What Is Soap Analysis . Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. What is a soap note? Each letter refers to one of four sections in the document you will. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. They contain four primary sections, represented by its acronym:
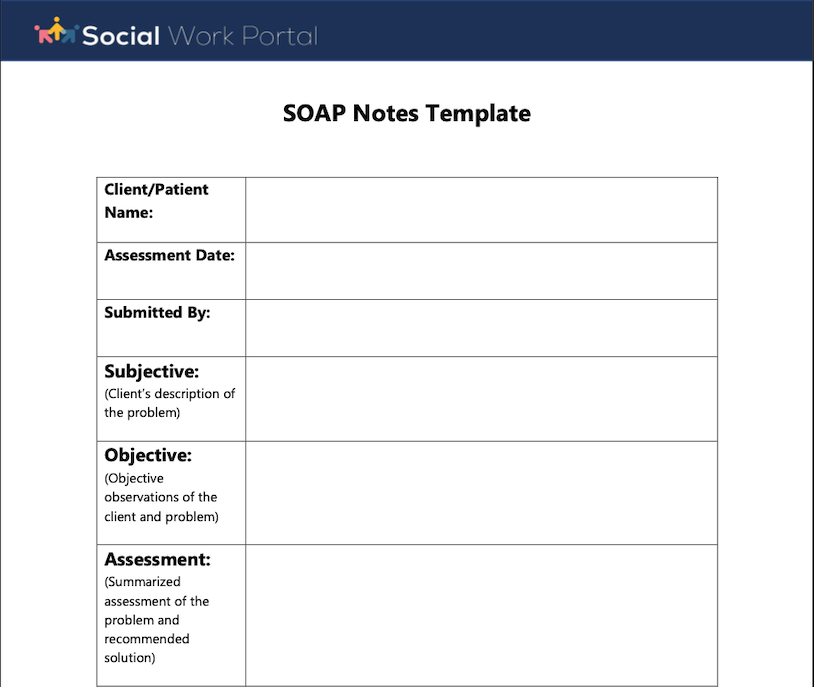
from www.socialworkportal.com
Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. They contain four primary sections, represented by its acronym: What is a soap note? Each letter refers to one of four sections in the document you will. Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for subjective, objective, assessment, and plan.
How to Write a Social Work Soap Assessment Best Guide to Soap
What Is Soap Analysis What is a soap note? Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note? In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document you will. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Exactly what is a soap note?. They contain four primary sections, represented by its acronym: Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals.
From www.edrawmax.com
Free Editable SOAPSTone Graphic Organizer Examples EdrawMax Online What Is Soap Analysis Each letter refers to one of four sections in the document you will. Exactly what is a soap note?. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. In the soap format, soap stands. What Is Soap Analysis.
From kelitbanganwonogiri.org
Soap Assessment Template What Is Soap Analysis Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Each letter refers to one of four sections in the document you will. What is a soap note? The subjective, objective, assessment and plan (soap) note is. What Is Soap Analysis.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary What Is Soap Analysis What is a soap note? In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document you will. Exactly what is a soap note?. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a structured way of recording. What Is Soap Analysis.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by What Is Soap Analysis Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. What is a soap note? In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document you will. Soap notes are a specific format for writing progress notes as a. What Is Soap Analysis.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Is Soap Analysis Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note? Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for. What Is Soap Analysis.
From thevisualcommunicationguy.com
SOAPStoneWritingStrategy_Reference The Visual Communication Guy What Is Soap Analysis Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Soap notes are a specific format for writing progress notes as a behavioral health clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Exactly what is a soap note?. What. What Is Soap Analysis.
From www.semanticscholar.org
DAILY FOLLOW UP NOTES’ ACCURACY ACCORDING TO SOAP (SUBJECTIVE What Is Soap Analysis They contain four primary sections, represented by its acronym: Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. What is a soap note? Each letter refers to one of four sections in the document you will. Soap notes are a structured way of. What Is Soap Analysis.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example What Is Soap Analysis Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Each letter refers to one of four sections in the document you will. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Soap notes are a specific format for writing progress. What Is Soap Analysis.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] What Is Soap Analysis Exactly what is a soap note?. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. They contain four primary. What Is Soap Analysis.
From klaazngam.blob.core.windows.net
Soap Note Example Social Work at Marie Bramlett blog What Is Soap Analysis Exactly what is a soap note?. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Each letter refers to one of four sections in the document you will. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a specific format. What Is Soap Analysis.
From mavink.com
Ejemplo De Nota Soap What Is Soap Analysis Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. What is a soap note? Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. They contain four primary sections, represented by. What Is Soap Analysis.
From www.chegg.com
Solved Case Presentation Using SOAP analysis please complete What Is Soap Analysis In the soap format, soap stands for subjective, objective, assessment, and plan. What is a soap note? They contain four primary sections, represented by its acronym: Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are. What Is Soap Analysis.
From www.slideshare.net
soap analysis PPT What Is Soap Analysis Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. What is a soap note? Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Soap notes are a structured way of. What Is Soap Analysis.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is Soap Analysis Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. They contain four primary sections,. What Is Soap Analysis.
From www.etsy.com
Primary Source Analysis Anchor Chart, SOAPS Strategy Anchor Chart What Is Soap Analysis Soap notes are a specific format for writing progress notes as a behavioral health clinician. Each letter refers to one of four sections in the document you will. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in. What Is Soap Analysis.
From www.pinterest.com
SOAP vs SBAR Nursing school tips, Nursing school survival, Nursing What Is Soap Analysis Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: What is a soap note? Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a way for healthcare providers to document patient data more efficiently. What Is Soap Analysis.
From iblog.dearbornschools.org
NewsELA Article Instructions Miss P's Classroom Blog What Is Soap Analysis The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Each letter refers to one of four sections in the document you will. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and. What Is Soap Analysis.
From www.peterainsworth.com
Soap Documentation Example What Is Soap Analysis What is a soap note? The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its. What Is Soap Analysis.
From www.studypool.com
SOLUTION Swot Analysis For Natural Soap Studypool What Is Soap Analysis Each letter refers to one of four sections in the document you will. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. What is a soap note? Soap notes are a way for healthcare providers to document patient data more efficiently and. What Is Soap Analysis.
From www.slideserve.com
PPT How is Soap Made? PowerPoint Presentation, free download ID2530430 What Is Soap Analysis Soap notes are a specific format for writing progress notes as a behavioral health clinician. Exactly what is a soap note?. What is a soap note? In the soap format, soap stands for subjective, objective, assessment, and plan. Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. Soap notes are a structured. What Is Soap Analysis.
From www.etsy.com
Primary Source Analysis Anchor Chart, SOAPS Strategy Anchor Chart What Is Soap Analysis In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Exactly what is a soap note?. What is a soap note? They contain four primary sections, represented by its acronym: Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters. What Is Soap Analysis.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is Soap Analysis What is a soap note? Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for subjective, objective, assessment, and plan. They contain four primary sections, represented by its acronym: Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Soap. What Is Soap Analysis.
From peterhurst.z13.web.core.windows.net
The E Entry In The Soaper Charting Method Means What Is Soap Analysis What is a soap note? They contain four primary sections, represented by its acronym: In the soap format, soap stands for subjective, objective, assessment, and plan. Exactly what is a soap note?. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap notes are a structured way of recording the progress of a patient. What Is Soap Analysis.
From www.scribd.com
SOAP Analysis PDF Hypertension Diseases And Disorders What Is Soap Analysis They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note. What Is Soap Analysis.
From www.theraplatform.com
Occupational therapy SOAP note What Is Soap Analysis Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Each letter refers to one of four sections in the document you will. What is a soap note?. What Is Soap Analysis.
From www.pinterest.com
SOAPS Primary Source Analysis Anchor Chart/Poster & Graphic Organizer What Is Soap Analysis Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. They contain four primary sections, represented by its acronym: The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Soap notes are a way for healthcare providers to document patient data more. What Is Soap Analysis.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox What Is Soap Analysis Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Soap notes are a specific format for writing progress notes as a behavioral health clinician. What is a soap note? Soap notes. What Is Soap Analysis.
From www.peterainsworth.com
Soap Documentation Example What Is Soap Analysis What is a soap note? Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. The subjective, objective, assessment and plan (soap) note is. What Is Soap Analysis.
From www.edrawmax.com
Free Editable SOAPSTone Graphic Organizer Examples EdrawMax Online What Is Soap Analysis Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Each letter refers to one of four sections. What Is Soap Analysis.
From www.slideserve.com
PPT Patient Medical Records PowerPoint Presentation, free download What Is Soap Analysis The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Each letter refers to one of four sections in the document you will. Exactly what is a soap note?. Soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented. What Is Soap Analysis.
From www.socialworkportal.com
How to Write a Social Work Soap Assessment Best Guide to Soap What Is Soap Analysis The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Exactly what is a soap note?. Each letter refers to one of four sections in the document you will. Soap notes are a structured way of recording the progress of a patient during treatment by health professionals. Soap notes are. What Is Soap Analysis.
From topanswerideas.com
The Importance of Soap Notes in Well Woman Exams A Comprehensive Guide What Is Soap Analysis What is a soap note? Soap notes are a specific format for writing progress notes as a behavioral health clinician. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Each letter refers to one of four sections in the document you will. They contain four primary sections, represented by. What Is Soap Analysis.
From www.slideserve.com
PPT PATIENT MEDICAL RECORDS PowerPoint Presentation, free download What Is Soap Analysis What is a soap note? Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Exactly what is a soap note?. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Soap notes are a structured way of recording the progress of a patient. What Is Soap Analysis.
From www.youtube.com
Intro to SOAPS Tone Analysis YouTube What Is Soap Analysis The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. Each letter refers to one of four sections in the document you will. What is a soap note? They contain four primary sections, represented by its acronym: Soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters. What Is Soap Analysis.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education What Is Soap Analysis Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare. They contain four primary sections, represented by its acronym: In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are. What Is Soap Analysis.