Soap Documentation Example . Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: Soap (subjective, objective, assessment, plan). Soap nursing notes are a type of patient progress note or nurse’s note. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
from templatelab.com
It is the documentation used to record information about encounters with patients that follows a specific format. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap (subjective, objective, assessment, plan). Soap nursing notes are a type of patient progress note or nurse’s note.
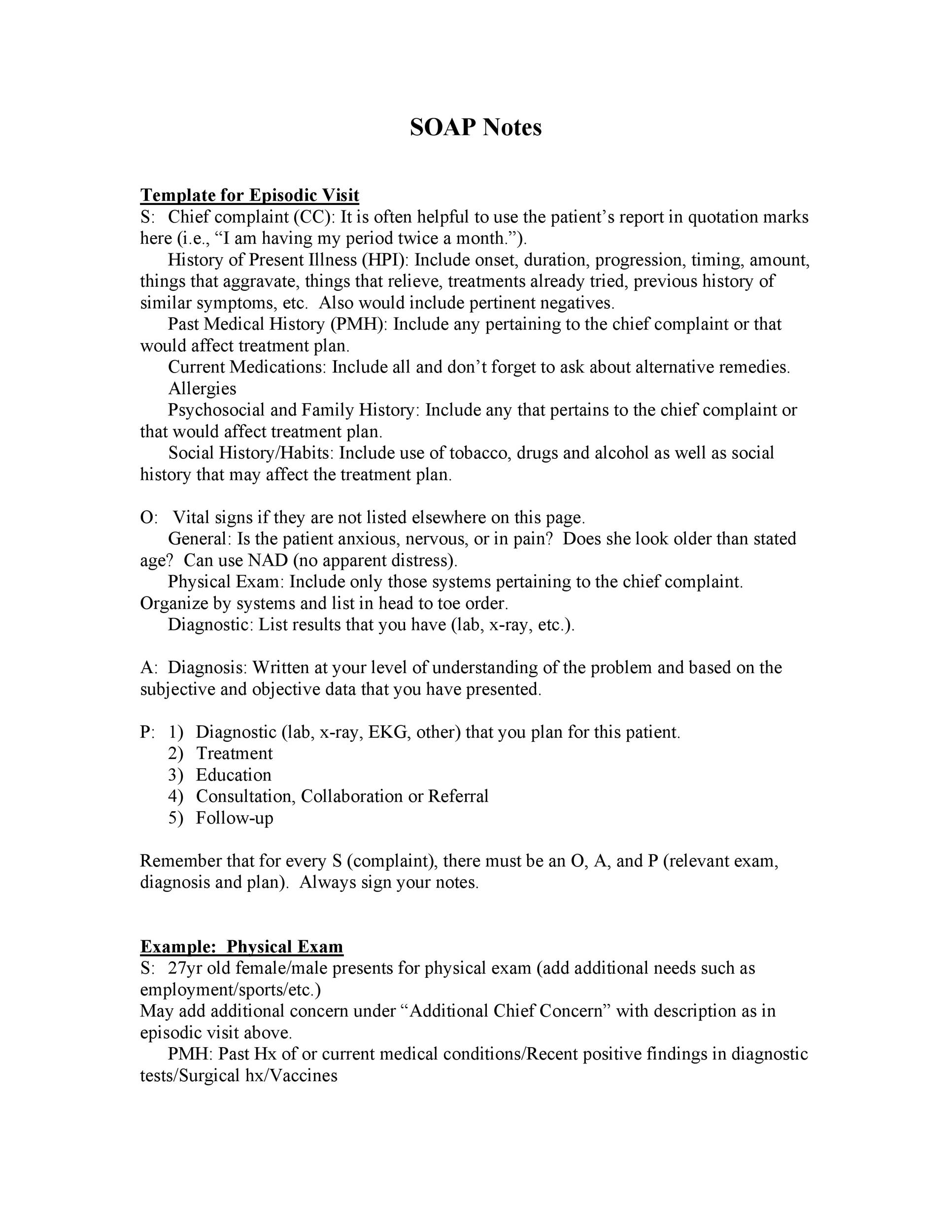
40 Fantastic SOAP Note Examples & Templates Template Lab
Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap (subjective, objective, assessment, plan). They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. It is the documentation used to record information about encounters with patients that follows a specific format.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education Soap Documentation Example Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with patients that follows a specific format. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap nursing notes are a type. Soap Documentation Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Documentation Example Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. While soap, dap, and birp notes are all structured formats for clinical documentation, they. Soap Documentation Example.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Documentation Example They contain four primary sections, represented by its acronym: Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. It is the documentation used to record information about encounters with patients that follows a specific format. The soap format can be one of the most effective ways for clinicians. Soap Documentation Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Documentation Example They contain four primary sections, represented by its acronym: While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap notes are a way for healthcare providers to document patient data more. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap (subjective, objective, assessment, plan). Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its acronym: The. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Documentation Example They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. While soap, dap, and birp notes are all structured formats for clinical. Soap Documentation Example.
From clinicsense.com
Free SOAP Notes Template ClinicSense Soap Documentation Example Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. It is the documentation used to record information about encounters with patients that follows a specific format. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap notes are a specific. Soap Documentation Example.
From www.peterainsworth.com
Soap Documentation Example Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note. Soap Documentation Example.
From otflourish.com
SOAP Note And Documentation Templates & Examples OT Flourish Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. While soap, dap,. Soap Documentation Example.
From www.clinicsource.com
Therapy Documentation Software SOAP Notes ClinicSource Soap Documentation Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap (subjective, objective, assessment, plan). It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. Using. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap (subjective, objective, assessment, plan). The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. It is the documentation used to record information about encounters with patients that follows a specific format. Using a soap note. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Documentation Example They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap nursing notes are a type of patient progress note or nurse’s note. Using a soap note format, clinicians can. Soap Documentation Example.
From www.sampletemplates.com
FREE 15+ SOAP Note Templates in PDF MS Word Soap Documentation Example Soap (subjective, objective, assessment, plan). Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap notes are a way for healthcare providers to document. Soap Documentation Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Documentation Example Soap (subjective, objective, assessment, plan). Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its acronym: The soap format can be one of the most effective ways for. Soap Documentation Example.
From www.wikihow.com
How to Write a Soap Note (with Pictures) wikiHow Soap Documentation Example While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap format can be one of the most effective ways for clinicians to. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are. Soap Documentation Example.
From www.carepatron.com
SOAP Notes For Occupational Therapy Template & Example Free PDF Download Soap Documentation Example Soap (subjective, objective, assessment, plan). They contain four primary sections, represented by its acronym: While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a specific. Soap Documentation Example.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox Soap Documentation Example Soap nursing notes are a type of patient progress note or nurse’s note. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. They contain four primary sections, represented. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap (subjective, objective, assessment, plan). The soap format can be one of the most effective ways for clinicians to document and objectively. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Documentation Example The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: It is the documentation used to record information about encounters with. Soap Documentation Example.
From studylib.net
Patient SOAP Note Charting Procedures Soap Documentation Example Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its acronym: It. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. They contain four. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap nursing notes are a type of patient progress note or nurse’s note. Soap (subjective, objective, assessment, plan). The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Documentation Example Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap nursing notes are a type of patient progress note or nurse’s note. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. The soap format can be one of the most. Soap Documentation Example.
From www.vrogue.co
Sample Soap Notes Occupational Therapy Pdf Fill Out A vrogue.co Soap Documentation Example They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. While soap,. Soap Documentation Example.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Soap Documentation Example Soap nursing notes are a type of patient progress note or nurse’s note. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap (subjective, objective, assessment, plan). While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct. Soap Documentation Example.
From www.template.net
11+ Soap Note Templates Free Sample, Example, Format Download! Soap Documentation Example Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: While soap, dap, and birp notes are all structured formats for clinical documentation, they have. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. Soap (subjective, objective, assessment, plan). While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example It is the documentation used to record information about encounters with patients that follows a specific format. Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. They contain four primary sections,. Soap Documentation Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Documentation Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Soap (subjective, objective, assessment, plan). Using a soap note format, clinicians can ensure they extract valuable information from patients in both a subjective and objective manner. It is the documentation used to record information about encounters. Soap Documentation Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Documentation Example Soap (subjective, objective, assessment, plan). Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap format can be one of the most effective ways for clinicians to document and objectively assess, diagnose, and track plans for clients. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four. Soap Documentation Example.
From www.theraplatform.com
Occupational therapy SOAP note Soap Documentation Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. While soap, dap, and birp notes are all structured formats for clinical documentation, they have distinct differences. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for healthcare providers to document patient data more efficiently and. Soap Documentation Example.