Soap Notes Are . Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a specific format for writing progress notes as a behavioral health clinician.
from templatelab.com
We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. The acronym stands for subjective,. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method for documenting patient information in healthcare. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers.
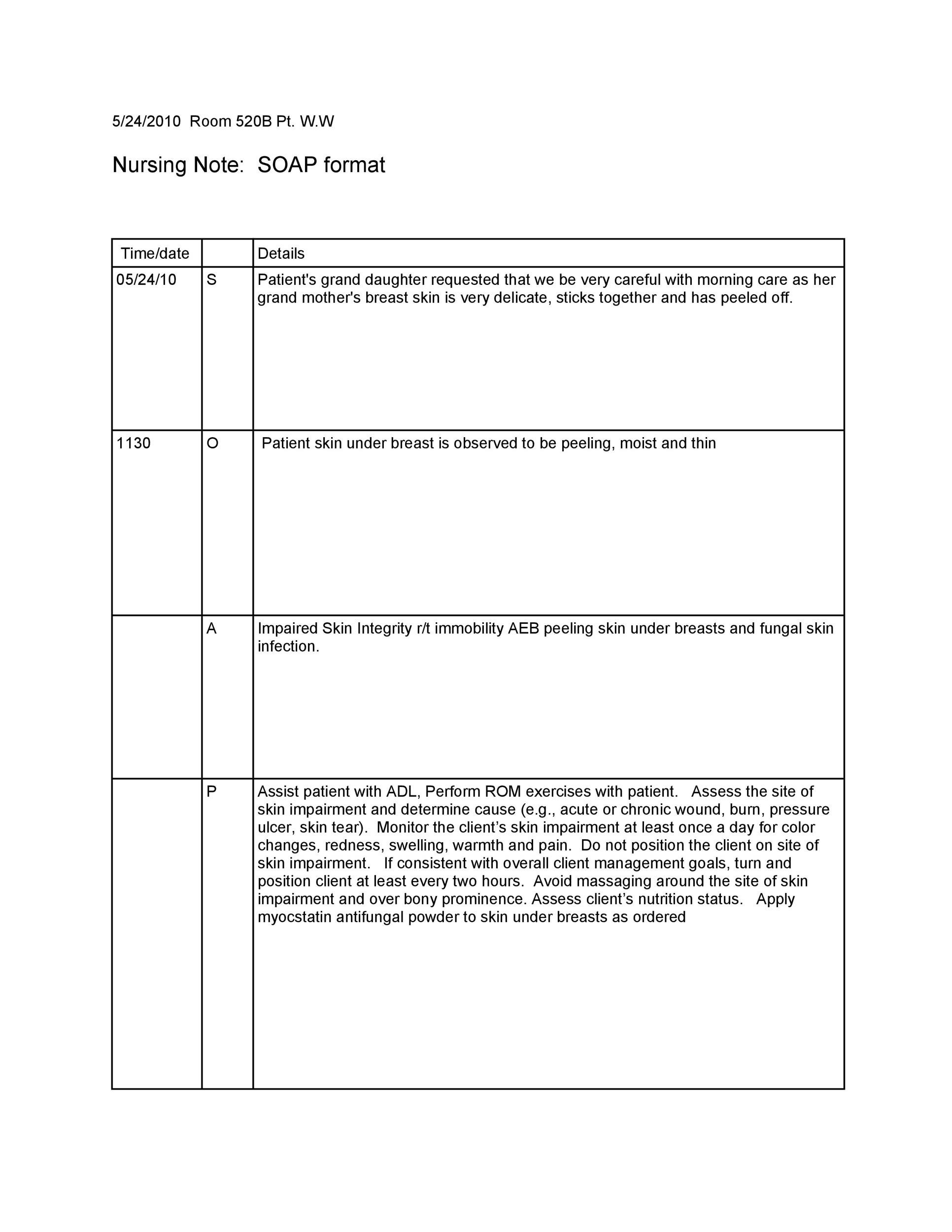
40 Fantastic SOAP Note Examples & Templates Template Lab
Soap Notes Are The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The acronym stands for subjective,. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a specific format for writing progress notes as a behavioral health clinician.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Notes Are The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing. Soap Notes Are.
From www.wordtemplatesonline.net
28 Best Soap Note Examples Free Templates Soap Notes Are They contain four primary sections, represented by its acronym: We’ve also compiled some soap. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable. Soap Notes Are.
From www.powerdiary.com
SOAP Notes for Occupational Therapy OT SOAP Note Examples Soap Notes Are The acronym stands for subjective,. They contain four primary sections, represented by its acronym: Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes include a statement about relevant client behaviors or. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a standardized method. Soap Notes Are.
From www.capterra.com
Free Soap Notes Templates for Busy Healthcare Professionals Capterra Soap Notes Are Soap notes are a standardized method for documenting patient information in healthcare. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a. Soap Notes Are.
From dev.ems-ce.com
Occupational Therapy Soap Note Template Soap Notes Are They contain four primary sections, represented by its acronym: The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. We’ve also compiled some soap. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method of documenting. Soap Notes Are.
From mavink.com
Ejemplo De Nota Soap Soap Notes Are In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented. Soap Notes Are.
From clinicsense.com
How To Write Occupational Therapy SOAP Notes Soap Notes Are We’ve also compiled some soap. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The acronym stands for subjective,. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Are Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. They contain four primary. Soap Notes Are.
From gertycancer.weebly.com
Soap notes gertycancer Soap Notes Are In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. Soap Notes Are.
From www.wordtemplatesonline.net
35+ SOAP Note Examples (Blank Formats & Writing Tips) Soap Notes Are They contain four primary sections, represented by its acronym: Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We’ve also compiled some soap. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more. Soap Notes Are.
From clinicsense.com
How to Write Effective Massage Therapy SOAP Notes Soap Notes Are Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. In this article, we’ll. Soap Notes Are.
From practicebetter.io
Mastering SOAP Notes as a Wellness Professional Practice Better Soap Notes Are In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The acronym stands for subjective,. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We’ve also compiled some soap. Soap notes are a standardized method of documenting patient encounters in. Soap Notes Are.
From quenza.com
SOAP Notes for Speech Therapy Ultimate Guide (& Examples) Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. They contain four primary sections, represented by its acronym: Soap notes are a standardized. Soap Notes Are.
From www.wordtemplatesonline.net
How to Write a SOAP Note (with SOAP Note Examples) Soap Notes Are The acronym stands for subjective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. They. Soap Notes Are.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are. Soap Notes Are.
From positivepsychology.com
What are SOAP Notes in Counseling? (+ Examples) Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. The acronym stands for subjective,. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),.. Soap Notes Are.
From canadianpa.ca
How to write a SOAP note — CANADIAN PA Soap Notes Are In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. They contain four primary sections, represented by its acronym: Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Soap notes are a standardized method for. Soap Notes Are.
From www.carepatron.com
SOAP Notes Template & Example Free PDF Download Soap Notes Are Soap notes are a standardized method for documenting patient information in healthcare. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient. Soap Notes Are.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Notes Are Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. The acronym stands for subjective,. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable,. Soap Notes Are.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Soap notes are a standardized method for documenting patient information in. Soap Notes Are.
From www.youtube.com
How to Write SOAP Notes YouTube Soap Notes Are Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The acronym stands for subjective,. They contain four primary sections, represented by its acronym: We’ve also compiled some soap. Soap notes include a statement about relevant client behaviors or status. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Are Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Are Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We’ve also compiled some soap. The subjective, objective, assessment and plan. Soap Notes Are.
From www.otdude.com
SOAP Notes Cheat Sheet for Occupational Therapy Documentation OT Dude Soap Notes Are Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a way for. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Notes Are In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The acronym stands for subjective,. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Notes Are Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a standardized method for documenting patient information in healthcare. The acronym stands for subjective,. In this article, we’ll cover how to write soap notes,. Soap Notes Are.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Notes Are The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. We’ve also compiled some soap. They contain four primary sections, represented by its acronym: In this article, we’ll cover how to write soap notes,. Soap Notes Are.
From mavink.com
Occupational Therapy Soap Notes Examples Soap Notes Are Soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. They contain four primary sections, represented by its acronym: The acronym stands for subjective,. Soap notes are a specific format for writing progress notes. Soap Notes Are.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Notes Are We’ve also compiled some soap. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. In this article, we’ll cover. Soap Notes Are.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. In this article, we’ll cover how to write soap. Soap Notes Are.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Soap Notes Are We’ve also compiled some soap. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method of. Soap Notes Are.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Notes Are Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and measurable data (objective),. We’ve also compiled some soap.. Soap Notes Are.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Notes Are Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: The acronym stands for subjective,. We’ve also compiled some soap. Soap notes are a standardized method of documenting patient encounters in medical and. Soap Notes Are.
From www.artemisaba.com
ABA SOAP Notes Tips, Examples & Template Artemis ABA Soap Notes Are We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently. Soap Notes Are.