the necessity of basic best practices for. Vital signs including oxygen saturation when indicated. the soap note (an acronym for. Where Do Labs Go In Soap Note.
From www.etsy.com
SOAP Notes Etsy Where Do Labs Go In Soap Note september 10, 2015 | evidence in integrative healthcare. In the outpatient clinic, soap is the traditional note structure: the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Vital signs including oxygen saturation when indicated. soap notes are a specific format for writing progress notes as a behavioral. Where Do Labs Go In Soap Note.
From www.powerdiary.com
What’s the Difference SOAP Notes vs DAP Notes Power Diary Where Do Labs Go In Soap Note soap notes are a specific format for writing progress notes as a behavioral health clinician. september 10, 2015 | evidence in integrative healthcare. In the outpatient clinic, soap is the traditional note structure: S ubjective, o bjective, a ssessment, p lan. In a previous post, we reviewed the necessity of basic best practices for. learn how to. Where Do Labs Go In Soap Note.
From www.capterra.com
Free SOAP Notes Templates for Busy Healthcare Professionals Capterra Where Do Labs Go In Soap Note Vital signs including oxygen saturation when indicated. In a previous post, we reviewed the necessity of basic best practices for. september 10, 2015 | evidence in integrative healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. learn how to write a soap note so you can efficiently track, assess, diagnose, and. Where Do Labs Go In Soap Note.
From www.realiaproject.org
11+ SOAP Note Example FREE Download [Word, PDF] Where Do Labs Go In Soap Note soap notes are a specific format for writing progress notes as a behavioral health clinician. Vital signs including oxygen saturation when indicated. september 10, 2015 | evidence in integrative healthcare. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. In the outpatient clinic, soap is the traditional. Where Do Labs Go In Soap Note.
From www.allbusinesstemplates.com
免费 Chiropractic Soap Note 样本文件在 Where Do Labs Go In Soap Note september 10, 2015 | evidence in integrative healthcare. Vital signs including oxygen saturation when indicated. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a specific. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Where Do Labs Go In Soap Note soap notes are a specific format for writing progress notes as a behavioral health clinician. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Vital signs including oxygen saturation when. Where Do Labs Go In Soap Note.
From www.studypool.com
SOLUTION Pmhnp Soap Note Studypool Where Do Labs Go In Soap Note In a previous post, we reviewed the necessity of basic best practices for. Vital signs including oxygen saturation when indicated. In the outpatient clinic, soap is the traditional note structure: september 10, 2015 | evidence in integrative healthcare. S ubjective, o bjective, a ssessment, p lan. soap notes are a specific format for writing progress notes as a. Where Do Labs Go In Soap Note.
From www.vrogue.co
How To Write A Soap Note With Soap Note Examples vrogue.co Where Do Labs Go In Soap Note the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. soap notes are a specific format for writing progress notes as a behavioral health clinician. In a previous post, we reviewed the necessity of basic best practices for. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of. Where Do Labs Go In Soap Note.
From creativedesignlayouttemplates.blogspot.com
Soap Report Template Where Do Labs Go In Soap Note S ubjective, o bjective, a ssessment, p lan. soap notes are a specific format for writing progress notes as a behavioral health clinician. In the outpatient clinic, soap is the traditional note structure: In a previous post, we reviewed the necessity of basic best practices for. Vital signs including oxygen saturation when indicated. learn how to write a. Where Do Labs Go In Soap Note.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox Where Do Labs Go In Soap Note In the outpatient clinic, soap is the traditional note structure: the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. learn how to write a soap note so you can efficiently track, assess, diagnose,. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Where Do Labs Go In Soap Note the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Vital signs including oxygen saturation when indicated. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. september 10, 2015 | evidence in integrative healthcare. S ubjective, o bjective, a ssessment, p lan. In the outpatient. Where Do Labs Go In Soap Note.
From tutore.org
Pain Management Soap Note Template Master of Documents Where Do Labs Go In Soap Note the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. september 10, 2015 | evidence in integrative healthcare. soap notes are a specific format for writing progress notes as a behavioral health clinician. learn how to write a soap note so you can efficiently track, assess, diagnose,. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Where Do Labs Go In Soap Note soap notes are a specific format for writing progress notes as a behavioral health clinician. Vital signs including oxygen saturation when indicated. september 10, 2015 | evidence in integrative healthcare. S ubjective, o bjective, a ssessment, p lan. In a previous post, we reviewed the necessity of basic best practices for. learn how to write a soap. Where Do Labs Go In Soap Note.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Where Do Labs Go In Soap Note learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Vital signs including oxygen saturation when indicated. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely.. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Where Do Labs Go In Soap Note learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. In the outpatient clinic, soap is the traditional note structure: soap notes are a specific format for writing progress notes as a behavioral health clinician. In a previous post, we reviewed the necessity of basic best practices for. the subjective,. Where Do Labs Go In Soap Note.
From www.pinterest.com
soap note template counseling Google Search SOAP Notes Pinterest Where Do Labs Go In Soap Note the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. In the outpatient clinic, soap is the traditional note structure: Vital signs including oxygen saturation when indicated. soap notes are a specific format for writing progress notes as a behavioral health clinician. learn how to write a soap. Where Do Labs Go In Soap Note.
From idtcenter.org
Editable Soap Note Ashpmedia Diabetic Soap Note Template IDTcenter Where Do Labs Go In Soap Note S ubjective, o bjective, a ssessment, p lan. september 10, 2015 | evidence in integrative healthcare. soap notes are a specific format for writing progress notes as a behavioral health clinician. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Vital signs including oxygen saturation when indicated. In a previous post, we. Where Do Labs Go In Soap Note.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Diet & Nutrition Where Do Labs Go In Soap Note Vital signs including oxygen saturation when indicated. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a specific format for writing progress notes as a behavioral health clinician. september 10, 2015 | evidence in integrative healthcare. the subjective, objective, assessment and plan (soap) note is. Where Do Labs Go In Soap Note.
From medicalform-111.blogspot.com
19 MEDICAL NOTES R/O MedicalForm Where Do Labs Go In Soap Note the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. In the outpatient clinic, soap is the traditional note structure: S ubjective, o bjective, a ssessment, p lan. soap notes are a specific format for writing progress notes as a behavioral health clinician. In a previous post, we reviewed the necessity of basic best. Where Do Labs Go In Soap Note.
From www.wordtemplatesonline.net
How to Write a SOAP Note (with SOAP Note Examples) Where Do Labs Go In Soap Note S ubjective, o bjective, a ssessment, p lan. soap notes are a specific format for writing progress notes as a behavioral health clinician. september 10, 2015 | evidence in integrative healthcare. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. In a previous post, we reviewed the. Where Do Labs Go In Soap Note.
From lessonmediaryouko99.z19.web.core.windows.net
soap notes worksheet Where Do Labs Go In Soap Note the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. september 10, 2015 | evidence in integrative healthcare. In a previous post, we reviewed the necessity of basic best practices for. Vital signs including oxygen saturation when indicated. soap notes are a specific format for writing progress notes. Where Do Labs Go In Soap Note.
From pinterest.com
SOAP Note Example for Mental Health Counselors Mental Health Where Do Labs Go In Soap Note learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. In a previous post, we reviewed the necessity of basic best practices for. In the outpatient clinic, soap is the traditional note structure: september 10, 2015 | evidence in integrative healthcare. the subjective, objective, assessment and plan (soap) note is. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Where Do Labs Go In Soap Note learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a specific format for writing progress notes as a behavioral health clinician. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. september 10, 2015 | evidence in integrative healthcare. S ubjective,. Where Do Labs Go In Soap Note.
From studylib.net
PROGRESS (SOAP) NOTES Where Do Labs Go In Soap Note september 10, 2015 | evidence in integrative healthcare. S ubjective, o bjective, a ssessment, p lan. In the outpatient clinic, soap is the traditional note structure: the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Vital signs including oxygen saturation when indicated. learn how to write a soap note so you can. Where Do Labs Go In Soap Note.
From studylib.net
Patient SOAP Note Charting Procedures Where Do Labs Go In Soap Note S ubjective, o bjective, a ssessment, p lan. soap notes are a specific format for writing progress notes as a behavioral health clinician. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. In the outpatient clinic, soap is the traditional note structure: september 10, 2015 | evidence in integrative healthcare. learn. Where Do Labs Go In Soap Note.
From www.pinterest.com
SOAP Notes Occupational Therapy Examination Review Guide 3rd Edition Where Do Labs Go In Soap Note S ubjective, o bjective, a ssessment, p lan. september 10, 2015 | evidence in integrative healthcare. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. Vital signs including oxygen saturation when indicated. In. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Where Do Labs Go In Soap Note Vital signs including oxygen saturation when indicated. soap notes are a specific format for writing progress notes as a behavioral health clinician. In a previous post, we reviewed the necessity of basic best practices for. In the outpatient clinic, soap is the traditional note structure: september 10, 2015 | evidence in integrative healthcare. learn how to write. Where Do Labs Go In Soap Note.
From www.pinterest.com
875 best images about nursing stuff on Pinterest Pharmacology Where Do Labs Go In Soap Note september 10, 2015 | evidence in integrative healthcare. In the outpatient clinic, soap is the traditional note structure: the subjective, objective, assessment and plan (soap) note is an acronym representing a widely. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. S ubjective, o bjective, a ssessment,. Where Do Labs Go In Soap Note.
From www.theraplatform.com
Occupational therapy SOAP note Where Do Labs Go In Soap Note september 10, 2015 | evidence in integrative healthcare. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Vital signs including oxygen saturation when indicated. the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. soap notes are a specific. Where Do Labs Go In Soap Note.
From xfessayhgxr.berlinunlimited.org
Soap note Coursework Example Where Do Labs Go In Soap Note soap notes are a specific format for writing progress notes as a behavioral health clinician. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. september 10, 2015 | evidence in integrative healthcare. Vital signs including oxygen saturation when indicated. In a previous post, we reviewed the necessity of basic. Where Do Labs Go In Soap Note.
From www.pinterest.com
Soap notes OT Pinterest Soaps, Note and Soap note Where Do Labs Go In Soap Note In the outpatient clinic, soap is the traditional note structure: S ubjective, o bjective, a ssessment, p lan. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Vital signs including oxygen saturation when indicated. In a previous post, we reviewed the necessity of basic best practices for. soap notes are. Where Do Labs Go In Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Where Do Labs Go In Soap Note the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. In the outpatient clinic, soap is the traditional note structure: Vital signs including oxygen saturation when indicated. september 10, 2015 | evidence in integrative healthcare. S ubjective, o bjective, a ssessment, p lan. In a previous post, we reviewed. Where Do Labs Go In Soap Note.