History And Physical Form Example . Sample pediatric history and physical exam. The history was obtained from both the patient’s. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The patient’s history and physical that either support or refute the diagnosis. Nausea and vomiting x 1 day. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Lower abdominal pain x 2 days. Explore the essential guide to the history. For each item on your differential, explain what. Date and time of h&p: “i got lightheadedness and felt. Surgical/procedural indications and present illness:
from pray.gelorailmu.com
“i got lightheadedness and felt. Sample pediatric history and physical exam. For each item on your differential, explain what. Explore the essential guide to the history. Surgical/procedural indications and present illness: Date and time of h&p: Nausea and vomiting x 1 day. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Lower abdominal pain x 2 days. The patient’s history and physical that either support or refute the diagnosis.
Free 5+ Work Physical Forms In Pdf in History And Physical Template
History And Physical Form Example “i got lightheadedness and felt. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Date and time of h&p: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. For each item on your differential, explain what. Sample pediatric history and physical exam. Lower abdominal pain x 2 days. The patient’s history and physical that either support or refute the diagnosis. “i got lightheadedness and felt. Nausea and vomiting x 1 day. Surgical/procedural indications and present illness: Explore the essential guide to the history. The history was obtained from both the patient’s.
From www.formsbank.com
PreOp History And Physical Form Montgomery Surgery Center printable History And Physical Form Example Lower abdominal pain x 2 days. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: For each item on your differential, explain what. Sample pediatric history and physical exam. Nausea and vomiting x 1 day. Surgical/procedural indications and present illness: Date and time of h&p: “i got lightheadedness and felt. The patient’s history and physical that. History And Physical Form Example.
From www.formsbank.com
Medical History And Physical Examination Form printable pdf download History And Physical Form Example Sample pediatric history and physical exam. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Nausea and vomiting x 1 day. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Lower abdominal pain x 2 days. Date and time of h&p: The history was obtained from. History And Physical Form Example.
From www.sampletemplatess.com
History And Physical Form Template SampleTemplatess SampleTemplatess History And Physical Form Example Sample pediatric history and physical exam. The patient’s history and physical that either support or refute the diagnosis. Date and time of h&p: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Nausea and vomiting x 1 day. Explore the essential guide to the history. For each item on your differential, explain what. It includes patient. History And Physical Form Example.
From enterstarcrypticcity.blogspot.com
History And Physical Form Template PDF Template History And Physical Form Example Date and time of h&p: For each item on your differential, explain what. Lower abdominal pain x 2 days. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The history was obtained from both the patient’s. Explore the essential guide to the history. Surgical/procedural indications and present illness: The patient’s. History And Physical Form Example.
From pray.gelorailmu.com
Free 5+ Work Physical Forms In Pdf in History And Physical Template History And Physical Form Example Surgical/procedural indications and present illness: Date and time of h&p: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. “i got lightheadedness and felt. Lower abdominal pain x 2 days. The patient’s history and physical that either. History And Physical Form Example.
From old.sermitsiaq.ag
History And Physical Template History And Physical Form Example The patient’s history and physical that either support or refute the diagnosis. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Nausea and vomiting x 1 day. Lower abdominal pain x 2 days. Date and time of h&p: “i got lightheadedness and felt. For each item on your differential, explain. History And Physical Form Example.
From www.pdffiller.com
Physical And History Template Fill Online, Printable, Fillable, Blank History And Physical Form Example It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The patient’s history and physical that either support or refute the diagnosis. Lower abdominal pain x 2 days. Surgical/procedural indications and present illness: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The history was obtained from. History And Physical Form Example.
From www.formsbank.com
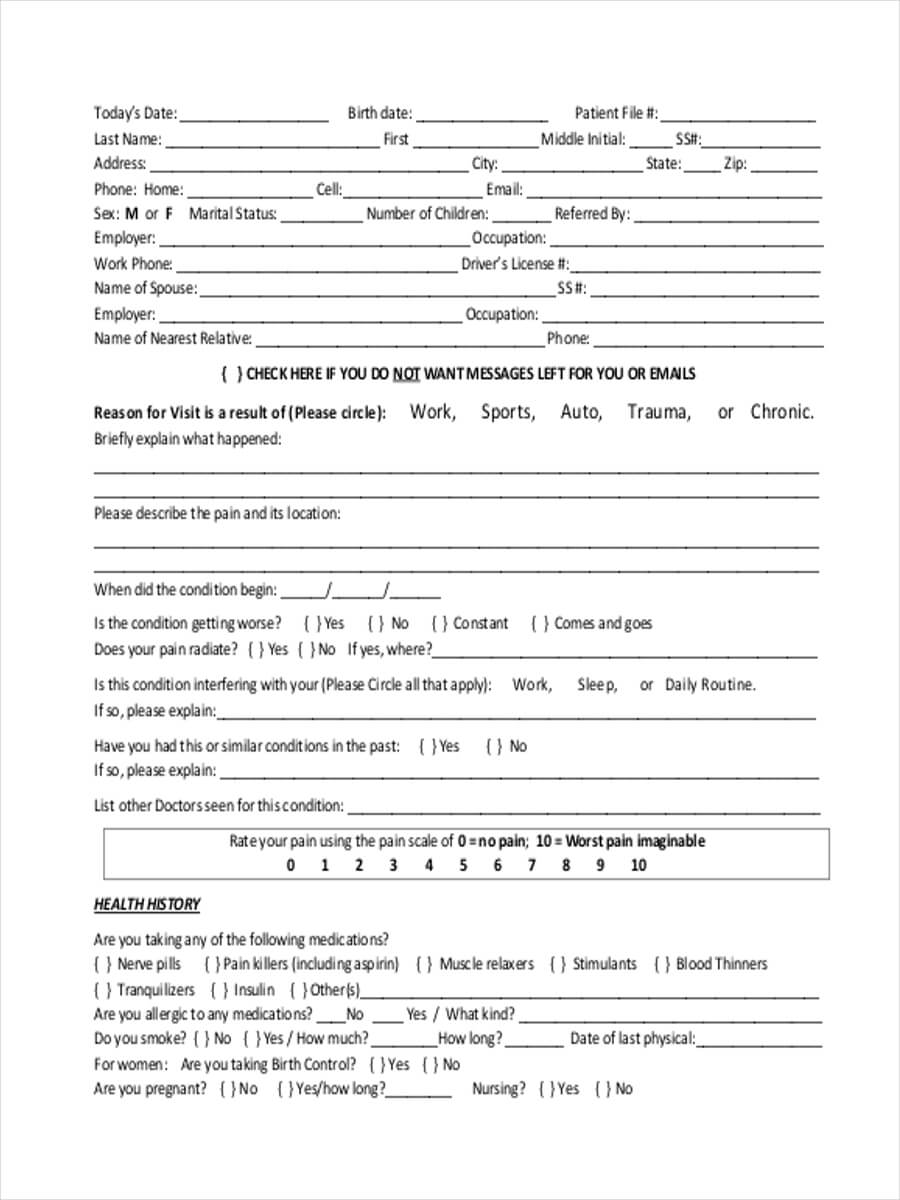
Patient History And Physical Form printable pdf download History And Physical Form Example Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The patient’s history and physical that either support or refute the diagnosis. For each item on your differential, explain what. Nausea and vomiting x 1 day. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. “i got. History And Physical Form Example.
From www.signnow.com
History and Physical Template Edit & Share airSlate SignNow History And Physical Form Example Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The patient’s history and physical that either support or refute the diagnosis. Sample pediatric history and physical exam. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The history was obtained from both the patient’s. Nausea and. History And Physical Form Example.
From sarseh.com
History And Physical Template Word History And Physical Form Example It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The patient’s history and physical that either support or refute the diagnosis. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: “i got lightheadedness and felt. The history was obtained from both the patient’s. Explore the essential. History And Physical Form Example.
From www.dexform.com
Sample medical/physical history report form in Word and Pdf formats History And Physical Form Example Sample pediatric history and physical exam. The history was obtained from both the patient’s. Surgical/procedural indications and present illness: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Date and time of h&p: Lower abdominal pain x 2 days. Comprehensive adult history and physical (sample summative h&p by m2 student). History And Physical Form Example.
From templates.udlvirtual.edu.pe
Free Printable History And Physical Template Printable Templates History And Physical Form Example Nausea and vomiting x 1 day. For each item on your differential, explain what. Date and time of h&p: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The history was obtained from both the patient’s. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: “i. History And Physical Form Example.
From www.sampleforms.com
FREE 10+ Generic PreEmployment Physical Forms in PDF History And Physical Form Example Sample pediatric history and physical exam. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The history was obtained from both the patient’s. The patient’s history and physical that either support or refute the diagnosis. Explore the essential guide to the history. Date and time of h&p: Nausea and vomiting. History And Physical Form Example.
From pray.gelorailmu.com
Free 5+ Sample Employee Physical Forms In Ms Word Pdf for History And History And Physical Form Example Lower abdominal pain x 2 days. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The history was obtained from both the patient’s. Explore the essential guide to the history. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. For each item on your differential, explain. History And Physical Form Example.
From www.signnow.com
Printable History and Physical Template PDF airSlate SignNow History And Physical Form Example Nausea and vomiting x 1 day. “i got lightheadedness and felt. For each item on your differential, explain what. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The history was obtained from both the patient’s. Sample pediatric history and physical exam. Lower abdominal pain x 2 days. Surgical/procedural indications and present illness: Date and time. History And Physical Form Example.
From mungfali.com
Printable Medical History And Physical Form History And Physical Form Example Date and time of h&p: The history was obtained from both the patient’s. Nausea and vomiting x 1 day. The patient’s history and physical that either support or refute the diagnosis. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Comprehensive adult history and physical (sample summative h&p by m2. History And Physical Form Example.
From templatelab.com
43 Medical Health History Forms [PDF, Word] ᐅ TemplateLab History And Physical Form Example Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: For each item on your differential, explain what. Explore the essential guide to the history. Sample pediatric history and physical exam. Surgical/procedural indications and present illness: The history was obtained from both the patient’s. Date and time of h&p: Lower abdominal pain x 2 days. “i got. History And Physical Form Example.
From www.uslegalforms.com
Adult History & Annual Physical Form Fill and Sign Printable Template History And Physical Form Example The patient’s history and physical that either support or refute the diagnosis. Nausea and vomiting x 1 day. Surgical/procedural indications and present illness: “i got lightheadedness and felt. Date and time of h&p: Sample pediatric history and physical exam. Explore the essential guide to the history. It includes patient demographics, medical, family, and social history, a review of systems, and. History And Physical Form Example.
From www.uslegalforms.com
Farese Physical Therapy Patient Medical History Form Fill and Sign History And Physical Form Example Nausea and vomiting x 1 day. Explore the essential guide to the history. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Sample pediatric history and physical exam. Surgical/procedural indications and present illness: The history was obtained from both the patient’s. For each item on your differential, explain what. The patient’s history and physical that either. History And Physical Form Example.
From www.formsbank.com
Physical Examination And Medical History Form printable pdf download History And Physical Form Example Surgical/procedural indications and present illness: Explore the essential guide to the history. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The patient’s history and physical that either support or refute the diagnosis. Sample pediatric history and physical exam. Date and time of h&p: Nausea and vomiting x 1 day. It includes patient demographics, medical, family,. History And Physical Form Example.
From my.fivestarsports.com
Medical History/Physical Form History And Physical Form Example Surgical/procedural indications and present illness: The patient’s history and physical that either support or refute the diagnosis. Date and time of h&p: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: For each item on your differential, explain what. Explore the essential guide to the history. The history was obtained from both the patient’s. It includes. History And Physical Form Example.
From www.etsy.com
History & Physical Exam Template Printable and Editable Versions Etsy History And Physical Form Example Lower abdominal pain x 2 days. The patient’s history and physical that either support or refute the diagnosis. The history was obtained from both the patient’s. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: “i got. History And Physical Form Example.
From studylib.net
2. Intake History and Physical Form History And Physical Form Example Surgical/procedural indications and present illness: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Lower abdominal pain x 2 days. The patient’s history and physical that either support or refute the diagnosis. For each item on your differential, explain what. Sample pediatric history and physical exam. Explore the essential guide to the history. The history was. History And Physical Form Example.
From templatelab.com
43 Medical Health History Forms [PDF, Word] ᐅ TemplateLab History And Physical Form Example Sample pediatric history and physical exam. Surgical/procedural indications and present illness: “i got lightheadedness and felt. For each item on your differential, explain what. Date and time of h&p: The history was obtained from both the patient’s. Lower abdominal pain x 2 days. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a. History And Physical Form Example.
From www.bodyprotherapy.com
Medical History Form page 1 History And Physical Form Example “i got lightheadedness and felt. The patient’s history and physical that either support or refute the diagnosis. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The history was obtained from both the patient’s. Sample pediatric history and physical exam. For each item on your differential, explain what. Explore the. History And Physical Form Example.
From www.sampletemplates.com
FREE 8+ Sample Physical Exam Forms in PDF History And Physical Form Example Date and time of h&p: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Surgical/procedural indications and present illness: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. “i got lightheadedness and felt. Nausea and vomiting x 1 day. Sample pediatric history and physical exam. Lower. History And Physical Form Example.
From www.pdffiller.com
History And Physical Template Pdf Fill Online, Printable, Fillable History And Physical Form Example Surgical/procedural indications and present illness: The patient’s history and physical that either support or refute the diagnosis. For each item on your differential, explain what. Sample pediatric history and physical exam. Lower abdominal pain x 2 days. “i got lightheadedness and felt. Nausea and vomiting x 1 day. Date and time of h&p: It includes patient demographics, medical, family, and. History And Physical Form Example.
From www.template.net
8+ Yearly Physical Form Templates PDF History And Physical Form Example Explore the essential guide to the history. Lower abdominal pain x 2 days. Sample pediatric history and physical exam. Surgical/procedural indications and present illness: The history was obtained from both the patient’s. The patient’s history and physical that either support or refute the diagnosis. Date and time of h&p: Comprehensive adult history and physical (sample summative h&p by m2 student). History And Physical Form Example.
From printableformsfree.com
Printable History And Physical Forms Internal Medicine Printable History And Physical Form Example It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Sample pediatric history and physical exam. The patient’s history and physical that either support or refute the diagnosis. Nausea and vomiting x 1 day. Lower abdominal pain x. History And Physical Form Example.
From www.templateroller.com
Preemployment History and Physical Form Temple University Fill Out History And Physical Form Example The history was obtained from both the patient’s. Nausea and vomiting x 1 day. Date and time of h&p: “i got lightheadedness and felt. Explore the essential guide to the history. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Comprehensive adult history and physical (sample summative h&p by m2. History And Physical Form Example.
From www.slideshare.net
History & Physical Form PDF History And Physical Form Example Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The history was obtained from both the patient’s. For each item on your differential, explain what. Explore the essential guide to the history. Nausea and vomiting x 1 day. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical. History And Physical Form Example.
From www.sampletemplates.com
FREE 10+ Sample Medical History Forms in MS Word PDF History And Physical Form Example For each item on your differential, explain what. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Date and time of h&p: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. The history was obtained from both the patient’s. Explore the essential guide to the history.. History And Physical Form Example.
From www.dexform.com
Sample medical/physical history report form in Word and Pdf formats History And Physical Form Example Nausea and vomiting x 1 day. “i got lightheadedness and felt. The history was obtained from both the patient’s. Sample pediatric history and physical exam. Date and time of h&p: Lower abdominal pain x 2 days. Surgical/procedural indications and present illness: It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination.. History And Physical Form Example.
From www.template.net
8+ Yearly Physical Form Templates PDF History And Physical Form Example Date and time of h&p: Sample pediatric history and physical exam. Lower abdominal pain x 2 days. “i got lightheadedness and felt. Explore the essential guide to the history. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: For each item on your differential, explain what. The patient’s history and physical that either support or refute. History And Physical Form Example.
From enterstarcrypticcity.blogspot.com
History And Physical Examination Template PDF Template History And Physical Form Example The history was obtained from both the patient’s. It includes patient demographics, medical, family, and social history, a review of systems, and findings from a physical examination. Lower abdominal pain x 2 days. For each item on your differential, explain what. The patient’s history and physical that either support or refute the diagnosis. Surgical/procedural indications and present illness: Date and. History And Physical Form Example.