Soap Note Medical School . Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. “i am here to recheck my blood pressure and talk about my headaches.” s: Nbome has a timed soap note practice document to get quicker with writing soap notes. 37 yo female presents to clinic today with follow up on blood pressure. Another thing i used to do was practice writing them in a. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients.
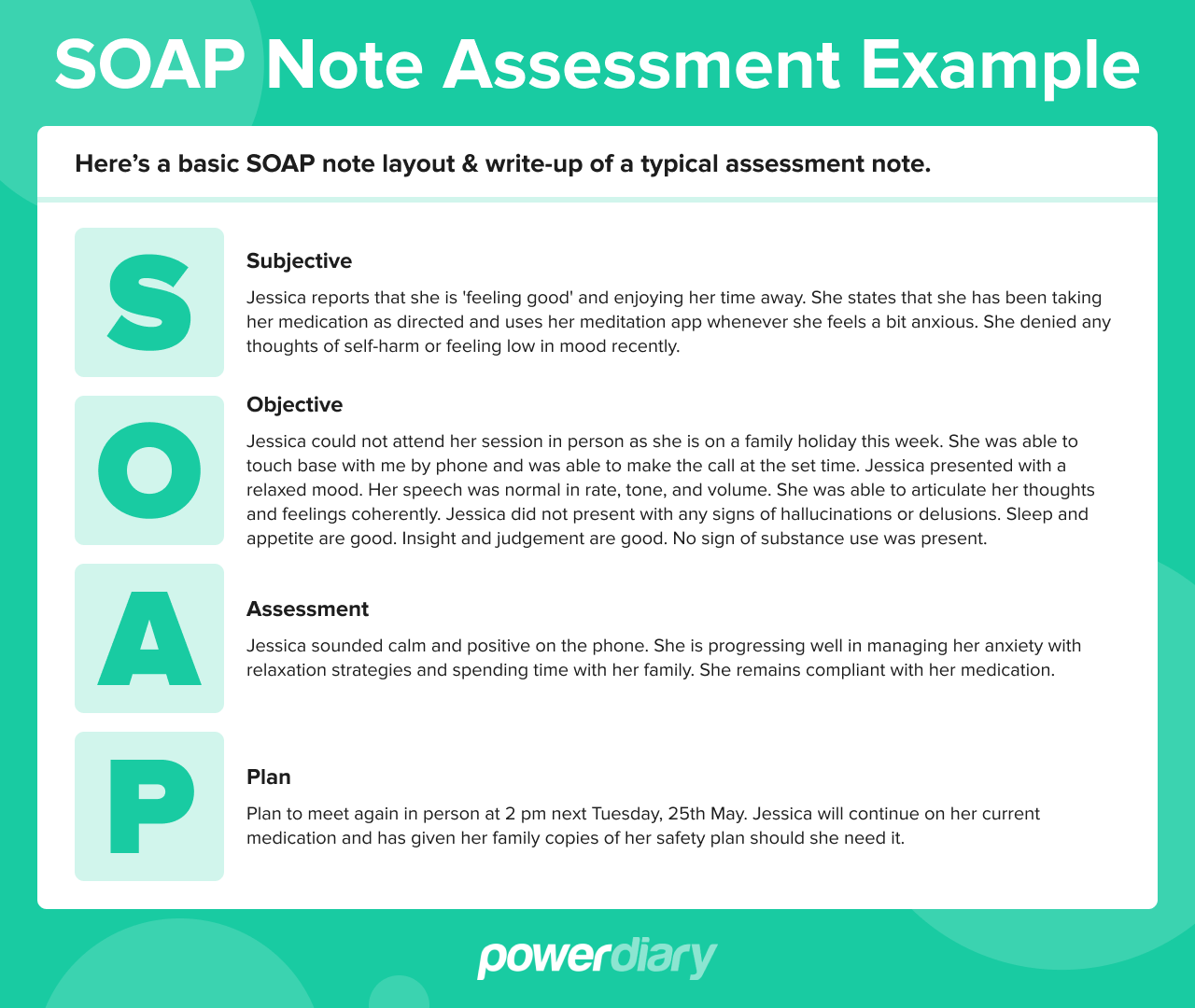
from www.powerdiary.com
Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. “i am here to recheck my blood pressure and talk about my headaches.” s: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. 37 yo female presents to clinic today with follow up on blood pressure. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Another thing i used to do was practice writing them in a. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Nbome has a timed soap note practice document to get quicker with writing soap notes.
Essential Guide to SOAP Notes SOAP Notes Example
Soap Note Medical School Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. They contain four primary sections, represented by its acronym: Nbome has a timed soap note practice document to get quicker with writing soap notes. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. “i am here to recheck my blood pressure and talk about my headaches.” s: 37 yo female presents to clinic today with follow up on blood pressure. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Another thing i used to do was practice writing them in a.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Note Medical School They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Nbome has a timed soap note practice document to get quicker with writing soap notes. Another thing i used to do was practice writing them in a. Soap notes are. Soap Note Medical School.
From davida.davivienda.com
Bcba Session Notes Template Printable Word Searches Soap Note Medical School Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Another thing i used to do. Soap Note Medical School.
From ainslieehand.blogspot.com
How To Write Good Soap Notes Ainslie Hand Soap Note Medical School Another thing i used to do was practice writing them in a. “i am here to recheck my blood pressure and talk about my headaches.” s: 37 yo female presents to clinic today with follow up on blood pressure. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers.. Soap Note Medical School.
From clinicsense.com
Free SOAP Notes Template ClinicSense Soap Note Medical School The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Nbome has a timed soap note practice document to get quicker with writing soap notes.. Soap Note Medical School.
From botswana.desertcart.com
Buy Medical Soap Notes Pocket Size H&P , Progress Note Templates Soap Note Medical School “i am here to recheck my blood pressure and talk about my headaches.” s: 37 yo female presents to clinic today with follow up on blood pressure. Nbome has a timed soap note practice document to get quicker with writing soap notes. They contain four primary sections, represented by its acronym: Another thing i used to do was practice writing. Soap Note Medical School.
From www.pinterest.com
Soap Note Etsy Soap note, Medical school essentials, Medical school Soap Note Medical School Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. “i am here to recheck my. Soap Note Medical School.
From www.studocu.com
Internal Medicine SOAP Note Michelle Shoshan SOAP Note Internal Soap Note Medical School Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. “i am here to recheck my blood pressure and talk about my headaches.” s: They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan. Soap Note Medical School.
From www.desertcart.in
Buy Medical Soap Notes Medical Soap Notes, Medical Report Sheet Soap Note Medical School Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Another thing i used to do was practice writing them in a. 37 yo female. Soap Note Medical School.
From schooloffirstaid.com
Wilderness First Aid SOAP Notes School of First Aid Soap Note Medical School Another thing i used to do was practice writing them in a. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are. Soap Note Medical School.
From www.pinterest.co.uk
Occupational Therapy Documentation Tips The OT Toolbox Occupational Soap Note Medical School The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Nbome has a timed soap note practice document to get quicker with writing soap notes. Another thing i used to do was practice writing them in a. They contain four primary sections, represented by its acronym: “i am here. Soap Note Medical School.
From www.pinterest.com
The remarkable Completed Esoap Note Sample — Nbome Regarding Soap Soap Note Medical School 37 yo female presents to clinic today with follow up on blood pressure. Nbome has a timed soap note practice document to get quicker with writing soap notes. Another thing i used to do was practice writing them in a. “i am here to recheck my blood pressure and talk about my headaches.” s: Soap notes are a standardized method. Soap Note Medical School.
From www.pinterest.com
sample soap note examples occupational therapy schools soap psychiatric Soap Note Medical School They contain four primary sections, represented by its acronym: 37 yo female presents to clinic today with follow up on blood pressure. Another thing i used to do was practice writing them in a. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Nbome has a timed soap note practice document to get quicker. Soap Note Medical School.
From www.pinterest.com
Pin on Salud Soap Note Medical School “i am here to recheck my blood pressure and talk about my headaches.” s: Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.. Soap Note Medical School.
From moussyusa.com
46+ Free Download SOAP Note Template for Your Medical Note Mous Syusa Soap Note Medical School The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: Soap notes are a standardized method of documenting patient encounters in. Soap Note Medical School.
From www.pinterest.com
Download SOAP Note with Body Printable Medical Form in 2020 Soap note Soap Note Medical School Nbome has a timed soap note practice document to get quicker with writing soap notes. 37 yo female presents to clinic today with follow up on blood pressure. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient. Soap Note Medical School.
From www.pinterest.com
SOAP Notes 101 Teaching Medical Charting! Great for Health Science Soap Note Medical School Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. 37 yo female presents to clinic today with follow up on blood pressure. Soap notes are a standardized method of documenting. Soap Note Medical School.
From www.pinterest.com
How to create a Soap Note? This medical soap note covers the most Soap Note Medical School “i am here to recheck my blood pressure and talk about my headaches.” s: Nbome has a timed soap note practice document to get quicker with writing soap notes. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. 37 yo female presents to clinic today with follow up on blood pressure. The soap. Soap Note Medical School.
From medicalaid.org
Understanding SOAP Notes for Clinical Rotations International Medical Aid Soap Note Medical School 37 yo female presents to clinic today with follow up on blood pressure. “i am here to recheck my blood pressure and talk about my headaches.” s: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Nbome has a timed soap note practice document to get quicker with writing soap notes. They contain. Soap Note Medical School.
From resumeglop.weebly.com
Easybee speech hterapy soap note resumeglop Soap Note Medical School The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Another thing i used to do was practice writing them in a. Nbome has a timed soap note practice document to get quicker with writing soap notes. Soap notes are a way for healthcare providers to document patient data. Soap Note Medical School.
From www.pinterest.com
Prescription Pad, Nursing Notes, Nursing Tips, Soap Note, Software Soap Note Medical School Another thing i used to do was practice writing them in a. “i am here to recheck my blood pressure and talk about my headaches.” s: 37 yo female presents to clinic today with follow up on blood pressure. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track. Soap Note Medical School.
From www.scribd.com
Sample Soap Note PDF Soap Note Medical School Another thing i used to do was practice writing them in a. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. The subjective, objective, assessment and plan (soap) note is. Soap Note Medical School.
From in.pinterest.com
First Aid CPD SOAP 👀⠀ ⠀ SOAP is a medical acronym used to remember Soap Note Medical School Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Nbome has a timed soap note practice document to get quicker with writing soap notes. Soap notes are a specific format. Soap Note Medical School.
From www.template.net
Internal Medicine Soap Note Template Edit Online & Download Example Soap Note Medical School The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. “i am here to recheck my blood pressure and talk about my headaches.” s: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap format can be one of the most. Soap Note Medical School.
From www.typecalendar.com
Free Printable SOAP Note Templates [PDF, Word] Soap Note Medical School Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Nbome has a timed soap note practice document to get quicker with writing soap notes. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Another thing i used to do. Soap Note Medical School.
From dl-uk.apowersoft.com
Free Printable Soap Notes Soap Note Medical School Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. 37 yo female presents to clinic today with follow up on blood pressure. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They. Soap Note Medical School.
From www.pinterest.com
Soap Notes Example Check more at Soap Note Medical School 37 yo female presents to clinic today with follow up on blood pressure. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. They contain four primary sections, represented by its. Soap Note Medical School.
From template.mapadapalavra.ba.gov.br
Psychiatry Soap Note Template Soap Note Medical School Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. 37 yo female presents to. Soap Note Medical School.
From templates.rjuuc.edu.np
Aba Notes Templates Soap Note Medical School The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. They contain four primary sections, represented by its acronym: 37 yo female presents to clinic today with follow up on blood pressure. Soap notes are a standardized method of documenting patient encounters in medical and healthcare. Soap Note Medical School.
From autonotes.ai
How to Write a Mental Health SOAP Note AutoNotes Soap Note Medical School 37 yo female presents to clinic today with follow up on blood pressure. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. They contain four primary sections, represented by its acronym: Nbome has a timed soap note practice document to get quicker with writing soap notes. Another thing. Soap Note Medical School.
From www.pinterest.com
46+ Free Download SOAP Note Template for Your Medical Note Soap note Soap Note Medical School Another thing i used to do was practice writing them in a. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. “i am here to recheck my blood pressure and talk about my headaches.” s: 37 yo female presents. Soap Note Medical School.
From www.vrogue.co
Printable Soap Progress Notes Soap Note Notes Templat vrogue.co Soap Note Medical School 37 yo female presents to clinic today with follow up on blood pressure. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Another thing i used to do was. Soap Note Medical School.
From www.pinterest.com.mx
Free Soap Notes Templates for Busy Healthcare Professionals Soap note Soap Note Medical School Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. 37 yo female presents to clinic today with follow up on blood pressure. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and. Soap Note Medical School.
From www.pinterest.com
Soap Note Example Nurse Practitioner All You Need To Know Soap note Soap Note Medical School “i am here to recheck my blood pressure and talk about my headaches.” s: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a specific format for writing progress notes. Soap Note Medical School.
From www.vrogue.co
Image Result For Soap Notes Examples Occupational The vrogue.co Soap Note Medical School They contain four primary sections, represented by its acronym: Another thing i used to do was practice writing them in a. 37 yo female presents to clinic today with follow up on blood pressure. “i am here to recheck my blood pressure and talk about my headaches.” s: Soap notes are a way for healthcare providers to document patient data. Soap Note Medical School.
From www.studocu.com
Example Soap Note (2) soap 4015cl Example Soap Note From nbome Soap Note Medical School 37 yo female presents to clinic today with follow up on blood pressure. “i am here to recheck my blood pressure and talk about my headaches.” s: Nbome has a timed soap note practice document to get quicker with writing soap notes. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format. Soap Note Medical School.