Soap Medical Chart . Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Exactly what is a soap note?. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. This guide discusses the soap framework (subjective, objective,. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare.
from studylib.net
This guide discusses the soap framework (subjective, objective,. Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a standardized method for documenting patient information in healthcare. Exactly what is a soap note?. We’ve also compiled some soap. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section.
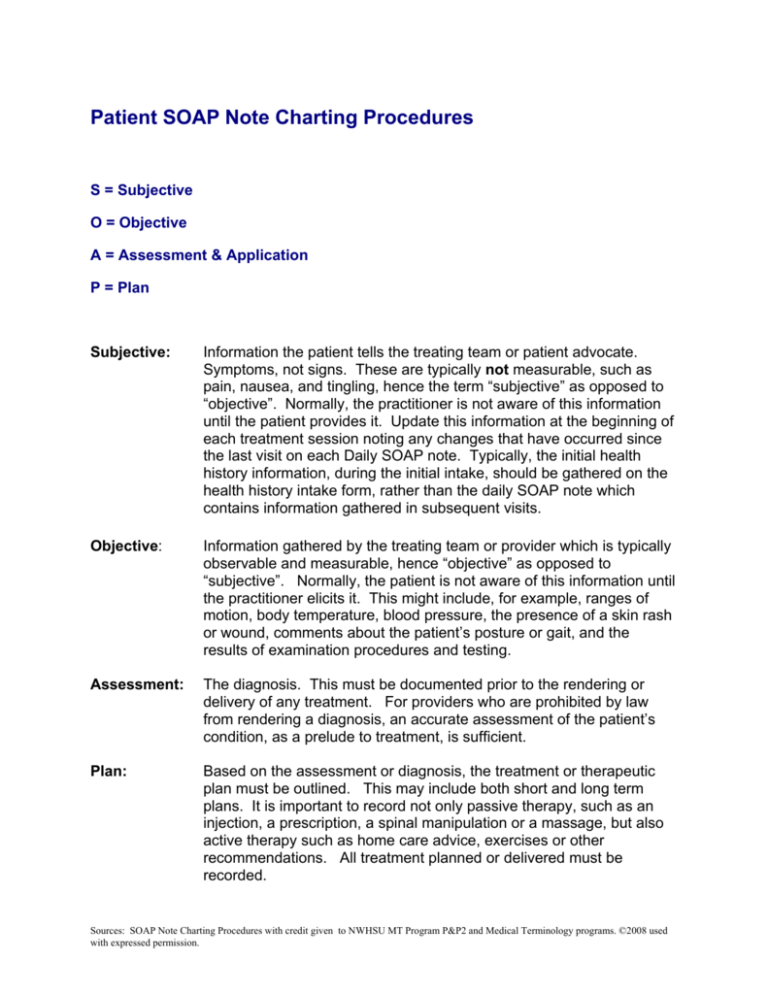
Patient SOAP Note Charting Procedures
Soap Medical Chart Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. This guide discusses the soap framework (subjective, objective,. Exactly what is a soap note?. Soap notes are a standardized method for documenting patient information in healthcare. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Documenting a patient assessment in the notes is something all medical students need to practice. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox Soap Medical Chart Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Exactly what is a soap note?. This guide discusses the soap framework (subjective, objective,. Documenting a patient assessment in the. Soap Medical Chart.
From www.scribd.com
Soap Additives Chart Ingredient Characteristics Usage Rate Note PDF Soap Medical Chart Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes. Soap Medical Chart.
From viewpoint.online
How to put the patient first in your eye examinations Viewpoint Soap Medical Chart Soap notes are a standardized method for documenting patient information in healthcare. We’ve also compiled some soap. This guide discusses the soap framework (subjective, objective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Documenting a patient assessment in the notes is something all medical students need to. Soap Medical Chart.
From canadianpa.ca
How to write a SOAP note — CANADIAN PA Soap Medical Chart Documenting a patient assessment in the notes is something all medical students need to practice. The acronym stands for subjective,. This guide discusses the soap framework (subjective, objective,. Exactly what is a soap note?. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an. Soap Medical Chart.
From covenantlifecog.com
SOAPmethodposter Soap Medical Chart The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In. Soap Medical Chart.
From www.tosurg.ca
Notes and Templates TOsurg Soap Medical Chart Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The acronym stands for subjective,. We’ve also compiled some soap. Soap. Soap Medical Chart.
From www.carepatron.com
Soap Chart & Example Free PDF Download Soap Medical Chart We’ve also compiled some soap. The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soap framework (subjective, objective,. Soap notes are a highly structured format for documenting the. Soap Medical Chart.
From www.researchgate.net
Class diagram SOAP for Medical Charts Download Scientific Diagram Soap Medical Chart The acronym stands for subjective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method for documenting patient information in healthcare. Documenting a patient assessment in. Soap Medical Chart.
From www.sampletemplates.com
FREE 8+ SOAP Note Samples in PDF, Word Soap Medical Chart The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Exactly what is a soap note?. The acronym stands for subjective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a way. Soap Medical Chart.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Medical Chart The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Exactly what is a soap note?. Documenting a patient assessment in the notes is something all medical students need to practice. Soap. Soap Medical Chart.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by Soap Medical Chart This guide discusses the soap framework (subjective, objective,. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a highly structured format for. Soap Medical Chart.
From www.academia.edu
(PDF) The SOAP Pattern for Medical Charts Eduardo Fernandez Soap Medical Chart This guide discusses the soap framework (subjective, objective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Exactly what is a soap note?. Soap—or subjective,. Soap Medical Chart.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Medical Chart The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient. Soap Medical Chart.
From www.practicefusion.com
Medical Chart and SOAP Notes Templates Practice Fusion Soap Medical Chart In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured. Soap Medical Chart.
From www.pinterest.com
soap notes with the words soap on it Soap Medical Chart We’ve also compiled some soap. The acronym stands for subjective,. Soap notes are a standardized method for documenting patient information in healthcare. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Documenting. Soap Medical Chart.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Medical Chart Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soap framework (subjective, objective,. We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Exactly what is a soap note?. Soap notes are a standardized. Soap Medical Chart.
From www.pinterest.com
SOAP chart Massage therapy, Soap note, Massage therapy techniques Soap Medical Chart Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Documenting. Soap Medical Chart.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Medical Chart Documenting a patient assessment in the notes is something all medical students need to practice. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a standardized method for documenting patient information in healthcare. Exactly what is a soap note?. Soap notes are a highly structured. Soap Medical Chart.
From www.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract Soap Medical Chart Documenting a patient assessment in the notes is something all medical students need to practice. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap). Soap Medical Chart.
From training.proz.com
SOAP Notes and Medical Charts The Nitty Gritty of Medical Soap Medical Chart In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The subjective, objective, assessment. Soap Medical Chart.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Medical Chart Documenting a patient assessment in the notes is something all medical students need to practice. The acronym stands for subjective,. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap—or subjective,. Soap Medical Chart.
From www.capterra.com
Free SOAP Notes Templates for Busy Healthcare Professionals Capterra Soap Medical Chart Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soap framework (subjective, objective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in. Soap Medical Chart.
From www.carepatron.com
SOAP Notes for Chiropractic Template & Example Free PDF Download Soap Medical Chart Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. This guide discusses the soap framework (subjective, objective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. The acronym stands. Soap Medical Chart.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For Soap Medical Chart The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The acronym stands for subjective,. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly. Soap Medical Chart.
From musculoskeletalkey.com
Treatment Notes and Progress Notes Using a Modified SOAP Format Soap Medical Chart In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. This guide discusses the soap framework (subjective, objective,. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a standardized method for documenting patient information in healthcare. Documenting a. Soap Medical Chart.
From www.pinterest.com
Soap Note Template Pendidikan, Penyakit, Rumah sakit Soap Medical Chart Exactly what is a soap note?. We’ve also compiled some soap. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. This guide discusses the soap framework (subjective, objective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are. Soap Medical Chart.
From zolmi.com
How To Write Massage Therapy Soap Notes in 2024 Examples Soap Medical Chart This guide discusses the soap framework (subjective, objective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. We’ve also compiled some soap. Soap notes are a standardized method for documenting patient information in healthcare. Documenting a patient assessment in the notes is something all medical students. Soap Medical Chart.
From ar.inspiredpencil.com
Soap Chart Template Soap Medical Chart Soap notes are a standardized method for documenting patient information in healthcare. Exactly what is a soap note?. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soap framework (subjective, objective,. The acronym stands. Soap Medical Chart.
From www.carecloud.com
Free SOAP Notes Template CareCloud Continuum Soap Medical Chart In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The acronym stands for subjective,. We’ve also compiled some soap. Exactly what is a soap note?. Documenting a patient assessment in the notes is something all medical students need to practice. The subjective, objective, assessment and plan (soap) note. Soap Medical Chart.
From www.wildmedcenter.com
Wilderness Medicine Training Center's Patient SOAP Notes Soap Medical Chart The acronym stands for subjective,. Documenting a patient assessment in the notes is something all medical students need to practice. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in. Soap Medical Chart.
From clinicsense.com
Free SOAP Notes Template ClinicSense Soap Medical Chart Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. We’ve also compiled some soap. Documenting a patient assessment in the notes is something all medical students need to practice. The acronym stands for subjective,. Soap—or subjective, objective, assessment and plan—notes allow. Soap Medical Chart.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide Soap Medical Chart Soap notes are a standardized method for documenting patient information in healthcare. Exactly what is a soap note?. We’ve also compiled some soap. Documenting a patient assessment in the notes is something all medical students need to practice. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap. Soap Medical Chart.
From www.theraplatform.com
Occupational therapy SOAP note Soap Medical Chart Exactly what is a soap note?. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The acronym stands for subjective,. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap notes are a standardized method for documenting patient. Soap Medical Chart.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education Soap Medical Chart Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare. Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. We’ve also compiled some soap. Exactly what is a. Soap Medical Chart.
From studylib.net
Patient SOAP Note Charting Procedures Soap Medical Chart The acronym stands for subjective,. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a standardized method for documenting patient information in healthcare.. Soap Medical Chart.