Cvs Caremark Prior Authorization Form Praluent . Cvs caremark administers the prescription benefit plan for the patient identified. When a pa is needed for a prescription, the member will be asked to have. If you wish to request a medicare part determination (prior authorization or exception. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A live representative will assist. Submission of the following information is necessary to initiate the prior authorization review: After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form.
from www.pdffiller.com
When a pa is needed for a prescription, the member will be asked to have. A live representative will assist. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you wish to request a medicare part determination (prior authorization or exception. Submission of the following information is necessary to initiate the prior authorization review: Cvs caremark administers the prescription benefit plan for the patient identified.
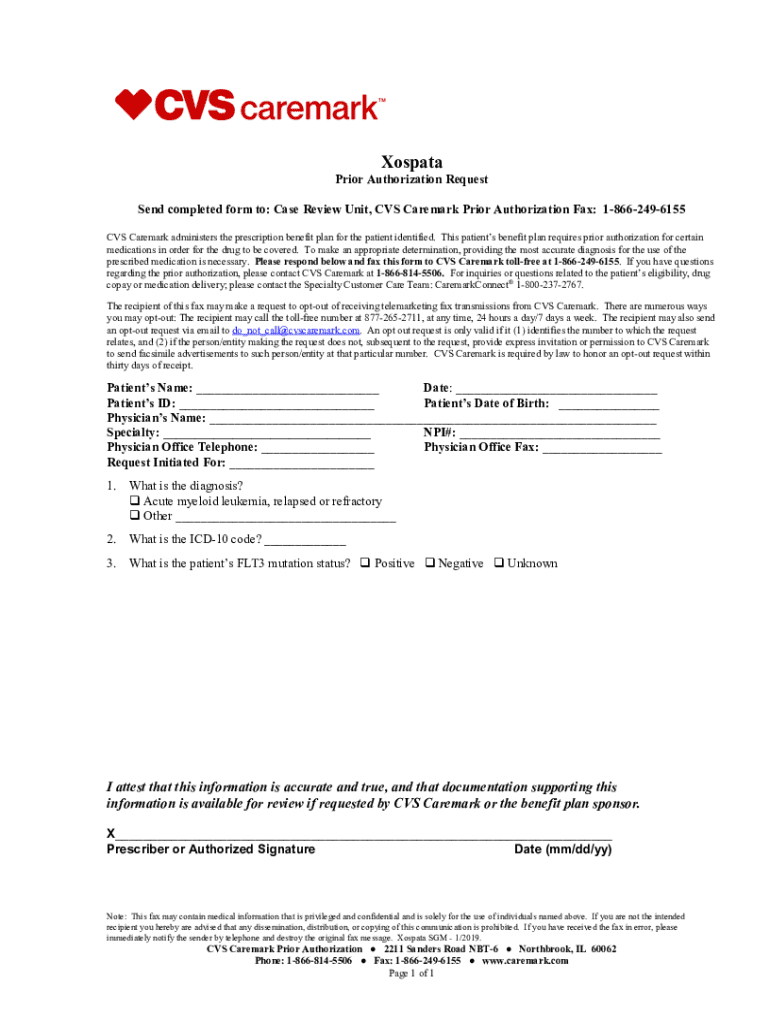
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email
Cvs Caremark Prior Authorization Form Praluent This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you wish to request a medicare part determination (prior authorization or exception. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Submission of the following information is necessary to initiate the prior authorization review: This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Cvs caremark administers the prescription benefit plan for the patient identified. When a pa is needed for a prescription, the member will be asked to have. A live representative will assist.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization HMSA Fax Email Print Cvs Caremark Prior Authorization Form Praluent When a pa is needed for a prescription, the member will be asked to have. Cvs caremark administers the prescription benefit plan for the patient identified. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Submission of the following information is necessary to initiate the prior authorization review: A live representative. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form eForms Fax Cvs Caremark Prior Authorization Form Praluent After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. When a pa is needed for a prescription, the member will be asked to have. If you wish to request a medicare part determination (prior authorization or exception. This patient’s benefit plan requires prior authorization for certain medications in order. Cvs Caremark Prior Authorization Form Praluent.
From www.authorizationform.net
Cvs Caremark Ivig Prior Authorization Form Cvs Caremark Prior Authorization Form Praluent A live representative will assist. If you wish to request a medicare part determination (prior authorization or exception. Cvs caremark administers the prescription benefit plan for the patient identified. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Submission of the following information is necessary to initiate the prior. Cvs Caremark Prior Authorization Form Praluent.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. If you wish to request a medicare part determination (prior authorization or exception. This patient’s benefit plan requires prior authorization for certain medications in order for the. Cvs Caremark Prior Authorization Form Praluent.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form Praluent If you wish to request a medicare part determination (prior authorization or exception. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. When a pa is needed for a prescription, the member will be asked to have. Cvs caremark administers the prescription benefit plan for the patient identified. Submission of the. Cvs Caremark Prior Authorization Form Praluent.
From www.dochub.com
Cvs caremark wegovy prior authorization criteria Fill out & sign Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: A live representative will assist. Cvs caremark administers the prescription benefit plan for the patient identified. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. After your doctor prescribes praluent, your health plan (insurance) may require your doctor. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Cvs Caremark Formulary Exception Prior Authorization Request Form Cvs Caremark Prior Authorization Form Praluent After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. When a pa is needed for a prescription, the member will be asked to have. Submission of the following information is necessary. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you wish to request a medicare part determination. Cvs Caremark Prior Authorization Form Praluent.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Form Praluent This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you wish to request a medicare part determination (prior authorization or exception. Cvs caremark administers the prescription benefit plan for the patient identified. Submission of the following information is necessary to initiate the prior authorization review: When a pa is needed. Cvs Caremark Prior Authorization Form Praluent.
From www.dochub.com
Caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form Praluent When a pa is needed for a prescription, the member will be asked to have. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. A live representative will assist. If you wish to request a medicare part determination (prior authorization or exception. Submission of the following information is necessary. Cvs Caremark Prior Authorization Form Praluent.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Prior Authorization Form Praluent A live representative will assist. Submission of the following information is necessary to initiate the prior authorization review: Cvs caremark administers the prescription benefit plan for the patient identified. If you wish to request a medicare part determination (prior authorization or exception. When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit. Cvs Caremark Prior Authorization Form Praluent.
From www.authorizationform.net
Caremark Specialty Pharmacy Prior Authorization Form Cvs Caremark Prior Authorization Form Praluent This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Cvs caremark administers the prescription benefit plan for the patient identified. A live representative will assist. Submission of the following information is necessary to initiate the prior authorization review: After your doctor prescribes praluent, your health plan (insurance) may require your doctor. Cvs Caremark Prior Authorization Form Praluent.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Prior Authorization Form Praluent After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. When a pa is needed for a prescription, the member will be asked to have. Submission of the following information is necessary to initiate the prior authorization review: Cvs caremark administers the prescription benefit plan for the patient identified. This. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Authorization Form Praluent After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Submission of the following information is necessary. Cvs Caremark Prior Authorization Form Praluent.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Prior Authorization Form Praluent This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. If you wish to request a medicare part determination (prior authorization or exception. When a pa is needed for a prescription, the. Cvs Caremark Prior Authorization Form Praluent.
From www.formsbank.com
Cvs Aveed Prior Authorization Request Form printable pdf download Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: Cvs caremark administers the prescription benefit plan for the patient identified. A live representative will assist. If you wish to request a medicare part determination (prior authorization or exception. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization. Cvs Caremark Prior Authorization Form Praluent.
From www.templateroller.com
Botox Passport Prior Authorization Request Form Cvs Caremark Fill Cvs Caremark Prior Authorization Form Praluent This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Cvs caremark administers the prescription benefit plan for the patient identified. Submission of the following information is necessary to initiate the prior authorization review: When a pa is needed for a prescription, the member will be asked to have. After your doctor. Cvs Caremark Prior Authorization Form Praluent.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: When a pa is needed for a prescription, the member will be asked to have. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Cvs caremark administers the prescription benefit plan for the patient identified. If. Cvs Caremark Prior Authorization Form Praluent.
From www.sampletemplates.com
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF Cvs Caremark Prior Authorization Form Praluent If you wish to request a medicare part determination (prior authorization or exception. A live representative will assist. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Cvs caremark administers the prescription benefit plan for the patient identified. When a pa is needed for a prescription, the member will. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Form Fax Email Print Cvs Caremark Prior Authorization Form Praluent This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. A live representative will assist. If you wish to request a medicare part determination (prior authorization or exception. Submission of the following. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Fill Online Cvs Caremark Prior Authorization Form Praluent Cvs caremark administers the prescription benefit plan for the patient identified. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A live representative will assist. Submission of the following information is necessary to initiate the prior authorization review: After your doctor prescribes praluent, your health plan (insurance) may require your doctor. Cvs Caremark Prior Authorization Form Praluent.
From eforms.com
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Cvs caremark administers the prescription benefit plan for the patient identified. A live representative will assist. If you wish to request a medicare part determination (prior authorization or exception.. Cvs Caremark Prior Authorization Form Praluent.
From www.authorizationform.net
Caremark Prior Authorization Form Printable Pdf Download Cvs Caremark Prior Authorization Form Praluent After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. If you wish to request a medicare part determination (prior authorization or exception. A live representative will assist. Submission of the following information is necessary to initiate the prior authorization review: Cvs caremark administers the prescription benefit plan for the. Cvs Caremark Prior Authorization Form Praluent.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form Praluent After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. When a pa is needed for a prescription, the member will be asked to have. A live representative will assist. Cvs caremark administers the prescription benefit plan for the patient identified. This patient’s benefit plan requires prior authorization for certain. Cvs Caremark Prior Authorization Form Praluent.
From www.templateroller.com
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online Cvs Caremark Prior Authorization Form Praluent If you wish to request a medicare part determination (prior authorization or exception. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. When a pa is needed for a prescription, the member will be asked to have. Cvs caremark administers the prescription benefit plan for the patient identified. This. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Authorization Form Praluent If you wish to request a medicare part determination (prior authorization or exception. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A live representative will assist. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Submission of the following. Cvs Caremark Prior Authorization Form Praluent.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form Praluent Cvs caremark administers the prescription benefit plan for the patient identified. If you wish to request a medicare part determination (prior authorization or exception. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Submission of the following information is necessary to initiate the prior authorization review: A live representative. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print Cvs Caremark Prior Authorization Form Praluent When a pa is needed for a prescription, the member will be asked to have. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. A live representative will assist. If you wish to request a medicare part determination (prior authorization or exception. Cvs caremark administers the prescription benefit plan. Cvs Caremark Prior Authorization Form Praluent.
From mungfali.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable E10 Cvs Caremark Prior Authorization Form Praluent When a pa is needed for a prescription, the member will be asked to have. Cvs caremark administers the prescription benefit plan for the patient identified. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. A live representative will assist. Submission of the following information is necessary to initiate. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email Cvs Caremark Prior Authorization Form Praluent If you wish to request a medicare part determination (prior authorization or exception. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. Submission of the following information is necessary to initiate the prior authorization review: This patient’s benefit plan requires prior authorization for certain medications in order for the. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print Cvs Caremark Prior Authorization Form Praluent When a pa is needed for a prescription, the member will be asked to have. Cvs caremark administers the prescription benefit plan for the patient identified. If you wish to request a medicare part determination (prior authorization or exception. Submission of the following information is necessary to initiate the prior authorization review: A live representative will assist. After your doctor. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Provider Resource Cvs Caremark Prior Authorization Form Praluent Submission of the following information is necessary to initiate the prior authorization review: If you wish to request a medicare part determination (prior authorization or exception. Cvs caremark administers the prescription benefit plan for the patient identified. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. A live representative will assist.. Cvs Caremark Prior Authorization Form Praluent.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Prior Authorization Form Praluent Cvs caremark administers the prescription benefit plan for the patient identified. If you wish to request a medicare part determination (prior authorization or exception. After your doctor prescribes praluent, your health plan (insurance) may require your doctor to submit a prior authorization (pa) form. When a pa is needed for a prescription, the member will be asked to have. This. Cvs Caremark Prior Authorization Form Praluent.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Prior Authorization Form Praluent A live representative will assist. When a pa is needed for a prescription, the member will be asked to have. If you wish to request a medicare part determination (prior authorization or exception. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Submission of the following information is necessary to initiate. Cvs Caremark Prior Authorization Form Praluent.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Prior Authorization Form Praluent When a pa is needed for a prescription, the member will be asked to have. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you wish to request a medicare part determination (prior authorization or exception. A live representative will assist. Cvs caremark administers the prescription benefit plan for the. Cvs Caremark Prior Authorization Form Praluent.