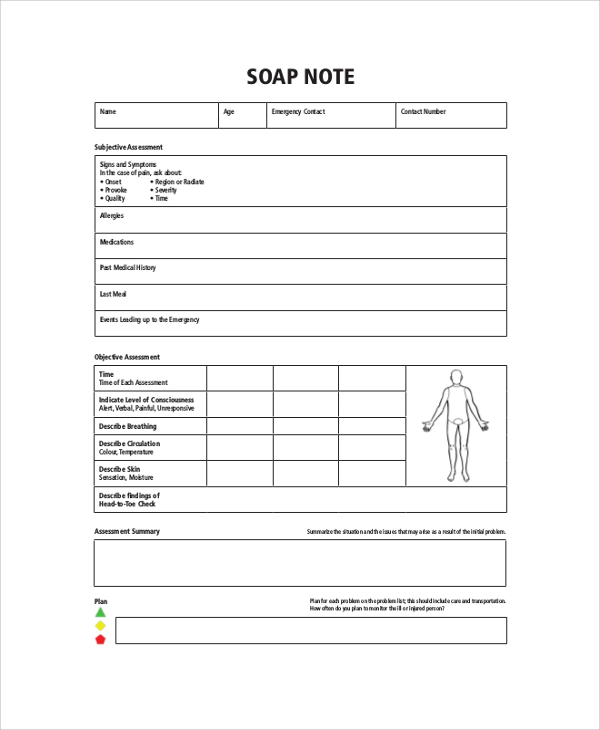
History And Physical Soap Note . The soap note is an update on an existing problem as in a post op visit or follow up of a problem. How do doctors organize all the information about their patients? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. It is an important reference document that provides concise information. Documenting a patient assessment in the notes is something all medical students need to practice. The written history and physical (h&p) serves several purposes: Back in the 1950s, lawrence weed asked himself the same. Surgical history with dates, indications and types of operations. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. This format is used in.
from templates.rjuuc.edu.np
How do doctors organize all the information about their patients? In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. Documenting a patient assessment in the notes is something all medical students need to practice. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. It is an important reference document that provides concise information. Surgical history with dates, indications and types of operations. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. This format is used in. The written history and physical (h&p) serves several purposes:
Physical Therapy Soap Note Template
History And Physical Soap Note It is an important reference document that provides concise information. Documenting a patient assessment in the notes is something all medical students need to practice. How do doctors organize all the information about their patients? In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. This format is used in. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. The written history and physical (h&p) serves several purposes: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. Surgical history with dates, indications and types of operations. Back in the 1950s, lawrence weed asked himself the same. It is an important reference document that provides concise information.
From www.studocu.com
“Sore Throat” SOAP NOTE Chief complaint “Sore Throat” History of History And Physical Soap Note This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. Back in the 1950s, lawrence weed asked himself the same. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. The soap note is an. History And Physical Soap Note.
From www.etsy.com
History and Physical SOAP Note Template, Comprehensive Physical History And Physical Soap Note Surgical history with dates, indications and types of operations. How do doctors organize all the information about their patients? In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. The written history and physical (h&p) serves several purposes: This format is used in. It is an important reference. History And Physical Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab History And Physical Soap Note This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. Surgical history with dates, indications and types of operations. It is an important reference document. History And Physical Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab History And Physical Soap Note It is an important reference document that provides concise information. Back in the 1950s, lawrence weed asked himself the same. This format is used in. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. How do doctors organize all the information about their patients? In modern. History And Physical Soap Note.
From printabletemplate.concejomunicipaldechinu.gov.co
Soap Note Template Physical Therapy History And Physical Soap Note The written history and physical (h&p) serves several purposes: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. How do doctors organize all the information about their. History And Physical Soap Note.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF History And Physical Soap Note It is an important reference document that provides concise information. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. Surgical history with dates, indications and types of operations. This format is used in. How do doctors organize all the information about their patients? The written history and. History And Physical Soap Note.
From www.etsy.com
SOAP Note Template History and Physical PDF and Word Document Etsy History And Physical Soap Note In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. Back in the 1950s, lawrence weed asked himself the same. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. Documenting a patient assessment in. History And Physical Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab History And Physical Soap Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Back in the 1950s, lawrence weed asked himself the same. The written history and physical (h&p) serves several purposes: This format is used in. Surgical history with dates, indications and types of operations. It is an important reference document that provides. History And Physical Soap Note.
From studylib.net
Patient SOAP Note Charting Procedures History And Physical Soap Note How do doctors organize all the information about their patients? The written history and physical (h&p) serves several purposes: This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. It is an important reference document that provides concise information. The subjective, objective, assessment and plan (soap) note. History And Physical Soap Note.
From templates.rjuuc.edu.np
Physical Therapy Soap Note Template History And Physical Soap Note It is an important reference document that provides concise information. Surgical history with dates, indications and types of operations. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a. History And Physical Soap Note.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide History And Physical Soap Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This format is used in. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. Surgical history with dates, indications and types of operations. The soap note is. History And Physical Soap Note.
From www.typecalendar.com
Free Printable SOAP Note Templates [PDF, Word] History And Physical Soap Note The written history and physical (h&p) serves several purposes: How do doctors organize all the information about their patients? Back in the 1950s, lawrence weed asked himself the same. Documenting a patient assessment in the notes is something all medical students need to practice. It is an important reference document that provides concise information. This format is used in. This. History And Physical Soap Note.
From www.etsy.com
History and Physical SOAP Note Template, Comprehensive Physical History And Physical Soap Note It is an important reference document that provides concise information. Surgical history with dates, indications and types of operations. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. Back in the 1950s, lawrence weed asked himself the same. This guide discusses the soap framework (subjective, objective, assessment, plan), which should. History And Physical Soap Note.
From www.etsy.com
SOAP Note Template History and Physical PDF and Word Document Etsy History And Physical Soap Note This format is used in. The written history and physical (h&p) serves several purposes: Back in the 1950s, lawrence weed asked himself the same. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely. History And Physical Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab History And Physical Soap Note The written history and physical (h&p) serves several purposes: It is an important reference document that provides concise information. Back in the 1950s, lawrence weed asked himself the same. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. In modern clinical practice, doctors share medical information primarily. History And Physical Soap Note.
From www.etsy.com
History and Physical SOAP Note Template, Comprehensive Physical History And Physical Soap Note It is an important reference document that provides concise information. This format is used in. How do doctors organize all the information about their patients? The soap note is an update on an existing problem as in a post op visit or follow up of a problem. Documenting a patient assessment in the notes is something all medical students need. History And Physical Soap Note.
From aruba.desertcart.com
Buy Progress & H&P + 4 Day SOAP Progress Note + Medical History and History And Physical Soap Note How do doctors organize all the information about their patients? This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. The written history and physical. History And Physical Soap Note.
From www.studocu.com
Sample H&P and SOAP note History & Physical (admission note) CC History And Physical Soap Note Documenting a patient assessment in the notes is something all medical students need to practice. How do doctors organize all the information about their patients? The soap note is an update on an existing problem as in a post op visit or follow up of a problem. The subjective, objective, assessment and plan (soap) note is an acronym representing a. History And Physical Soap Note.
From www.carepatron.com
SOAP Notes For Physical Therapy Template & Example Free PDF Download History And Physical Soap Note This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. Documenting a patient assessment in the notes is something all medical students need to practice.. History And Physical Soap Note.
From www.studypool.com
SOLUTION Newborn soap note Studypool History And Physical Soap Note How do doctors organize all the information about their patients? This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. Documenting a patient assessment in the notes is something all medical students need to practice. The soap note is an update on an existing problem as in. History And Physical Soap Note.
From www.template.net
11+ Soap Note Templates Free Sample, Example, Format Download! History And Physical Soap Note Documenting a patient assessment in the notes is something all medical students need to practice. Surgical history with dates, indications and types of operations. The written history and physical (h&p) serves several purposes: The soap note is an update on an existing problem as in a post op visit or follow up of a problem. How do doctors organize all. History And Physical Soap Note.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF History And Physical Soap Note How do doctors organize all the information about their patients? Surgical history with dates, indications and types of operations. Back in the 1950s, lawrence weed asked himself the same. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. This guide discusses the soap framework (subjective, objective, assessment,. History And Physical Soap Note.
From www.studypool.com
SOLUTION Newborn soap note Studypool History And Physical Soap Note Documenting a patient assessment in the notes is something all medical students need to practice. How do doctors organize all the information about their patients? This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. It is an important reference document that provides concise information. Surgical history. History And Physical Soap Note.
From www.studocu.com
Mixed Soapnote SOAP Note SOAP Note Form S/ Identifying Information History And Physical Soap Note The soap note is an update on an existing problem as in a post op visit or follow up of a problem. It is an important reference document that provides concise information. Surgical history with dates, indications and types of operations. Back in the 1950s, lawrence weed asked himself the same. Documenting a patient assessment in the notes is something. History And Physical Soap Note.
From www.etsy.com
History and Physical SOAP Note Template, Comprehensive Physical History And Physical Soap Note In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a. History And Physical Soap Note.
From studylib.net
Daily Progress Notes (The “SOAP” note) History And Physical Soap Note It is an important reference document that provides concise information. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. How do doctors organize all the information about their patients? The soap note is an update on an existing problem as in a post op visit or follow up of a. History And Physical Soap Note.
From www.etsy.com
History and Physical SOAP Note Format for Medical Students, Residents History And Physical Soap Note This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. Surgical history with dates, indications and types of operations. The written history and physical (h&p) serves several purposes: How do doctors organize all the information about their patients? It is an important reference document that provides concise. History And Physical Soap Note.
From www.studocu.com
Labour and delivery Soap Note Word Free Download Sample L&D Admit History And Physical Soap Note How do doctors organize all the information about their patients? The soap note is an update on an existing problem as in a post op visit or follow up of a problem. The written history and physical (h&p) serves several purposes: It is an important reference document that provides concise information. This guide discusses the soap framework (subjective, objective, assessment,. History And Physical Soap Note.
From safetyculture.com
Free Physical Therapy SOAP Note PDF SafetyCulture History And Physical Soap Note How do doctors organize all the information about their patients? The soap note is an update on an existing problem as in a post op visit or follow up of a problem. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. The subjective, objective, assessment and. History And Physical Soap Note.
From healthcareproxymaryland.blogspot.com
Soap Note Physical Therapy Sample History And Physical Soap Note This format is used in. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. It is an important reference document that provides concise information. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. Documenting. History And Physical Soap Note.
From www.etsy.com
History and Physical SOAP Note Template, Comprehensive Physical History And Physical Soap Note Documenting a patient assessment in the notes is something all medical students need to practice. Surgical history with dates, indications and types of operations. The soap note is an update on an existing problem as in a post op visit or follow up of a problem. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely. History And Physical Soap Note.
From www.sampletemplates.com
FREE 15+ SOAP Note Templates in PDF MS Word History And Physical Soap Note Surgical history with dates, indications and types of operations. How do doctors organize all the information about their patients? It is an important reference document that provides concise information. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. The soap note is an update on an existing. History And Physical Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab History And Physical Soap Note The soap note is an update on an existing problem as in a post op visit or follow up of a problem. Back in the 1950s, lawrence weed asked himself the same. In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. This format is used in. This. History And Physical Soap Note.
From writeness-training.blogspot.com
Soap Note Physical Exam Example History And Physical Soap Note In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and soap. The written history and physical (h&p) serves several purposes: Back in the 1950s, lawrence weed asked himself the same. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a. History And Physical Soap Note.
From orlandoeveryday.com
Dermatology Soap Note Template A Comprehensive Guide For Medical History And Physical Soap Note This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. It is an important reference document that provides concise information. How do doctors organize all the information about their patients? Documenting a patient assessment in the notes is something all medical students need to practice. In modern. History And Physical Soap Note.