Chorus Community Health Plan Prior Authorization List . prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. Epo the summary of benefits. To learn more about specific plan authorization requirements, visit the individual plan authorization. prior authorization is a process where your provider must obtain approval from your health plan before. Chorus community health plans coverage for: if you need assistance accessing information or documents on the chorus community health plans website and. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. please review the list to see if the medication requires a prior authorization and if it will be processed through the. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them.
from www.planforms.net
prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. prior authorization is a process where your provider must obtain approval from your health plan before. Epo the summary of benefits. please review the list to see if the medication requires a prior authorization and if it will be processed through the. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. if you need assistance accessing information or documents on the chorus community health plans website and. To learn more about specific plan authorization requirements, visit the individual plan authorization. Chorus community health plans coverage for: to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug.
Allcare Health Plan Prior Authorization Form
Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: To learn more about specific plan authorization requirements, visit the individual plan authorization. if you need assistance accessing information or documents on the chorus community health plans website and. prior authorization is a process where your provider must obtain approval from your health plan before. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Epo the summary of benefits. prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. Chorus community health plans coverage for: please review the list to see if the medication requires a prior authorization and if it will be processed through the. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them.
From www.yumpu.com
Medication Prior Authorization Form Simply Healthcare Plans Chorus Community Health Plan Prior Authorization List prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. if you need assistance accessing information or documents on the chorus community health plans website and. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Epo the summary of benefits.. Chorus Community Health Plan Prior Authorization List.
From www.phoenixvirtualstaff.com
The Complete Guide to Prior Authorization Navigating the Complex Chorus Community Health Plan Prior Authorization List please review the list to see if the medication requires a prior authorization and if it will be processed through the. Chorus community health plans coverage for: to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. prior authorization form for prescription drug benefits if you have questions. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
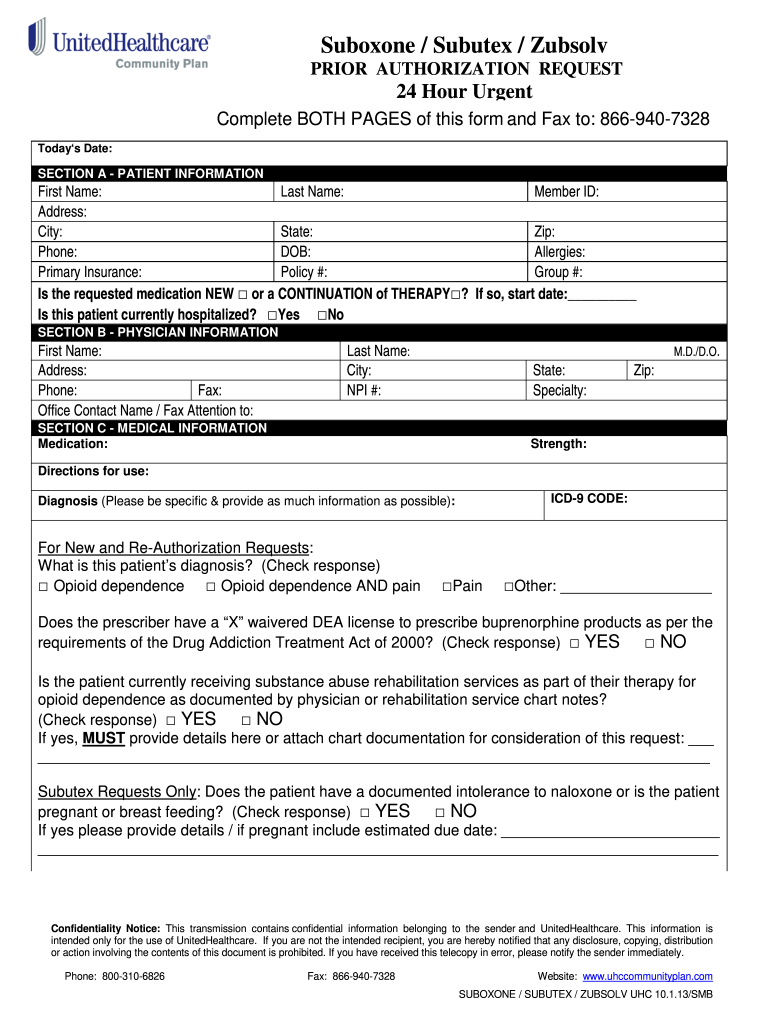
United Healthcare Community Plan Pre Authorization Form Chorus Community Health Plan Prior Authorization List prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. please review the list to see if the medication requires a prior authorization and if it will be processed through the.. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Health First Health Plans Prior Authorization Forms Chorus Community Health Plan Prior Authorization List to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Chorus community health plans coverage for: prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. Epo the summary of benefits. please review the list to see if the. Chorus Community Health Plan Prior Authorization List.
From support.foodsmart.co
Chorus Community Health Plan App registration Zipongo Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: Epo the summary of benefits. prior authorization is a process where your provider must obtain approval from your health plan before. To learn more about specific plan authorization requirements, visit the individual plan authorization. prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. . Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Harmony Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. To learn more about specific plan authorization requirements, visit the individual plan authorization. if you need assistance accessing information or documents on the chorus community health plans website and. prior authorization is a process where your provider must. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Prior Authorization Request Form Printable Pdf Download Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: prior authorization is a process where your provider must obtain approval from your health plan before. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. To learn more about specific plan authorization requirements, visit the individual plan authorization. please review the. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Carefirst Community Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. please review the list to see if the medication requires a prior authorization and if it will be processed through the. prior authorization is a process where your provider must obtain approval from your. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Health Partners Plans Prior Authorization Form Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. please review the list to see if the medication requires a prior authorization and if it will be processed through the. Epo the summary of benefits. to check a cchp plan drug. Chorus Community Health Plan Prior Authorization List.
From dokumen.tips
(PDF) 2016 and 2017 Prior Authorization List and Quick Reference Chorus Community Health Plan Prior Authorization List if you need assistance accessing information or documents on the chorus community health plans website and. Epo the summary of benefits. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. To learn more about specific plan authorization requirements, visit the individual plan authorization. Chorus community health plans coverage. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Allcare Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. prior authorization is a process where your provider must obtain approval from your health plan before. if you need assistance accessing information or documents on the chorus community health plans website and. to check a cchp plan. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Upmc Health Plan Medication Prior Authorization Form Chorus Community Health Plan Prior Authorization List To learn more about specific plan authorization requirements, visit the individual plan authorization. if you need assistance accessing information or documents on the chorus community health plans website and. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Chorus community health plans coverage for: prior authorization —. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Prior Authorization Form United Healthcare Community Plan Chorus Community Health Plan Prior Authorization List To learn more about specific plan authorization requirements, visit the individual plan authorization. Chorus community health plans coverage for: if you need assistance accessing information or documents on the chorus community health plans website and. please review the list to see if the medication requires a prior authorization and if it will be processed through the. Epo the. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Allcare Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. please review the list to see if the medication requires a prior authorization and if it will be processed through the. To learn more about specific plan authorization requirements, visit the individual plan authorization. prior authorization is a. Chorus Community Health Plan Prior Authorization List.
From www.linkedin.com
Chorus Community Health Plans on LinkedIn Children's Community Health Chorus Community Health Plan Prior Authorization List To learn more about specific plan authorization requirements, visit the individual plan authorization. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Epo the summary of benefits. if you need assistance accessing information or documents on the chorus community health plans website and. prior authorization — prior. Chorus Community Health Plan Prior Authorization List.
From www.pdffiller.com
Fillable Online ppuc prior authorization request form Community Care Chorus Community Health Plan Prior Authorization List prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. Chorus community health plans coverage for: To learn more about specific plan authorization requirements, visit the individual plan authorization. prior authorization is a process where your provider must obtain approval from your health plan before. please review the. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Prior Authorization Form United Healthcare Community Plan Chorus Community Health Plan Prior Authorization List Epo the summary of benefits. Chorus community health plans coverage for: prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. prior authorization is a process where your provider must obtain approval from your health plan before. if you need assistance accessing information or documents on the chorus community health. Chorus Community Health Plan Prior Authorization List.
From chorushealthplans.org
Member Resources Chorus Community Health Plans Chorus Community Health Plan Prior Authorization List prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. To learn more about specific plan authorization requirements, visit the individual plan authorization. Epo the summary of benefits. Chorus community health plans coverage for: please review the list to see if the medication requires a prior authorization and if. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Blue Cross Community Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Chorus community health plans coverage for: please review the list to see if the medication requires a prior authorization and if it will be processed through the. prior authorization is a process where your provider must obtain approval. Chorus Community Health Plan Prior Authorization List.
From www.signnow.com
Community Health Plan Prior Authorization 20202024 Form Fill Out and Chorus Community Health Plan Prior Authorization List to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. prior authorization is a process where your provider must obtain approval from your health plan before. prior authorization. Chorus Community Health Plan Prior Authorization List.
From www.sampleforms.com
FREE 8+ Sample Prior Authorization Forms in PDF MS Word Chorus Community Health Plan Prior Authorization List prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. Chorus community health plans coverage for: prior authorization is a process where your provider must obtain approval from your health plan before. prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
FREE 35 Sample Authorization Forms In PDF Chorus Community Health Plan Prior Authorization List please review the list to see if the medication requires a prior authorization and if it will be processed through the. Epo the summary of benefits. prior authorization is a process where your provider must obtain approval from your health plan before. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found. Chorus Community Health Plan Prior Authorization List.
From formspal.com
Prior Authorization Form ≡ Fill Out Printable PDF Forms Online Chorus Community Health Plan Prior Authorization List prior authorization is a process where your provider must obtain approval from your health plan before. Epo the summary of benefits. please review the list to see if the medication requires a prior authorization and if it will be processed through the. To learn more about specific plan authorization requirements, visit the individual plan authorization. prior authorization. Chorus Community Health Plan Prior Authorization List.
From www.sampleforms.com
FREE 41+ Authorization Forms in PDF Excel MS word Chorus Community Health Plan Prior Authorization List prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. Epo the summary of benefits. prior authorization is a process where your provider must obtain approval from your health plan before. To learn more about specific plan authorization requirements, visit the individual plan authorization. please review the list to see. Chorus Community Health Plan Prior Authorization List.
From www.pdffiller.com
Fillable Online United Healthcare Community Plan Prior Authorization Chorus Community Health Plan Prior Authorization List to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. please review the list to see if the medication requires a prior authorization and if it will be processed through the. prior authorization is a process where your provider must obtain approval from your health plan before. . Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Community Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List To learn more about specific plan authorization requirements, visit the individual plan authorization. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. prior authorization is a process where your provider. Chorus Community Health Plan Prior Authorization List.
From www.pdffiller.com
Fillable Online US Family Health Plan Prior Authorization Form for Chorus Community Health Plan Prior Authorization List prior authorization is a process where your provider must obtain approval from your health plan before. please review the list to see if the medication requires a prior authorization and if it will be processed through the. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. Chorus. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Blue Cross Community Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: Epo the summary of benefits. To learn more about specific plan authorization requirements, visit the individual plan authorization. if you need assistance accessing information or documents on the chorus community health plans website and. please review the list to see if the medication requires a prior authorization and if it will be. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Florida Healthcare Plans Prior Authorization Form Chorus Community Health Plan Prior Authorization List please review the list to see if the medication requires a prior authorization and if it will be processed through the. Epo the summary of benefits. prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for. if you need assistance accessing information or documents on the chorus community health plans. Chorus Community Health Plan Prior Authorization List.
From medicare.chpw.org
Prior Authorization 2024 Changes Community Health Plan of Washington Chorus Community Health Plan Prior Authorization List prior authorization is a process where your provider must obtain approval from your health plan before. please review the list to see if the medication requires a prior authorization and if it will be processed through the. Chorus community health plans coverage for: prior authorization — prior approval for certain treatment and services — may be required. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Upper Peninsula Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List if you need assistance accessing information or documents on the chorus community health plans website and. please review the list to see if the medication requires a prior authorization and if it will be processed through the. Chorus community health plans coverage for: prior authorization form for prescription drug benefits if you have questions about our prior. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Sharp Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List Epo the summary of benefits. to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. prior authorization is a process where your provider must obtain approval from your health plan before. prior authorization form for prescription drug benefits if you have questions about our prior authorization requirements for.. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
First Choice Health Plan Prior Authorization Form Chorus Community Health Plan Prior Authorization List Chorus community health plans coverage for: please review the list to see if the medication requires a prior authorization and if it will be processed through the. Epo the summary of benefits. prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. prior authorization is a process where. Chorus Community Health Plan Prior Authorization List.
From drive.google.com
Medical Prior Authorization List.pdf Google Drive Chorus Community Health Plan Prior Authorization List to check a cchp plan drug list, a comprehensive formulary, and pharmacy can be found below under cchp drug. prior authorization is a process where your provider must obtain approval from your health plan before. if you need assistance accessing information or documents on the chorus community health plans website and. Epo the summary of benefits. To. Chorus Community Health Plan Prior Authorization List.
From www.planforms.net
Unitedhealthcare Community Plan Medical Prior Authorization Form Chorus Community Health Plan Prior Authorization List prior authorization — prior approval for certain treatment and services — may be required before cchp will cover them. please review the list to see if the medication requires a prior authorization and if it will be processed through the. if you need assistance accessing information or documents on the chorus community health plans website and. To. Chorus Community Health Plan Prior Authorization List.