Aetna Better Health Of Va Claim Reconsideration Form . Learn about the timeframe for appeals and reconsiderations. You may disagree with a claim or utilization review decision. You or the member’s designated representative can file on their behalf with their written consent. Please fill out the form to get authorization for services. Just complete the authorization release for. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Discover how to submit a dispute. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. To help aetna review and respond to your request, please provide the following information. You have 60 days from. Click on the appropriate button below to find your correct form. (this information may be found on correspondence.
from www.formsbank.com
(this information may be found on correspondence. Just complete the authorization release for. Learn about the timeframe for appeals and reconsiderations. To help aetna review and respond to your request, please provide the following information. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Click on the appropriate button below to find your correct form. You or the member’s designated representative can file on their behalf with their written consent. You may disagree with a claim or utilization review decision. Discover how to submit a dispute. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a.
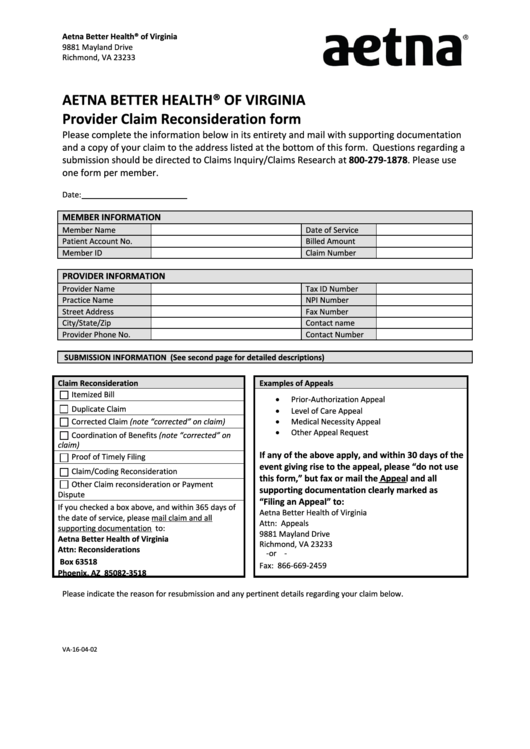
Virginia Provider Claim Reconsideration Form printable pdf download
Aetna Better Health Of Va Claim Reconsideration Form Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Discover how to submit a dispute. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Learn about the timeframe for appeals and reconsiderations. To help aetna review and respond to your request, please provide the following information. (this information may be found on correspondence. You have 60 days from. You or the member’s designated representative can file on their behalf with their written consent. You may disagree with a claim or utilization review decision. Click on the appropriate button below to find your correct form. Please fill out the form to get authorization for services. Just complete the authorization release for.
From fill.io
Fill Free fillable Aetna Better Health PDF forms Aetna Better Health Of Va Claim Reconsideration Form Click on the appropriate button below to find your correct form. Discover how to submit a dispute. Just complete the authorization release for. Learn about the timeframe for appeals and reconsiderations. To help aetna review and respond to your request, please provide the following information. You have 60 days from. You may disagree with a claim or utilization review decision.. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Aetna Reconsideration Form Complete with ease airSlate SignNow Aetna Better Health Of Va Claim Reconsideration Form (this information may be found on correspondence. You have 60 days from. Please fill out the form to get authorization for services. Click on the appropriate button below to find your correct form. Discover how to submit a dispute. To help aetna review and respond to your request, please provide the following information. Use this provider claim appeal form for. Aetna Better Health Of Va Claim Reconsideration Form.
From www.formsbank.com
Top 84 Aetna Forms And Templates free to download in PDF format Aetna Better Health Of Va Claim Reconsideration Form You may disagree with a claim or utilization review decision. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Please fill out the form to get authorization for services. Discover how to submit a dispute. You or the member’s designated representative can file on their behalf. Aetna Better Health Of Va Claim Reconsideration Form.
From fill.io
Fill Free fillable Aetna Better Health PDF forms Aetna Better Health Of Va Claim Reconsideration Form Just complete the authorization release for. Learn about the timeframe for appeals and reconsiderations. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Please fill out the form to get authorization for services. Discover how to submit a dispute. Click on the appropriate button below to find your correct form. You or the member’s designated representative. Aetna Better Health Of Va Claim Reconsideration Form.
From www.uslegalforms.com
Aetna Better Health Prior Authorization Fill and Sign Printable Aetna Better Health Of Va Claim Reconsideration Form Please fill out the form to get authorization for services. Just complete the authorization release for. To help aetna review and respond to your request, please provide the following information. Learn about the timeframe for appeals and reconsiderations. You or the member’s designated representative can file on their behalf with their written consent. Discover how to submit a dispute. You. Aetna Better Health Of Va Claim Reconsideration Form.
From eforms.com
Free Aetna Prior (Rx) Authorization Form PDF eForms Aetna Better Health Of Va Claim Reconsideration Form To help aetna review and respond to your request, please provide the following information. Learn about the timeframe for appeals and reconsiderations. You may disagree with a claim or utilization review decision. You have 60 days from. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Please fill out the form to get authorization for services.. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Uhc Reconsideration 20122024 Form Fill Out and Sign Printable PDF Aetna Better Health Of Va Claim Reconsideration Form Discover how to submit a dispute. Just complete the authorization release for. You may disagree with a claim or utilization review decision. (this information may be found on correspondence. You have 60 days from. You or the member’s designated representative can file on their behalf with their written consent. Use this provider claim appeal form for provider claim appeals concerning. Aetna Better Health Of Va Claim Reconsideration Form.
From www.formsbank.com
Form Ne140667 Aetna Provider Claim Resubmission/reconsideration Aetna Better Health Of Va Claim Reconsideration Form (this information may be found on correspondence. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. You have 60 days from. You or the member’s designated representative can file on their behalf with. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online Aetna Better Health Authorization Tool Fax Email Print Aetna Better Health Of Va Claim Reconsideration Form To help aetna review and respond to your request, please provide the following information. Please fill out the form to get authorization for services. Click on the appropriate button below to find your correct form. (this information may be found on correspondence. You or the member’s designated representative can file on their behalf with their written consent. You have 60. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Aetna Reimbursement Form Fill Out and Sign Printable PDF Template Aetna Better Health Of Va Claim Reconsideration Form Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Discover how to submit a dispute. To help aetna review and respond to your request, please provide the following information. You have 60 days from. (this information may be found on correspondence. You may disagree with a claim or utilization review decision. Learn about the timeframe for. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online Word b2010b document template for Aetna Better bHealthb Aetna Better Health Of Va Claim Reconsideration Form Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Just complete the authorization release for. Please fill out the form to get authorization for services. Click on the appropriate button below to find your correct form. Discover how to submit a dispute. You or the member’s designated representative can file on their behalf with their written. Aetna Better Health Of Va Claim Reconsideration Form.
From www.formsbank.com
Fillable Missouri Provider Claim Reconsideration Form printable pdf Aetna Better Health Of Va Claim Reconsideration Form To help aetna review and respond to your request, please provide the following information. You have 60 days from. Just complete the authorization release for. Click on the appropriate button below to find your correct form. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Use this provider claim appeal form for provider claim appeals concerning. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Aetna Phi 20192024 Form Fill Out and Sign Printable PDF Template Aetna Better Health Of Va Claim Reconsideration Form You have 60 days from. Learn about the timeframe for appeals and reconsiderations. Just complete the authorization release for. To help aetna review and respond to your request, please provide the following information. Please fill out the form to get authorization for services. Click on the appropriate button below to find your correct form. Use this provider claim appeal form. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online AETNA BETTER HEALTH OF FLORIDA Claims Adjustment Aetna Better Health Of Va Claim Reconsideration Form Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Learn about the timeframe for appeals and reconsiderations. You may disagree with a claim or utilization review decision. To help aetna review and respond to your request, please provide the following information. Formal reviews of claims reimbursements. Aetna Better Health Of Va Claim Reconsideration Form.
From fill.io
Fill Free fillable Aetna Better Health PDF forms Aetna Better Health Of Va Claim Reconsideration Form You may disagree with a claim or utilization review decision. Click on the appropriate button below to find your correct form. You have 60 days from. Please fill out the form to get authorization for services. To help aetna review and respond to your request, please provide the following information. Formal reviews of claims reimbursements or coding decisions, or claims. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Aetna Reconsideration 20122024 Form Fill Out and Sign Printable PDF Aetna Better Health Of Va Claim Reconsideration Form You may disagree with a claim or utilization review decision. To help aetna review and respond to your request, please provide the following information. Please fill out the form to get authorization for services. (this information may be found on correspondence. Learn about the timeframe for appeals and reconsiderations. Use this provider claim appeal form for provider claim appeals concerning. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online Claims Reconsideration Form New Address Aetna Aetna Better Health Of Va Claim Reconsideration Form You or the member’s designated representative can file on their behalf with their written consent. Please fill out the form to get authorization for services. Learn about the timeframe for appeals and reconsiderations. Click on the appropriate button below to find your correct form. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment. Aetna Better Health Of Va Claim Reconsideration Form.
From www.templateroller.com
Form VA160402 Fill Out, Sign Online and Download Printable PDF Aetna Better Health Of Va Claim Reconsideration Form (this information may be found on correspondence. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Discover how to submit a dispute. Please fill out the form to get authorization for services. Learn about the timeframe for appeals and reconsiderations. You or the member’s designated representative. Aetna Better Health Of Va Claim Reconsideration Form.
From aetna-pharmacy-prior-authorization-form.pdffiller.com
Aetna Medicare Prior Authorization Form Fill Online, Printable Aetna Better Health Of Va Claim Reconsideration Form Learn about the timeframe for appeals and reconsiderations. (this information may be found on correspondence. Click on the appropriate button below to find your correct form. Please fill out the form to get authorization for services. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. You have 60 days from. Use this provider claim appeal form. Aetna Better Health Of Va Claim Reconsideration Form.
From fill.io
Fill Free fillable AETNA BETTER HEALTH OF VIRGINIA (128VA) ERA Aetna Better Health Of Va Claim Reconsideration Form Click on the appropriate button below to find your correct form. Discover how to submit a dispute. You have 60 days from. Please fill out the form to get authorization for services. Learn about the timeframe for appeals and reconsiderations. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Just complete the authorization release for. You. Aetna Better Health Of Va Claim Reconsideration Form.
From www.formsbank.com
Form La151106 Aetna Better Health Form printable pdf download Aetna Better Health Of Va Claim Reconsideration Form Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. You have 60 days from. Just complete the authorization release for. To help aetna review and respond to your request, please provide the following information. You or the member’s designated representative can file on their behalf with. Aetna Better Health Of Va Claim Reconsideration Form.
From magqqueenie.pages.dev
Aetna Reconsideration Form 2024 Catlee Alvinia Aetna Better Health Of Va Claim Reconsideration Form To help aetna review and respond to your request, please provide the following information. Learn about the timeframe for appeals and reconsiderations. Please fill out the form to get authorization for services. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Formal reviews of claims reimbursements. Aetna Better Health Of Va Claim Reconsideration Form.
From pdfprof.com
aetna claim forms Aetna Better Health Of Va Claim Reconsideration Form Please fill out the form to get authorization for services. You may disagree with a claim or utilization review decision. You or the member’s designated representative can file on their behalf with their written consent. Just complete the authorization release for. Discover how to submit a dispute. (this information may be found on correspondence. Formal reviews of claims reimbursements or. Aetna Better Health Of Va Claim Reconsideration Form.
From www.formsbank.com
Virginia Provider Claim Reconsideration Form printable pdf download Aetna Better Health Of Va Claim Reconsideration Form To help aetna review and respond to your request, please provide the following information. Just complete the authorization release for. (this information may be found on correspondence. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. Learn about the timeframe for appeals and reconsiderations. Please fill. Aetna Better Health Of Va Claim Reconsideration Form.
From www.aetnabetterhealth.com
Find a Provider Aetna Medicaid Illinois Aetna Better Health Of Va Claim Reconsideration Form Click on the appropriate button below to find your correct form. Learn about the timeframe for appeals and reconsiderations. Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. (this information may be found on correspondence. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online Aetna better health reconsideration form va. Aetna Aetna Better Health Of Va Claim Reconsideration Form Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Just complete the authorization release for. You have 60 days from. To help aetna review and respond to your request, please provide the following information. Discover how to submit a dispute. (this information may be found on correspondence. Click on the appropriate button below to find your. Aetna Better Health Of Va Claim Reconsideration Form.
From www.uslegalforms.com
Get VA Reconsideration of Value Request Requirements US Legal Forms Aetna Better Health Of Va Claim Reconsideration Form Click on the appropriate button below to find your correct form. Learn about the timeframe for appeals and reconsiderations. You have 60 days from. (this information may be found on correspondence. You may disagree with a claim or utilization review decision. Just complete the authorization release for. Please fill out the form to get authorization for services. Use this provider. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Aetna Claim Form Complete with ease airSlate SignNow Aetna Better Health Of Va Claim Reconsideration Form To help aetna review and respond to your request, please provide the following information. You have 60 days from. Click on the appropriate button below to find your correct form. (this information may be found on correspondence. You or the member’s designated representative can file on their behalf with their written consent. Just complete the authorization release for. Please fill. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online aetna better health of west virginia prior Aetna Better Health Of Va Claim Reconsideration Form You may disagree with a claim or utilization review decision. Just complete the authorization release for. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. (this information may be found on correspondence. Discover how to submit a dispute. Please fill out the form to get authorization. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
20192022 Form Aetna GR67902 Fill Online, Printable, Fillable, Blank Aetna Better Health Of Va Claim Reconsideration Form Click on the appropriate button below to find your correct form. You or the member’s designated representative can file on their behalf with their written consent. Discover how to submit a dispute. Just complete the authorization release for. Please fill out the form to get authorization for services. Formal reviews of claims reimbursements or coding decisions, or claims that require. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
Fillable Online FINAL Prenatal Risk Assessment Form Aetna Better Aetna Better Health Of Va Claim Reconsideration Form You or the member’s designated representative can file on their behalf with their written consent. You have 60 days from. You may disagree with a claim or utilization review decision. To help aetna review and respond to your request, please provide the following information. (this information may be found on correspondence. Use this provider claim appeal form for provider claim. Aetna Better Health Of Va Claim Reconsideration Form.
From www.signnow.com
Claims for Reconsideration U S Department of Veterans Claims for Aetna Better Health Of Va Claim Reconsideration Form Learn about the timeframe for appeals and reconsiderations. You have 60 days from. You may disagree with a claim or utilization review decision. You or the member’s designated representative can file on their behalf with their written consent. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to. Aetna Better Health Of Va Claim Reconsideration Form.
From www.pdffiller.com
20182024 Form Aetna GR68192 Fill Online, Printable, Fillable, Blank Aetna Better Health Of Va Claim Reconsideration Form (this information may be found on correspondence. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. To help aetna review and respond to your request, please provide the following information. Click on the appropriate button below to find your correct form. Discover how to submit a. Aetna Better Health Of Va Claim Reconsideration Form.
From www.formsbank.com
Aetna Better Health Form Of New Jersey printable pdf download Aetna Better Health Of Va Claim Reconsideration Form Formal reviews of claims reimbursements or coding decisions, or claims that require reprocessing. Click on the appropriate button below to find your correct form. To help aetna review and respond to your request, please provide the following information. You or the member’s designated representative can file on their behalf with their written consent. Just complete the authorization release for. Discover. Aetna Better Health Of Va Claim Reconsideration Form.
From www.vrogue.co
Aetna Claim Forms Fill Out And Sign Printable Pdf Tem vrogue.co Aetna Better Health Of Va Claim Reconsideration Form Just complete the authorization release for. To help aetna review and respond to your request, please provide the following information. You or the member’s designated representative can file on their behalf with their written consent. Use this provider claim appeal form for provider claim appeals concerning claim denials and claim payment amounts that are not related to a. (this information. Aetna Better Health Of Va Claim Reconsideration Form.