What Type Of Abbreviation Is Soap . Soap is an acronym for subjective, objective, assessment, and plan. documenting a patient assessment in the notes is something all medical students need to practice. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. The patient’s feelings about the issue and how it impacts his/her life. what does soap stand for? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Subjective, objective, assessment, and plan. These four components form the basis. For which of the following does the abbreviation pt stand?. soap is an acronym based on each of the note’s four components:
from www.studocu.com
what does soap stand for? documenting a patient assessment in the notes is something all medical students need to practice. For which of the following does the abbreviation pt stand?. The patient’s feelings about the issue and how it impacts his/her life. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. Soap is an acronym for subjective, objective, assessment, and plan. Subjective, objective, assessment, and plan. soap is an acronym based on each of the note’s four components: the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. These four components form the basis.
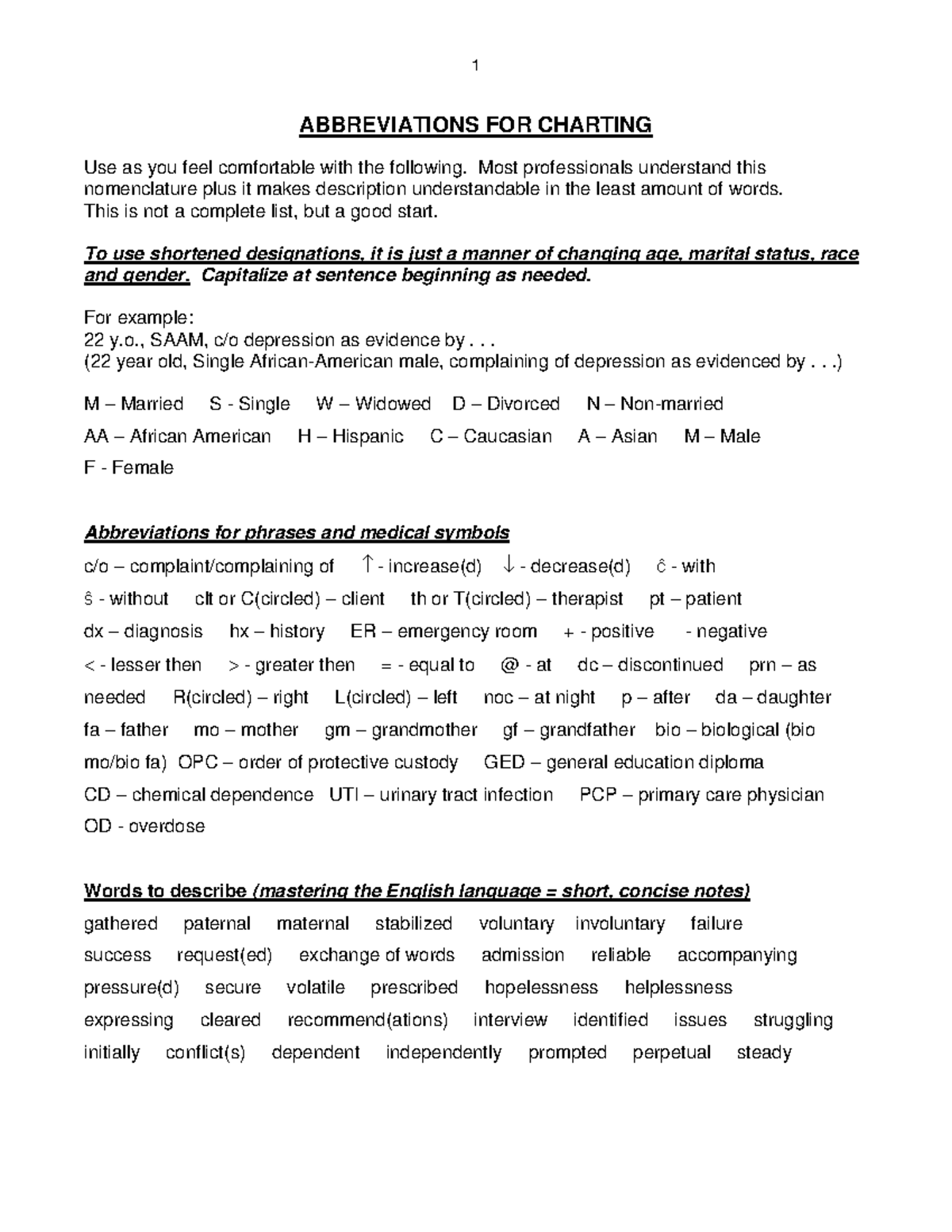
AbbreviationsForCharting when SOAP NOTES , counseling Notes, Therapy
What Type Of Abbreviation Is Soap what does soap stand for? soap is an acronym based on each of the note’s four components: These four components form the basis. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. The patient’s feelings about the issue and how it impacts his/her life. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. what does soap stand for? Subjective, objective, assessment, and plan. Soap is an acronym for subjective, objective, assessment, and plan. For which of the following does the abbreviation pt stand?. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. documenting a patient assessment in the notes is something all medical students need to practice.
From www.pinterest.com
Soapmaking Terms and Abbreviations Soapmaking, Abbreviations, Terms What Type Of Abbreviation Is Soap For which of the following does the abbreviation pt stand?. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. documenting a patient assessment in the notes is something all medical students need to practice. These four components form the basis. Subjective, objective, assessment, and plan. soap is an acronym based on each of the. What Type Of Abbreviation Is Soap.
From willetteshomelaundry.com
Information On The Different Types Of Cleaning Soaps Willette's Home What Type Of Abbreviation Is Soap Subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. For which of the following does the abbreviation pt stand?. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. soap is an acronym based on each. What Type Of Abbreviation Is Soap.
From livingnorm.com
All Types of Bathing Soap Living Norm What Type Of Abbreviation Is Soap Soap is an acronym for subjective, objective, assessment, and plan. These four components form the basis. what does soap stand for? soap is an acronym based on each of the note’s four components: For which of the following does the abbreviation pt stand?. soap notes are a highly structured format for documenting the progress of a patient. What Type Of Abbreviation Is Soap.
From freyaburke.z13.web.core.windows.net
Soap Note Abbreviations List What Type Of Abbreviation Is Soap Subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. The patient’s feelings about the issue and how it impacts his/her life. what does soap stand for? Soap is an acronym for subjective, objective, assessment, and plan. the subjective, objective, assessment and plan (soap) note is an acronym representing a. What Type Of Abbreviation Is Soap.
From www.ultimatehpsoap.com
Soap Making Abbreviations Made EASY! What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. For which of the following does the abbreviation pt stand?. soap is an acronym based on each of the note’s four components: Subjective, objective, assessment,. What Type Of Abbreviation Is Soap.
From www.youtube.com
Types of Soap, Chemistry Lecture Sabaq.pk YouTube What Type Of Abbreviation Is Soap soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. soap is an acronym based on each of the note’s four components: Soap. What Type Of Abbreviation Is Soap.
From glowsly.com
Types of Bar Soaps Choosing the Right Type for Your Skin Glowsly What Type Of Abbreviation Is Soap Subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. The patient’s feelings about the issue and how it impacts his/her life. documenting a patient assessment in the notes is something all medical students need to practice. the subjective, objective, assessment and plan (soap) note is an acronym representing a. What Type Of Abbreviation Is Soap.
From education2research.com
The Importance of a Well Woman Exam Soap Note A Comprehensive Guide What Type Of Abbreviation Is Soap soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. The patient’s feelings about the issue and how it impacts his/her life. documenting a patient assessment in. What Type Of Abbreviation Is Soap.
From www.youtube.com
Abbreviations in SOAP Notes Part 2 YouTube What Type Of Abbreviation Is Soap Subjective, objective, assessment, and plan. The patient’s feelings about the issue and how it impacts his/her life. soap is an acronym based on each of the note’s four components: soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. the subjective, objective, assessment and. What Type Of Abbreviation Is Soap.
From homeporio.blogspot.com
22 Different Types of Soap Homeporio What Type Of Abbreviation Is Soap Soap is an acronym for subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. what does soap stand for? soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. For which of the following does the. What Type Of Abbreviation Is Soap.
From www.theraplatform.com
Occupational therapy SOAP note What Type Of Abbreviation Is Soap documenting a patient assessment in the notes is something all medical students need to practice. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. what does soap stand for? soap notes. What Type Of Abbreviation Is Soap.
From www.scienceabc.com
Difference Between Types Of Soaps, Shampoos And Detergents What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. documenting a patient assessment in the notes is something all medical students need to practice. Subjective, objective, assessment, and plan. soap is an acronym based on each of the note’s four components: soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. . What Type Of Abbreviation Is Soap.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Type Of Abbreviation Is Soap Subjective, objective, assessment, and plan. For which of the following does the abbreviation pt stand?. These four components form the basis. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. documenting a patient assessment in the notes is something all medical students need to. What Type Of Abbreviation Is Soap.
From enrichbodycare.com
Different types of commercial soapsEnrich Bodycare What Type Of Abbreviation Is Soap Soap is an acronym for subjective, objective, assessment, and plan. what does soap stand for? These four components form the basis. Subjective, objective, assessment, and plan. soap is an acronym based on each of the note’s four components: the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for. What Type Of Abbreviation Is Soap.
From www.albogroupitaly.com
The different types of soap and its properties What Type Of Abbreviation Is Soap the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap is an acronym for subjective, objective, assessment, and plan. For which of the following does the abbreviation pt stand?. The patient’s feelings about the issue and how it impacts his/her life. soap is an acronym based. What Type Of Abbreviation Is Soap.
From www.youtube.com
How to Write SOAP Notes YouTube What Type Of Abbreviation Is Soap what does soap stand for? Subjective, objective, assessment, and plan. The patient’s feelings about the issue and how it impacts his/her life. soap is an acronym based on each of the note’s four components: For which of the following does the abbreviation pt stand?. These four components form the basis. the subjective, objective, assessment and plan (soap). What Type Of Abbreviation Is Soap.
From www.pinterest.com
Medical Mnemonics Diagnostic Criteria for SLE Soap Brain MD What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. Subjective, objective, assessment, and plan. documenting a patient assessment in the notes is something all medical students need to practice. For which of the following does the abbreviation pt stand?. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. what does soap. What Type Of Abbreviation Is Soap.
From www.youtube.com
50 Types of Handmade Soaps Learn Soap Making at Home SMB HUNAR What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. These four components form the basis. Subjective, objective, assessment, and plan. For which of the following does the abbreviation pt stand?. documenting a patient assessment. What Type Of Abbreviation Is Soap.
From thenovastudio.com
Free Printable Common Abbreviations for Soap, Fizzies, & More The What Type Of Abbreviation Is Soap documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. what does soap stand for? soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. The. What Type Of Abbreviation Is Soap.
From www.pinterest.com
Soapmaking Terms and Abbreviations Soapmaking, Soap, Soap making What Type Of Abbreviation Is Soap For which of the following does the abbreviation pt stand?. Subjective, objective, assessment, and plan. Soap is an acronym for subjective, objective, assessment, and plan. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. soap is an acronym based on each of the note’s. What Type Of Abbreviation Is Soap.
From www.studypool.com
SOLUTION Soapie medical abbreviations Studypool What Type Of Abbreviation Is Soap For which of the following does the abbreviation pt stand?. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. The patient’s feelings about the issue and how it impacts his/her life. documenting a patient assessment in the notes is something all medical students need to practice. Soap is an acronym for subjective, objective, assessment, and. What Type Of Abbreviation Is Soap.
From www.youtube.com
Soaps and Syndet Bars ! Type of soaps ! Unit4 L6 ! Cosmetic science What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. For which of the following does the abbreviation pt stand?. what does soap stand for? Subjective, objective, assessment, and plan. Soap is an acronym for. What Type Of Abbreviation Is Soap.
From www.theottoolbox.com
Occupational Therapy Documentation Tips The OT Toolbox What Type Of Abbreviation Is Soap Soap is an acronym for subjective, objective, assessment, and plan. The patient’s feelings about the issue and how it impacts his/her life. what does soap stand for? the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. These four components form the basis. documenting a patient. What Type Of Abbreviation Is Soap.
From www.vrogue.co
Soap Charting Pinteres vrogue.co What Type Of Abbreviation Is Soap soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. documenting a patient assessment in the notes is something all medical students need to practice. what does soap stand for? For which of the following does the abbreviation pt stand?. The patient’s feelings about. What Type Of Abbreviation Is Soap.
From www.studocu.com
Soap note abbreviations(2) SOAP NOTE Common Abbreviations It is What Type Of Abbreviation Is Soap documenting a patient assessment in the notes is something all medical students need to practice. soap is an acronym based on each of the note’s four components: The patient’s feelings about the issue and how it impacts his/her life. soap notes are a highly structured format for documenting the progress of a patient during treatment and is. What Type Of Abbreviation Is Soap.
From 7esl.com
Abbreviations A Concise Guide to Understanding and Using Them • 7ESL What Type Of Abbreviation Is Soap Subjective, objective, assessment, and plan. soap is an acronym based on each of the note’s four components: documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. what. What Type Of Abbreviation Is Soap.
From www.alamy.com
Speech bubble illustration of information technology acronym What Type Of Abbreviation Is Soap the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Soap. What Type Of Abbreviation Is Soap.
From www.youtube.com
Soap From Different Countries Soap Brands YouTube What Type Of Abbreviation Is Soap soap is an acronym based on each of the note’s four components: These four components form the basis. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. what does soap stand for? For which of the following does the abbreviation pt stand?. The. What Type Of Abbreviation Is Soap.
From www.scribd.com
Abbreviations By Kettenbach Writing SOAP Notes 2 Edition PDF What Type Of Abbreviation Is Soap For which of the following does the abbreviation pt stand?. Soap is an acronym for subjective, objective, assessment, and plan. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible.. What Type Of Abbreviation Is Soap.
From fullrliving.com
SOAPS, IS IT IMPORTANT WHICH TYPE YOU USE? Fullrliving Eco Living What Type Of Abbreviation Is Soap For which of the following does the abbreviation pt stand?. These four components form the basis. Soap is an acronym for subjective, objective, assessment, and plan. what does soap stand for? soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. soap notes are a highly structured format for documenting the progress of a patient. What Type Of Abbreviation Is Soap.
From www.youtube.com
4) Beginner Soap Making Series Soap abbreviations and Terms YouTube What Type Of Abbreviation Is Soap soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. what does soap stand for? Subjective, objective, assessment, and plan. Soap is an acronym for subjective, objective, assessment, and plan. The patient’s feelings about the issue and how it impacts his/her life. documenting a patient assessment in the notes is something all medical students need. What Type Of Abbreviation Is Soap.
From www.youtube.com
TYPES OF SOAPS YouTube What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. Soap is an acronym for subjective, objective, assessment, and plan. soap is an acronym based on each of the note’s four components: soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. These four components form the basis. For which of the following does. What Type Of Abbreviation Is Soap.
From www.studocu.com
AbbreviationsForCharting when SOAP NOTES , counseling Notes, Therapy What Type Of Abbreviation Is Soap soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. Subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient. These four components form the basis. The patient’s feelings about the issue and how it impacts his/her life.. What Type Of Abbreviation Is Soap.
From www.dreamstime.com
Abbreviation Soap Stock Photos Free & RoyaltyFree Stock Photos from What Type Of Abbreviation Is Soap The patient’s feelings about the issue and how it impacts his/her life. For which of the following does the abbreviation pt stand?. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. what does soap stand for? soap—or subjective, objective, assessment and plan—notes allow. What Type Of Abbreviation Is Soap.
From asoothingliving.com
10 Different Types of Soap and Their Usage What Type Of Abbreviation Is Soap the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. For which of the following does the abbreviation pt stand?. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible. soap is an. What Type Of Abbreviation Is Soap.