Soap Diagnosis Example . Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soapframework (subjective, objective,. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note. Document measurable and observable data, including physical exam findings, vital signs, and test results. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym:
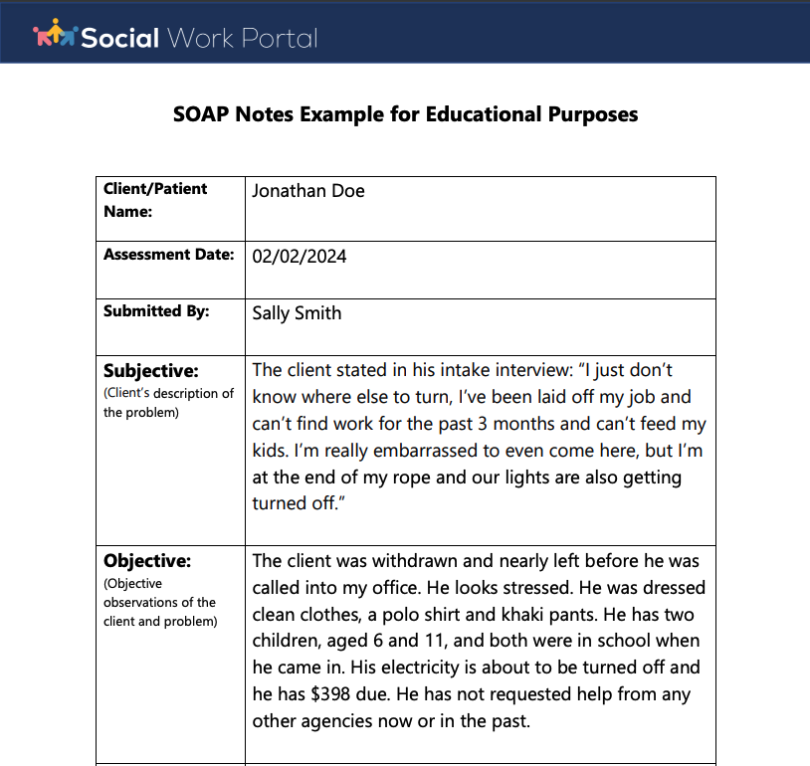
from www.socialworkportal.com
This guide discusses the soapframework (subjective, objective,. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap nursing notes are a type of patient progress note or nurse’s note. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with patients that follows a specific format. Documenting a patient assessment in the notes is something all medical students need to practice. They contain four primary sections, represented by its acronym:
How to Write a Social Work Soap Assessment Best Guide to Soap
Soap Diagnosis Example Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Document measurable and observable data, including physical exam findings, vital signs, and test results. We’ve also compiled some soap. They contain four primary sections, represented by its acronym: This guide discusses the soapframework (subjective, objective,. Soap nursing notes are a type of patient progress note or nurse’s note. Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a specific format for writing progress notes as a behavioral health clinician. It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
From www.scribd.com
Soap note Medical Diagnosis Substance Abuse Soap Diagnosis Example Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. It is the documentation used to record information about encounters with patients that follows a specific format. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. Soap nursing notes are a type. Soap Diagnosis Example.
From www.studocu.com
Heent soap example Soap note © 2019 Walden University Page 1 of 2 Soap Diagnosis Example We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. This guide discusses the soapframework (subjective, objective,. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. They contain four primary sections, represented. Soap Diagnosis Example.
From doctemplates.us
Medical Diagnosis Form Template DocTemplates Soap Diagnosis Example Document measurable and observable data, including physical exam findings, vital signs, and test results. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. In this article, we’ll cover how to write soap. Soap Diagnosis Example.
From www.scribd.com
SOAP Note Directions & Abbreviations Medical Diagnosis Differential Soap Diagnosis Example Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. This guide discusses the soapframework (subjective, objective,. Soap notes are a specific format for writing progress notes as a behavioral health clinician. We’ve. Soap Diagnosis Example.
From www.theraplatform.com
Occupational therapy SOAP note Soap Diagnosis Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. This guide discusses the soapframework (subjective, objective,. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by its acronym: Document measurable and observable data, including physical exam findings, vital signs, and test results. The soap. Soap Diagnosis Example.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education Soap Diagnosis Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. It is the documentation used to record information about encounters with patients that follows a specific format. Document measurable and observable data, including physical exam findings, vital signs, and test results. Soap nursing notes are a type of patient progress note or nurse’s note. The. Soap Diagnosis Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Diagnosis Example They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. This guide discusses the soapframework (subjective, objective,. We’ve also compiled some soap. It is the documentation used to record information about encounters with patients that follows a specific format. Document measurable and observable data, including physical exam findings,. Soap Diagnosis Example.
From www.carepatron.com
SOAP Notes for Chiropractic Template & Example Free PDF Download Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. It is the documentation used to record information about. Soap Diagnosis Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Diagnosis Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: We’ve also compiled some soap. The soap note helps guide healthcare workers use their clinical. Soap Diagnosis Example.
From www.slideshare.net
SOAP Notes Dentistry Example PDF Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. It is the. Soap Diagnosis Example.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Soap Diagnosis Example This guide discusses the soapframework (subjective, objective,. They contain four primary sections, represented by its acronym: We’ve also compiled some soap. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. In this article, we’ll cover how to write soap notes, describing the soap format and what to include. Soap Diagnosis Example.
From www.studocu.com
Comprehensive SOAP Template Comprehensive SOAP Template Patient Soap Diagnosis Example We’ve also compiled some soap. They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. In this article, we’ll cover how to write soap notes, describing the soap format and what to include. Soap Diagnosis Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Diagnosis Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific format for writing progress notes. Soap Diagnosis Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note. The soap note helps guide healthcare workers use their clinical reasoning. Soap Diagnosis Example.
From studylib.net
adult soap note Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. It is. Soap Diagnosis Example.
From www.studocu.com
Wk5 soap soap note about STIs. Includes differential diagnosis Soap Diagnosis Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses. Soap Diagnosis Example.
From studylib.net
Patient SOAP Note Charting Procedures Soap Diagnosis Example They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a. Soap Diagnosis Example.
From www.scribd.com
The SOAP Note Format Medical Record Diseases And Disorders Soap Diagnosis Example Document measurable and observable data, including physical exam findings, vital signs, and test results. It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym: Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soapframework. Soap Diagnosis Example.
From www.studocu.com
Health Assessment Skin Condition SOAP NOTE Differential Diagnosis for Soap Diagnosis Example It is the documentation used to record information about encounters with patients that follows a specific format. This guide discusses the soapframework (subjective, objective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: Documenting a patient assessment in the. Soap Diagnosis Example.
From www.pinterest.fr
soap note examples for nurse practitioners Nursing Documentation Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a way for. Soap Diagnosis Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Diagnosis Example They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. This guide discusses the soapframework (subjective, objective,. Documenting a patient assessment in the notes is something all. Soap Diagnosis Example.
From www.scribd.com
Soap Charting Medical Diagnosis Respiratory Tract Soap Diagnosis Example Document measurable and observable data, including physical exam findings, vital signs, and test results. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. This guide discusses the soapframework (subjective, objective,. The soap note helps guide healthcare workers use. Soap Diagnosis Example.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Soap Diagnosis Example This guide discusses the soapframework (subjective, objective,. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: Document measurable and observable data, including physical exam findings, vital signs, and test results. Documenting a patient assessment in the notes is something. Soap Diagnosis Example.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Diagnosis Example We’ve also compiled some soap. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections,. Soap Diagnosis Example.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Soap Diagnosis Example They contain four primary sections, represented by its acronym: Soap nursing notes are a type of patient progress note or nurse’s note. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. We’ve also compiled some soap. The soap note helps guide healthcare workers use their clinical reasoning to. Soap Diagnosis Example.
From unitedhealthcareinsurancedoctors.blogspot.com
Physical Therapy Soap Note For Stroke Patient United Health Care Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. They contain four primary sections, represented by its acronym: The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. We’ve also compiled some soap. This guide discusses the soapframework (subjective, objective,. Soap notes are. Soap Diagnosis Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Diagnosis Example Soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients that follows a specific format. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Documenting a patient assessment in the notes is something. Soap Diagnosis Example.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners, Physician Soap Diagnosis Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Soap nursing notes are a type of patient progress note or nurse’s note. Documenting a patient assessment in the notes is something all medical students need to practice. The soap note helps guide healthcare workers use their clinical reasoning. Soap Diagnosis Example.
From knowmedge.com
Medical Mnemonics Diagnostic Criteria for SLE Soap Brain MD USMLE Soap Diagnosis Example In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. Document measurable and observable data, including physical exam findings, vital signs, and test results. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. It is the documentation. Soap Diagnosis Example.
From tukioka-clinic.com
😎 Comprehensive soap note example. Womens Health SOAP note. 20190117 Soap Diagnosis Example Documenting a patient assessment in the notes is something all medical students need to practice. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. We’ve also compiled some soap. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in. Soap Diagnosis Example.
From kelitbanganwonogiri.org
Soap Assessment Template Soap Diagnosis Example This guide discusses the soapframework (subjective, objective,. We’ve also compiled some soap. Document measurable and observable data, including physical exam findings, vital signs, and test results. The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. They contain four primary sections, represented by its acronym: Documenting a patient assessment. Soap Diagnosis Example.
From www.slideserve.com
PPT Patient Medical Records PowerPoint Presentation, free download Soap Diagnosis Example They contain four primary sections, represented by its acronym: The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. We’ve also compiled some soap. Document measurable and observable data, including physical exam findings, vital signs, and test results. Soap notes are a specific format for writing progress notes as. Soap Diagnosis Example.
From www.studocu.com
Sample+SOAP+1Right+shoulder+pain Patient Name Stephen Smith DOB 1 Soap Diagnosis Example Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In this article, we’ll cover how to write soap notes, describing the soap format and what to include in each section. They contain four primary sections, represented by its acronym: Document measurable and observable data, including physical exam findings, vital signs, and test results.. Soap Diagnosis Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Diagnosis Example The soap note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. This guide discusses the soapframework (subjective, objective,. In this article, we’ll cover how to write soap notes, describing the soap format and what. Soap Diagnosis Example.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Diagnosis Example It is the documentation used to record information about encounters with patients that follows a specific format. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Document measurable and observable data, including physical exam findings, vital signs, and test results. The soap note helps guide healthcare workers use their clinical reasoning to assess,. Soap Diagnosis Example.