What Is A Prior Authorization Request . Some prescription drugs require prior authorization before reimbursement is considered. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. This section will define prior authorization, explaining its purpose and significance in the healthcare system. What is a prior authorization. To determine if a drug requires. Special authorization and prior authorization are. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. What are prior authorization and special authorization?
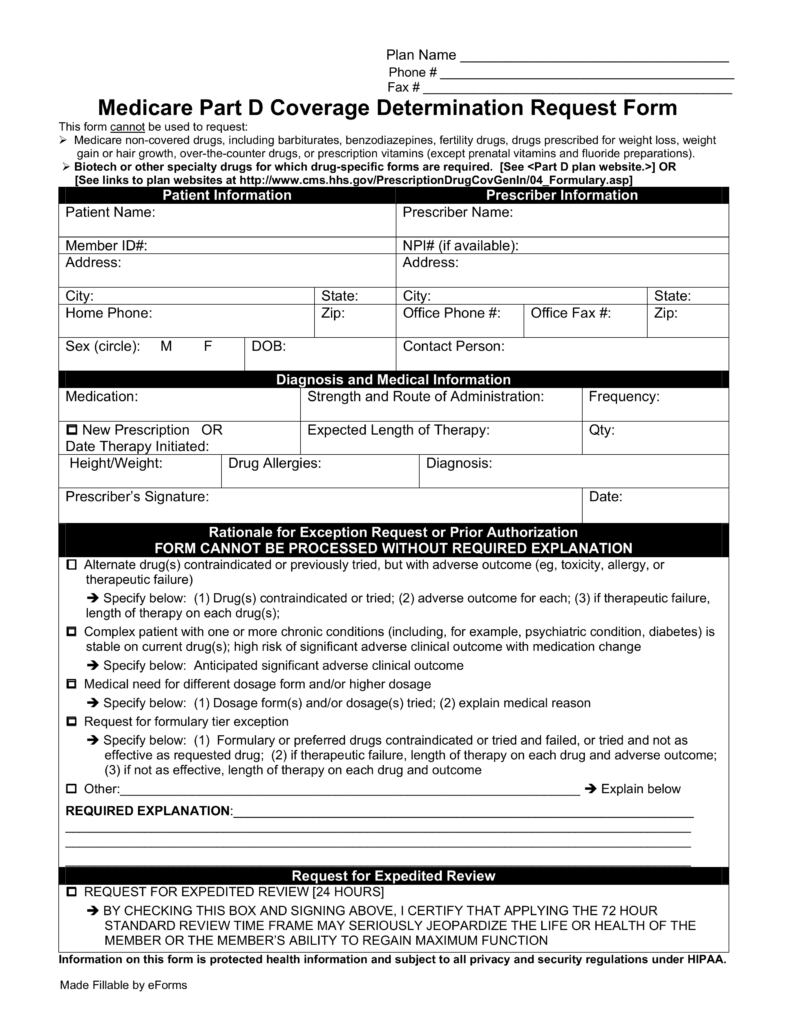
from eforms.com
To determine if a drug requires. Special authorization and prior authorization are. Some prescription drugs require prior authorization before reimbursement is considered. This section will define prior authorization, explaining its purpose and significance in the healthcare system. What is a prior authorization. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. What are prior authorization and special authorization?
Free Medicare Prior (Rx) Authorization Form PDF eForms
What Is A Prior Authorization Request What is a prior authorization. What is a prior authorization. This section will define prior authorization, explaining its purpose and significance in the healthcare system. To determine if a drug requires. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. Special authorization and prior authorization are. What are prior authorization and special authorization? Some prescription drugs require prior authorization before reimbursement is considered.
From www.uslegalforms.com
SCAN Prior Authorization Request Form Fill and Sign Printable What Is A Prior Authorization Request What are prior authorization and special authorization? To determine if a drug requires. This section will define prior authorization, explaining its purpose and significance in the healthcare system. What is a prior authorization. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 8+ Sample Prior Authorization Forms in PDF MS Word What Is A Prior Authorization Request To determine if a drug requires. What is a prior authorization. Some prescription drugs require prior authorization before reimbursement is considered. What are prior authorization and special authorization? This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your. What Is A Prior Authorization Request.
From www.signnow.com
Massachusetts Standard Prior Authorization 20162024 Form Fill Out What Is A Prior Authorization Request This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. What are prior authorization and special authorization? Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not. What Is A Prior Authorization Request.
From eforms.com
Free Medicare Prior (Rx) Authorization Form PDF eForms What Is A Prior Authorization Request To determine if a drug requires. What are prior authorization and special authorization? Special authorization and prior authorization are. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This section will define prior authorization, explaining its purpose and significance in the healthcare system. Prior authorization is the approval from. What Is A Prior Authorization Request.
From www.formsbank.com
Fillable Prior Authorization Request Form printable pdf download What Is A Prior Authorization Request Special authorization and prior authorization are. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. What is a prior authorization. Some prescription drugs require. What Is A Prior Authorization Request.
From www.formsbank.com
Prior Authorization Request Form printable pdf download What Is A Prior Authorization Request To determine if a drug requires. Some prescription drugs require prior authorization before reimbursement is considered. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. What are prior authorization and special authorization? What is a prior authorization. Prior authorization is the approval from your. What Is A Prior Authorization Request.
From eforms.com
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms What Is A Prior Authorization Request What is a prior authorization. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This section will define prior authorization, explaining its purpose and significance in the healthcare system. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word What Is A Prior Authorization Request This section will define prior authorization, explaining its purpose and significance in the healthcare system. Some prescription drugs require prior authorization before reimbursement is considered. Special authorization and prior authorization are. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. What is a prior authorization. What are prior authorization. What Is A Prior Authorization Request.
From www.formsbank.com
Fillable Standard Prior Authorization Request Form United Healthcare What Is A Prior Authorization Request This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. To determine if a drug requires. This section will define prior authorization, explaining its purpose and significance in the healthcare system. Some prescription drugs require prior authorization before reimbursement is considered. Special authorization and prior. What Is A Prior Authorization Request.
From www.signnow.com
Benecard Prior Authorization Form Complete with ease airSlate SignNow What Is A Prior Authorization Request What is a prior authorization. To determine if a drug requires. Special authorization and prior authorization are. Some prescription drugs require prior authorization before reimbursement is considered. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. This section will. What Is A Prior Authorization Request.
From www.signnow.com
Medication Prior Authorization Request Form UnitedHealthcare Fill Out What Is A Prior Authorization Request What is a prior authorization. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Some prescription drugs require prior authorization before reimbursement is considered. To determine if a drug requires. What are prior authorization and special authorization? Prior authorization. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 10+ Sample Medicare Forms in PDF MS Word What Is A Prior Authorization Request This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Special authorization and prior authorization are. What is a prior authorization. Some prescription drugs require prior authorization before reimbursement is considered. Prior authorization is the approval from your health insurance that may be required for. What Is A Prior Authorization Request.
From eforms.com
Free Prior (Rx) Authorization Forms PDF eForms What Is A Prior Authorization Request This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. What is a prior authorization. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This section will define prior authorization, explaining its purpose and. What Is A Prior Authorization Request.
From vativorx.com
What is prior authorization and how does the process work? VativoRx What Is A Prior Authorization Request This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. What is a prior authorization.. What Is A Prior Authorization Request.
From www.uslegalforms.com
IN Prior Authorization Request Form Fill and Sign Printable Template What Is A Prior Authorization Request Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. What are prior authorization and special authorization? What is a prior authorization. Special authorization and prior authorization are. To determine if a drug requires. This approval process is called prior. What Is A Prior Authorization Request.
From templates.rjuuc.edu.np
Generic Prior Authorization Form Template What Is A Prior Authorization Request This section will define prior authorization, explaining its purpose and significance in the healthcare system. What is a prior authorization. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for a. What Is A Prior Authorization Request.
From www.myndshft.com
The Ultimate Guide to Prior Authorization Myndshft What Is A Prior Authorization Request This section will define prior authorization, explaining its purpose and significance in the healthcare system. Some prescription drugs require prior authorization before reimbursement is considered. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This approval process is called prior authorization, and getting one before you get care means. What Is A Prior Authorization Request.
From www.uslegalforms.com
Caremark Prior Authorization Request Form Fill and Sign Printable What Is A Prior Authorization Request To determine if a drug requires. Special authorization and prior authorization are. What are prior authorization and special authorization? This section will define prior authorization, explaining its purpose and significance in the healthcare system. What is a prior authorization. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can. What Is A Prior Authorization Request.
From eforms.com
Free Ohio Medicaid Prior Authorization Form PDF eForms What Is A Prior Authorization Request To determine if a drug requires. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This section will define prior authorization, explaining its purpose and significance in the healthcare system. This approval process is called prior authorization, and getting one before you get care means the care is appropriate. What Is A Prior Authorization Request.
From www.formsbank.com
Fillable Medicaid Medical Surgical Prior Authorization Request What Is A Prior Authorization Request Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Special authorization and prior authorization are. What are prior authorization and special authorization? This approval process is called prior authorization, and getting one before you get care means the care. What Is A Prior Authorization Request.
From www.psychiatryatlanta.com
What is Prior Authorization? Some Mysteries Explained Atlanta What Is A Prior Authorization Request To determine if a drug requires. What is a prior authorization. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. Some prescription drugs require prior authorization before reimbursement is considered. This approval process is called prior authorization, and getting one before you get care means the care is appropriate. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word What Is A Prior Authorization Request Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. This section will define prior authorization, explaining its purpose and significance in the healthcare system. Special authorization and prior authorization are. What are prior authorization and special authorization? To determine. What Is A Prior Authorization Request.
From www.phoenixvirtualstaff.com
The Complete Guide to Prior Authorization Navigating the Complex What Is A Prior Authorization Request Some prescription drugs require prior authorization before reimbursement is considered. What are prior authorization and special authorization? To determine if a drug requires. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. This section will define prior authorization, explaining. What Is A Prior Authorization Request.
From formspal.com
Prior Authorization Form ≡ Fill Out Printable PDF Forms Online What Is A Prior Authorization Request This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Special authorization and prior authorization are. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an. What Is A Prior Authorization Request.
From www.formsbank.com
Fillable Prescription Drug Prior Authorization Request Form printable What Is A Prior Authorization Request Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Special authorization and prior authorization are. What is a prior authorization. Some prescription drugs require prior authorization before reimbursement is considered. To determine if a drug requires. This approval process. What Is A Prior Authorization Request.
From www.templateroller.com
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online What Is A Prior Authorization Request Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. To determine if a drug requires. This approval process is. What Is A Prior Authorization Request.
From eforms.com
Free Illinois Medicaid Prior (Rx) Authorization Form PDF eForms What Is A Prior Authorization Request Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. What are prior authorization and special authorization? Some prescription drugs require prior authorization before reimbursement is considered. This section will define prior authorization, explaining its purpose and significance in the healthcare system. Special authorization and prior authorization are. Prior authorization. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word What Is A Prior Authorization Request What are prior authorization and special authorization? Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. Special authorization and prior authorization are. This approval process is called prior authorization, and getting one before you get care means the care. What Is A Prior Authorization Request.
From eforms.com
Free Express Scripts Prior (Rx) Authorization Form PDF eForms What Is A Prior Authorization Request What is a prior authorization. Special authorization and prior authorization are. Some prescription drugs require prior authorization before reimbursement is considered. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency. This approval process is called prior authorization, and getting. What Is A Prior Authorization Request.
From www.formspdf.com
Simple UHC Prior Authorization Form for Everyone What Is A Prior Authorization Request What are prior authorization and special authorization? What is a prior authorization. Special authorization and prior authorization are. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for a service, treatment,. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word What Is A Prior Authorization Request To determine if a drug requires. Special authorization and prior authorization are. Some prescription drugs require prior authorization before reimbursement is considered. What are prior authorization and special authorization? This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. What is a prior authorization. Prior. What Is A Prior Authorization Request.
From www.sampleforms.com
FREE 13+ Prior Authorization Forms in PDF MS Word What Is A Prior Authorization Request Special authorization and prior authorization are. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. Some prescription drugs require prior authorization before reimbursement is considered. What is a prior authorization. This approval process is called prior authorization, and getting one before you get care means the care is appropriate. What Is A Prior Authorization Request.
From www.signnow.com
Bcbs Prior Authorization PDF 20092024 Form Fill Out and Sign What Is A Prior Authorization Request Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. This section will define prior authorization, explaining its purpose and significance in the healthcare system. To determine if a drug requires. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription. What Is A Prior Authorization Request.
From getreferralmd.com
The Shocking Truth about Prior Authorizations in Healthcare What Is A Prior Authorization Request What are prior authorization and special authorization? To determine if a drug requires. Special authorization and prior authorization are. Some prescription drugs require prior authorization before reimbursement is considered. Prior authorization does not guarantee payment, but it does make it more likely your health plan will cover the cost. What is a prior authorization. This approval process is called prior. What Is A Prior Authorization Request.
From www.sampletemplates.com
FREE 10+ Sample Authorization Request Forms in MS Word PDF What Is A Prior Authorization Request This section will define prior authorization, explaining its purpose and significance in the healthcare system. What are prior authorization and special authorization? This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. To determine if a drug requires. Prior authorization is the approval from your. What Is A Prior Authorization Request.