Cvs Caremark Botox Prior Authorization Form 2022 . to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa is needed for a prescription, the member will be asked to. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is.
from www.pdffiller.com
this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan.
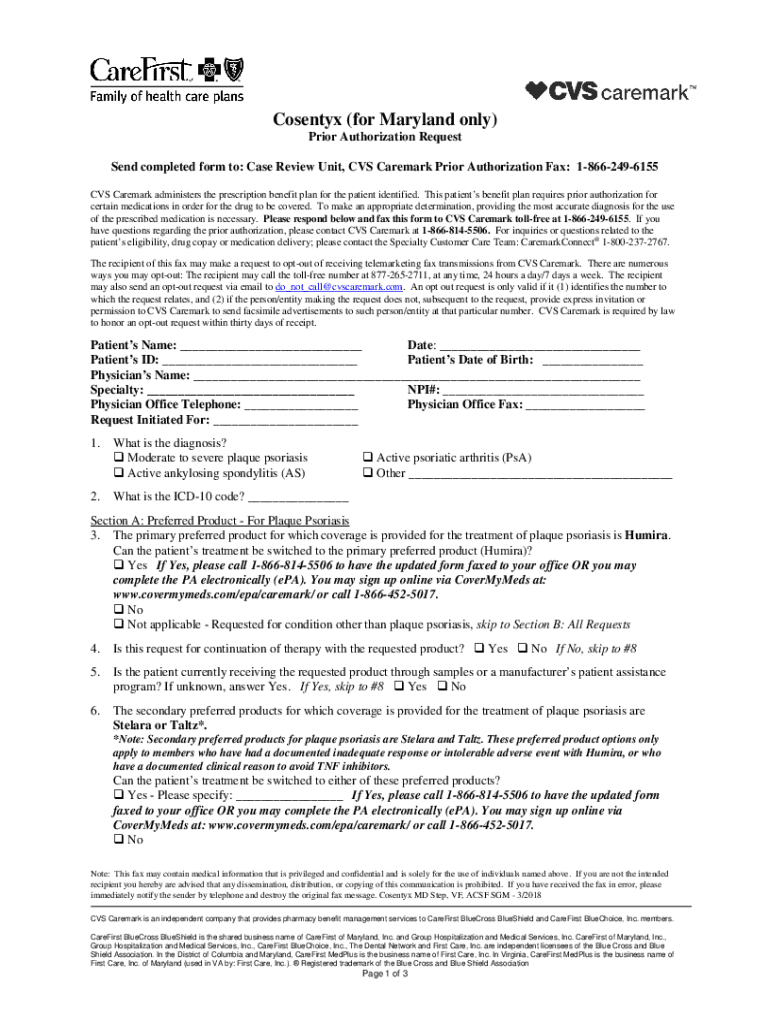
Fillable Online CVS/Caremark Prior (Rx) Authorization Form eForms Fax
Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa is needed for a prescription, the member will be asked to. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. — we offer access to specialty medications and infusion therapies, centralized intake and benefits.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june 02, 2022. to make an appropriate determination, providing. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print Cvs Caremark Botox Prior Authorization Form 2022 this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. When a pa is needed for a prescription, the member will be asked to. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the. Cvs Caremark Botox Prior Authorization Form 2022.
From www.templateroller.com
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination,. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june 02, 2022. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. —. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online Cvs caremark prior authorization form Fax Email Print Cvs Caremark Botox Prior Authorization Form 2022 this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the. Cvs Caremark Botox Prior Authorization Form 2022.
From www.authorizationform.net
Caremark Specialty Pharmacy Prior Authorization Form Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. this policy informs prescribers of preferred. Cvs Caremark Botox Prior Authorization Form 2022.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Botox Prior Authorization Form 2022 A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated. Cvs Caremark Botox Prior Authorization Form 2022.
From www.authorizationform.net
Cvs Caremark Ivig Prior Authorization Form Cvs Caremark Botox Prior Authorization Form 2022 — we offer access to specialty medications and infusion therapies, centralized intake and benefits. updated june 02, 2022. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa. Cvs Caremark Botox Prior Authorization Form 2022.
From www.templateroller.com
Botox Passport Prior Authorization Request Form Cvs Caremark Fill Cvs Caremark Botox Prior Authorization Form 2022 this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june. Cvs Caremark Botox Prior Authorization Form 2022.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. this policy informs prescribers of preferred products and provides an exception process for targeted products through. Cvs Caremark Botox Prior Authorization Form 2022.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. When a pa is needed for a prescription,. Cvs Caremark Botox Prior Authorization Form 2022.
From errnodjembewinboost.pages.dev
Cvs Caremark Prior Authorization Form Cvs Pharmacy Release Form Cvs Caremark Botox Prior Authorization Form 2022 this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. updated june 02, 2022. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. When a. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online Cvs caremark specialty pharmacy prior authorization Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. — we offer access to specialty. Cvs Caremark Botox Prior Authorization Form 2022.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa is needed for a prescription, the member will be asked to. this policy informs prescribers of preferred products. Cvs Caremark Botox Prior Authorization Form 2022.
From www.sampletemplates.com
FREE 8+ Sample Caremark Prior Authorization Forms in PDF Cvs Caremark Botox Prior Authorization Form 2022 — we offer access to specialty medications and infusion therapies, centralized intake and benefits. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination,. Cvs Caremark Botox Prior Authorization Form 2022.
From www.dochub.com
Cvs caremark prior authorization form Fill out & sign online DocHub Cvs Caremark Botox Prior Authorization Form 2022 — we offer access to specialty medications and infusion therapies, centralized intake and benefits. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june 02, 2022. . Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online CVS/Caremark Prior (Rx) Authorization Form eForms Fax Cvs Caremark Botox Prior Authorization Form 2022 updated june 02, 2022. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. When a pa is needed for a prescription, the member will be asked to. this policy informs prescribers of. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Cvs Caremark Prior Authorization Form For Fill Online, Printable Cvs Caremark Botox Prior Authorization Form 2022 this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. — we offer. Cvs Caremark Botox Prior Authorization Form 2022.
From www.authorizationform.net
Cvs Caremark Synagis Prior Authorization Form Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to be. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online Cvs Caremark Prior Authorization Form Fax Email Print Cvs Caremark Botox Prior Authorization Form 2022 A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. updated june 02, 2022. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination,. Cvs Caremark Botox Prior Authorization Form 2022.
From www.sampletemplates.com
9+ Sample Caremark Prior Authorization Forms Sample Templates Cvs Caremark Botox Prior Authorization Form 2022 this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june 02, 2022. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. A cvs/caremark prior. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online contact CVS Caremark at 18556337673 with questions Cvs Caremark Botox Prior Authorization Form 2022 updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa is needed for a prescription, the member will be asked to. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. to make an appropriate determination, providing. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Botox Prior Authorization Form 2022 A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa is needed for a prescription, the member will be asked to. — we offer access to specialty. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online Get Cvs Caremark Prior Authorization Form Fax Email Cvs Caremark Botox Prior Authorization Form 2022 updated june 02, 2022. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to. Cvs Caremark Botox Prior Authorization Form 2022.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Botox Prior Authorization Form 2022 A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. When a pa. Cvs Caremark Botox Prior Authorization Form 2022.
From www.templateroller.com
Botox Consent Form Fill Out, Sign Online and Download PDF Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. — we offer access to specialty medications. Cvs Caremark Botox Prior Authorization Form 2022.
From www.templateroller.com
Botox Passport Prior Authorization Request Form Cvs Caremark Fill Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. When a pa is needed for a prescription, the member will be asked to. — we offer access to specialty medications and. Cvs Caremark Botox Prior Authorization Form 2022.
From moussyusa.com
Template Caremark Prior Authorization Form Mous Syusa Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. updated june 02, 2022. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. —. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online CVS Caremark Prior Authorization Provider Resource Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. When a pa is needed for a prescription, the member will be asked to. A cvs/caremark prior authorization form is to be. Cvs Caremark Botox Prior Authorization Form 2022.
From www.uslegalforms.com
Cvs Caremark Prescription Form 20202022 Fill and Sign Printable Cvs Caremark Botox Prior Authorization Form 2022 A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. When a pa is needed for a prescription, the member will be asked to. this policy informs prescribers of preferred products and provides an. Cvs Caremark Botox Prior Authorization Form 2022.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Botox Prior Authorization Form 2022 to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. updated june 02, 2022. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. When a pa. Cvs Caremark Botox Prior Authorization Form 2022.
From www.authorizationform.net
Cvs Caremark Wegovy Prior Authorization Form Cvs Caremark Botox Prior Authorization Form 2022 updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Cvs Caremark Formulary Exception Prior Authorization Request Form Cvs Caremark Botox Prior Authorization Form 2022 A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. When a pa is needed for a prescription, the member will be asked to. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. updated june 02, 2022. this. Cvs Caremark Botox Prior Authorization Form 2022.
From www.authorizationform.net
Cvs Pharmacy Prior Authorization Form Cvs Caremark Botox Prior Authorization Form 2022 When a pa is needed for a prescription, the member will be asked to. — we offer access to specialty medications and infusion therapies, centralized intake and benefits. this policy informs prescribers of preferred products and provides an exception process for targeted products through prior. A cvs/caremark prior authorization form is to be used by a medical office. Cvs Caremark Botox Prior Authorization Form 2022.
From www.pdffiller.com
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF Cvs Caremark Botox Prior Authorization Form 2022 updated june 02, 2022. to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan. to make an appropriate determination, providing the most accurate diagnosis for the use of the. Cvs Caremark Botox Prior Authorization Form 2022.