Weight Management Soap Note . Soap / chart / progress notes. The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. What is a nutrition soap note? A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. But knowing how to create an easy to read note is harder than it looks! The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The soap note format creates a systematic, easy to follow chart note. We will go through some tips for creating a soap. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. Keep a written or digital meal diary.
from www.studocu.com
We will go through some tips for creating a soap. Soap / chart / progress notes. Keep a written or digital meal diary. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The soap note format creates a systematic, easy to follow chart note. The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. But knowing how to create an easy to read note is harder than it looks! What is a nutrition soap note? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of.
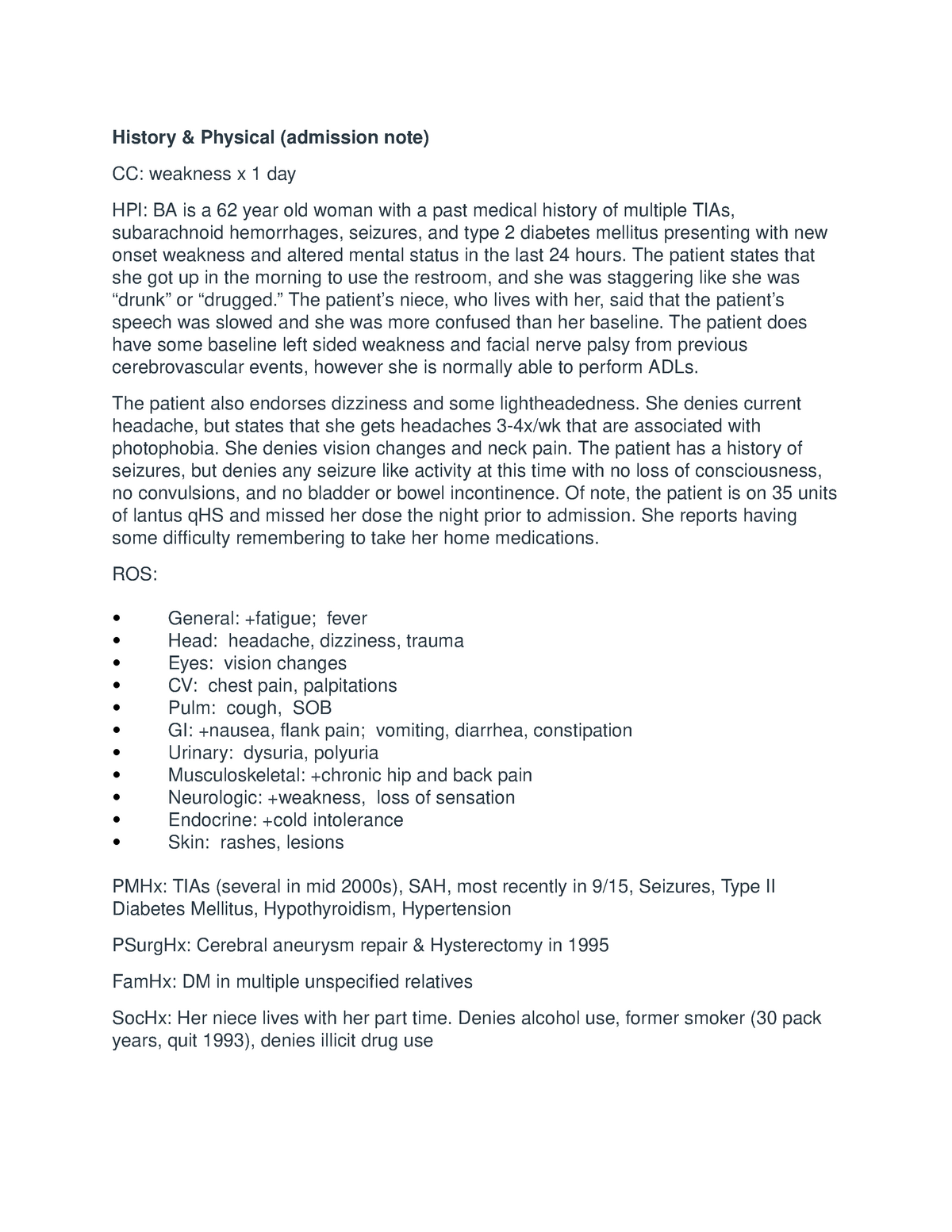
Sample H&P and SOAP note History & Physical (admission note) CC
Weight Management Soap Note The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. But knowing how to create an easy to read note is harder than it looks! Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. The soap note format creates a systematic, easy to follow chart note. Keep a written or digital meal diary. We will go through some tips for creating a soap. Soap / chart / progress notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. What is a nutrition soap note?
From learningmediacassandra.z21.web.core.windows.net
Soap Note Template Pdf Weight Management Soap Note What is a nutrition soap note? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. We will go through some tips for creating a soap. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. But knowing how to create an easy to read note. Weight Management Soap Note.
From tutore.org
Pain Management Soap Note Template Master of Documents Weight Management Soap Note But knowing how to create an easy to read note is harder than it looks! The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. Soap / chart / progress notes. The subjective, objective, assessment and plan. Weight Management Soap Note.
From www.hawkinsnewyork.com
Soap + Dish Gift Set Jasmine Hawkins New York Weight Management Soap Note The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. What is a nutrition soap note? A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and. Weight Management Soap Note.
From www.facebook.com
Coop Month Celebration Coop Month Celebration Kumustahan Session Part Weight Management Soap Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. We will go through some tips for creating a soap. Keep a written or digital meal diary. The soap note format creates a systematic, easy to follow chart note. But knowing how to create an easy to read note is harder than it. Weight Management Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Weight Management Soap Note But knowing how to create an easy to read note is harder than it looks! A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. The soap note format creates a systematic, easy to follow. Weight Management Soap Note.
From idtcenter.org
Sample 圖片So A P Notes Examples 精彩圖片搜 Doctors Note Pain Management Soap Weight Management Soap Note Keep a written or digital meal diary. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. Soap / chart / progress notes. The subjective, objective, assessment and plan (soap) note is an acronym representing. Weight Management Soap Note.
From www.hawkinsnewyork.com
Soap + Dish Gift Set Jasmine Hawkins New York Weight Management Soap Note The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. The soap note format creates a systematic, easy to follow chart note. Keep a written or digital meal diary. Learn how to document the nutrition care process. Weight Management Soap Note.
From www.pinterest.com
SOAP Note Template Etsy Notes template, Soap note, Templates Weight Management Soap Note Keep a written or digital meal diary. Soap / chart / progress notes. The soap note format creates a systematic, easy to follow chart note. We will go through some tips for creating a soap. What is a nutrition soap note? The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in. Weight Management Soap Note.
From www.printabletemplateslab.com
10+ Soap Note Template Free Download Word, Excel, PDF Format!! Weight Management Soap Note But knowing how to create an easy to read note is harder than it looks! The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Keep a written or digital meal diary. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. We will go. Weight Management Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Weight Management Soap Note The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. The soap note format creates a systematic, easy to follow chart note. Soap / chart / progress notes. What is a nutrition soap note? But knowing how to create an easy to read note is harder than it. Weight Management Soap Note.
From www.studocu.com
Sample H&P and SOAP note History & Physical (admission note) CC Weight Management Soap Note The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. Keep a written or digital meal diary. The soap note format creates a systematic, easy to follow chart note. Soap / chart / progress notes. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis,. Weight Management Soap Note.
From www.facebook.com
Community Checkup Oct. 17, 2024 COMMUNITY CHECKUP Oct. 17, 2024 Weight Management Soap Note What is a nutrition soap note? The soap note format creates a systematic, easy to follow chart note. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. Keep a written or digital meal diary. A nutrition. Weight Management Soap Note.
From essaywritinghelp.net
Lower Back Pain Soap Note Examples Essay Writing Help Weight Management Soap Note A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. Keep a written or digital meal diary. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss. Weight Management Soap Note.
From www.facebook.com
Community Checkup Oct. 17, 2024 COMMUNITY CHECKUP Oct. 17, 2024 Weight Management Soap Note The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. The obesity management checklist is intended to be used in. Weight Management Soap Note.
From www.uslegalforms.com
Weight Loss Progress Note Template Fill and Sign Printable Template Weight Management Soap Note A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. Keep a written or digital meal diary. But knowing how to create an easy to read note is harder than it looks! The soap note. Weight Management Soap Note.
From www.scribd.com
soap note tpn mize Weight Loss Health Sciences Weight Management Soap Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. Soap / chart / progress notes. A nutrition soap note. Weight Management Soap Note.
From www.facebook.com
Community Checkup Oct. 17, 2024 COMMUNITY CHECKUP Oct. 17, 2024 Weight Management Soap Note Keep a written or digital meal diary. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. We will go through some tips for creating a soap. But knowing how to create an easy to read note is harder than it looks! The soap note format, the acronym of which stands for subjective,. Weight Management Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Weight Management Soap Note Soap / chart / progress notes. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. Keep a written or. Weight Management Soap Note.
From idtcenter.org
Pain Management Soap Note Template Weight Management Soap Note The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. But knowing how to create an easy to read note is harder than it looks! What is a nutrition soap note? A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to. Weight Management Soap Note.
From www.pinterest.com
soap note template counseling Google Search SOAP Notes Pinterest Weight Management Soap Note The soap note format creates a systematic, easy to follow chart note. Soap / chart / progress notes. We will go through some tips for creating a soap. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment. Weight Management Soap Note.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Weight Management Soap Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. What is a nutrition soap note? The soap note format creates a systematic, easy to follow chart note. Soap / chart / progress notes. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. Learn. Weight Management Soap Note.
From www.carecloud.com
Free SOAP Notes Template CareCloud Continuum Weight Management Soap Note Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Keep a written or digital meal diary. The soap note format creates a systematic, easy to follow chart note. Soap / chart / progress notes. What. Weight Management Soap Note.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help Weight Management Soap Note But knowing how to create an easy to read note is harder than it looks! Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. Keep a written or digital meal diary. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. Soap / chart. Weight Management Soap Note.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Weight Management Soap Note What is a nutrition soap note? Keep a written or digital meal diary. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap / chart / progress notes. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare. Weight Management Soap Note.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Weight Management Soap Note The soap note format creates a systematic, easy to follow chart note. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. We will go through some tips for creating a soap. But knowing how to create an easy to read note is harder than it looks! The soap note format, the. Weight Management Soap Note.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For Weight Management Soap Note The soap note format creates a systematic, easy to follow chart note. A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. But knowing how to create an easy to read note is harder than. Weight Management Soap Note.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Weight Management Soap Note A nutrition soap note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document. Soap / chart / progress notes. We will go through some tips for creating a soap. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use. Weight Management Soap Note.
From idtcenter.org
Printable Wellness Massage Versus Therapeutic Massage Relaxing Pain Weight Management Soap Note The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. But knowing how to create an easy to read note is harder than it looks! Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The soap note format, the acronym of which stands for subjective,. Weight Management Soap Note.
From templates.udlvirtual.edu.pe
Free Printable Soap Notes For Massage Therapy PRINTABLE TEMPLATES Weight Management Soap Note Keep a written or digital meal diary. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. What is a. Weight Management Soap Note.
From www.hawkinsnewyork.com
Soap + Dish Gift Set Jasmine Hawkins New York Weight Management Soap Note Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. But knowing how to create an easy to read note is harder than it looks! The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. We will go through some tips. Weight Management Soap Note.
From www.facebook.com
Community Checkup Oct. 17, 2024 COMMUNITY CHECKUP Oct. 17, 2024 Weight Management Soap Note The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. The soap note format creates a systematic, easy to follow chart note. We will go through some tips for creating a soap. Learn how to document the. Weight Management Soap Note.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Nutrition Weight Management Soap Note What is a nutrition soap note? Keep a written or digital meal diary. The soap note format creates a systematic, easy to follow chart note. But knowing how to create an easy to read note is harder than it looks! Learn how to document the nutrition care process (ncp) steps of assessment, diagnosis, intervention, monitoring, and evaluation. The obesity management. Weight Management Soap Note.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Weight Management Soap Note The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. What is a nutrition soap note? Keep a written or digital meal diary. But knowing how to create an easy to read note is harder than it. Weight Management Soap Note.
From www.vrogue.co
Printable Soap Notes Fill Out And Sign Printable Pdf vrogue.co Weight Management Soap Note Soap / chart / progress notes. But knowing how to create an easy to read note is harder than it looks! The obesity management checklist is intended to be used in serial fashion to support and encourage weight loss in obese adults and. The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one. Weight Management Soap Note.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap Weight Management Soap Note The soap note format, the acronym of which stands for subjective, objective, assessment, and plan, is one of the standard document formats that healthcare providers use to document patient information and treatment progress. Keep a written or digital meal diary. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. What is a. Weight Management Soap Note.