Olive Health Prior Authorization . Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. With olive’s technology, florida blue becomes the first u.s. Florida blue receives hundreds of thousands of prior authorization submissions each year. With olive’s technology, florida blue becomes the first u.s. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Deploying an ai platform from a company called olive shifts. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process.
from authorizationforms.com
With olive’s technology, florida blue becomes the first u.s. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Deploying an ai platform from a company called olive shifts. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Florida blue receives hundreds of thousands of prior authorization submissions each year. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions.
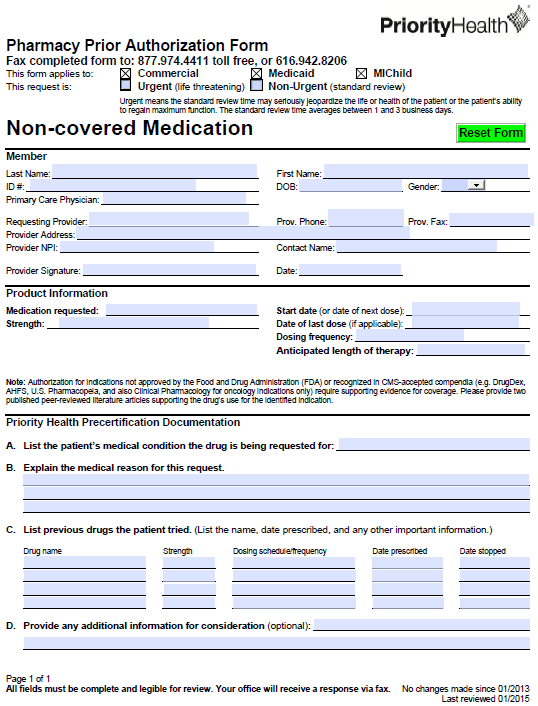
Free PriorityHealth Prior Prescription (Rx) Authorization Form PDF
Olive Health Prior Authorization Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. With olive’s technology, florida blue becomes the first u.s. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Deploying an ai platform from a company called olive shifts. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Florida blue receives hundreds of thousands of prior authorization submissions each year. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s.
From behavehealth.com
Doing a PreCertification or Prior Authorization with Molina HealthCare Olive Health Prior Authorization Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Deploying an ai platform from a company called olive shifts. With olive’s technology, florida blue becomes the first u.s. With olive’s technology, florida. Olive Health Prior Authorization.
From hitconsultant.net
M&A M&A Olive Acquires AI Prior Authorization Company Verata Health Olive Health Prior Authorization Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve. Olive Health Prior Authorization.
From studylib.net
PriorAuthFilled Olive Health Prior Authorization Deploying an ai platform from a company called olive shifts. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Guidewell’s subsidiary, florida blue, will become the first. Olive Health Prior Authorization.
From authorizationforms.com
Free PriorityHealth Prior Prescription (Rx) Authorization Form PDF Olive Health Prior Authorization Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Florida blue receives hundreds of thousands of prior authorization submissions each year. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Guidewell’s subsidiary, florida blue, will become the first us payer. Olive Health Prior Authorization.
From www.phoenixvirtualstaff.com
The Complete Guide to Prior Authorization Navigating the Complex Olive Health Prior Authorization Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. Guidewell’s health plan companies receive hundreds of thousands of prior authorization. Olive Health Prior Authorization.
From www.authorizationform.net
Lucent Health Prior Authorization Form Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to. Olive Health Prior Authorization.
From www.uslegalforms.com
Optima Medicaid Prior Authorization Form Outline Of Medicare Fill and Olive Health Prior Authorization Florida blue receives hundreds of thousands of prior authorization submissions each year. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Guidewell’s subsidiary, florida blue, will become the first us payer. Olive Health Prior Authorization.
From specialty-health.blogspot.com
Specialty Health What Is Prior Authorization For Medication Olive Health Prior Authorization Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the. Olive Health Prior Authorization.
From www.sampletemplates.com
FREE 7+ Medicaid Prior Authorization Forms in PDF Olive Health Prior Authorization To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Deploying an ai platform from a company called olive shifts. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. With olive’s technology, florida. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 41+ Authorization Forms in PDF Excel MS word Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Deploying an ai platform from a company called olive shifts. Florida blue receives hundreds of thousands of prior authorization submissions each year. With olive’s technology, florida blue becomes the first u.s. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of. Olive Health Prior Authorization.
From mavink.com
Prior Authorization Process Flow Chart Olive Health Prior Authorization Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. With olive’s technology, florida blue becomes the first u.s. With olive’s technology,. Olive Health Prior Authorization.
From blog.nalashaahealth.com
Why Health Plans Should Automate PreAuthorization? Olive Health Prior Authorization Deploying an ai platform from a company called olive shifts. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue,. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 8+ Sample Prior Authorization Forms in PDF MS Word Olive Health Prior Authorization Florida blue receives hundreds of thousands of prior authorization submissions each year. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. Deploying an ai platform from a company called olive shifts. With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a. Olive Health Prior Authorization.
From www.slideserve.com
PPT A Detailed Guide On Prior Authorization Process In RCM PowerPoint Olive Health Prior Authorization Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. With olive’s technology, florida blue becomes the first u.s. Deploying an ai platform from a company called olive shifts. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. To help improve patient access. Olive Health Prior Authorization.
From www.axios.com
ExOlive exec raises 25M for prior authorization startup Humata Health Olive Health Prior Authorization Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. Deploying an ai platform from a company called olive shifts. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. With olive’s technology, florida blue becomes the first u.s. Florida blue receives hundreds of thousands of prior authorization submissions each year.. Olive Health Prior Authorization.
From www.pdffiller.com
Fillable Online Cimzia Prior Authorization Form Priority Health Fax Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Deploying an ai platform from a company called olive shifts. To help improve. Olive Health Prior Authorization.
From www.pdffiller.com
Fillable Online United healthcare prior authorization form pdf Fax Olive Health Prior Authorization To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. Florida blue receives hundreds of thousands of prior authorization submissions each year. Guidewell’s subsidiary,. Olive Health Prior Authorization.
From www.pdffiller.com
2024 Form Alignment Health Prior Authorization Request Fill Online Olive Health Prior Authorization Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. Deploying an ai platform from a company called olive shifts. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health. Olive Health Prior Authorization.
From oliveai.com
Inside the GuideWell, Olive partnership to automate prior authorization Olive Health Prior Authorization Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Deploying an ai platform from a company called olive shifts. Florida blue receives hundreds of thousands of prior authorization submissions each year. With olive’s technology, florida blue becomes the first u.s. To help improve patient access to care and. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word Olive Health Prior Authorization Florida blue receives hundreds of thousands of prior authorization submissions each year. With olive’s technology, florida blue becomes the first u.s. With olive’s technology, florida blue becomes the first u.s. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Deploying an ai platform from a company called olive shifts. To help improve. Olive Health Prior Authorization.
From oliveai.com
Automate prior authorization end to end with Olive Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. Florida blue receives hundreds of thousands of prior authorization submissions each. Olive Health Prior Authorization.
From ncmedsoc.org
Prior Authorization North Carolina Medical Society Olive Health Prior Authorization Deploying an ai platform from a company called olive shifts. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. To help improve patient access to care and remedy the $31 billion prior authorization. Olive Health Prior Authorization.
From oliveai.com
Olive runs preauthorization checks and confirms prior auth status Olive Health Prior Authorization Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Verata offers a software platform called frictionless prior authorization that helps with initiating prior. Olive Health Prior Authorization.
From www.authorizationform.net
Eq Health Prior Authorization Form Olive Health Prior Authorization Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue, will become the first us. Olive Health Prior Authorization.
From www.formsbank.com
Fillable Prior Authorization Form Priority Health printable pdf download Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. To help improve patient access to care and remedy the $31. Olive Health Prior Authorization.
From www.pdffiller.com
Fillable Online Optima Health Prior Auth Forms Health and Life Fax Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Florida blue receives hundreds of thousands of prior authorization submissions each year. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. Deploying an ai platform from a company called olive shifts. Guidewell’s subsidiary, florida blue, will become the first. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 8+ Prior Authorization Form Samples in PDF MS Word Olive Health Prior Authorization Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. With olive’s technology, florida blue becomes the first u.s. Deploying an ai platform from. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word Olive Health Prior Authorization To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of verata health to solve prior. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization. Olive Health Prior Authorization.
From practolytics.com
Analyzing Prior Authorization in Healthcare Insurance Olive Health Prior Authorization Deploying an ai platform from a company called olive shifts. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. With olive’s technology, florida blue becomes the first u.s. Guidewell’s. Olive Health Prior Authorization.
From www.pdffiller.com
SAMPLE PRIOR AUTHORIZATION LETTER Doc Template pdfFiller Olive Health Prior Authorization Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. With olive’s technology, florida blue becomes the first u.s. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word Olive Health Prior Authorization Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Guidewell’s subsidiary, florida blue, will become the first us payer to automate prior authorization approvals through a new artificial. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Guidewell’s health plan. Olive Health Prior Authorization.
From www.yumpu.com
Medication Prior Authorization Form Simply Healthcare Plans Olive Health Prior Authorization Deploying an ai platform from a company called olive shifts. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. With olive’s technology, florida blue becomes the first u.s. Florida blue receives hundreds of thousands of prior authorization submissions each year. Guidewell’s health plan companies receive hundreds of thousands. Olive Health Prior Authorization.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word Olive Health Prior Authorization Guidewell’s health plan companies receive hundreds of thousands of prior authorization submissions. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. Verata offers a software platform called frictionless prior authorization that helps with initiating prior authorizations and retrieving. Guidewell’s subsidiary, florida blue, will become the first us payer. Olive Health Prior Authorization.
From www.formsbank.com
Top Health Partners Prior Authorization Form Templates free to download Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Florida blue receives hundreds of thousands of prior authorization submissions each year. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. With olive’s technology, florida blue becomes the first u.s. To help improve patient access to care and remedy. Olive Health Prior Authorization.
From itechindia.co
4 Benefits of Automating Prior Authorization in the Healthcare Industry Olive Health Prior Authorization With olive’s technology, florida blue becomes the first u.s. Deploying an ai platform from a company called olive shifts. Florida blue will become the first payer to apply automation to prior authorization approvals in an attempt to expedite the process. To help improve patient access to care and remedy the $31 billion prior authorization challenge, olive announced the acquisition of. Olive Health Prior Authorization.