What Is Retro Authorization In Medical Billing . Retro authorization secures approval for medical services already rendered to a patient. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. It refers to obtaining approval for medical services. Obtained before the service is provided. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Obtained during an ongoing treatment, often for extended.
from www.ncertbooks.guru
Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization secures approval for medical services already rendered to a patient. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. It refers to obtaining approval for medical services. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Obtained during an ongoing treatment, often for extended. Obtained before the service is provided. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to.
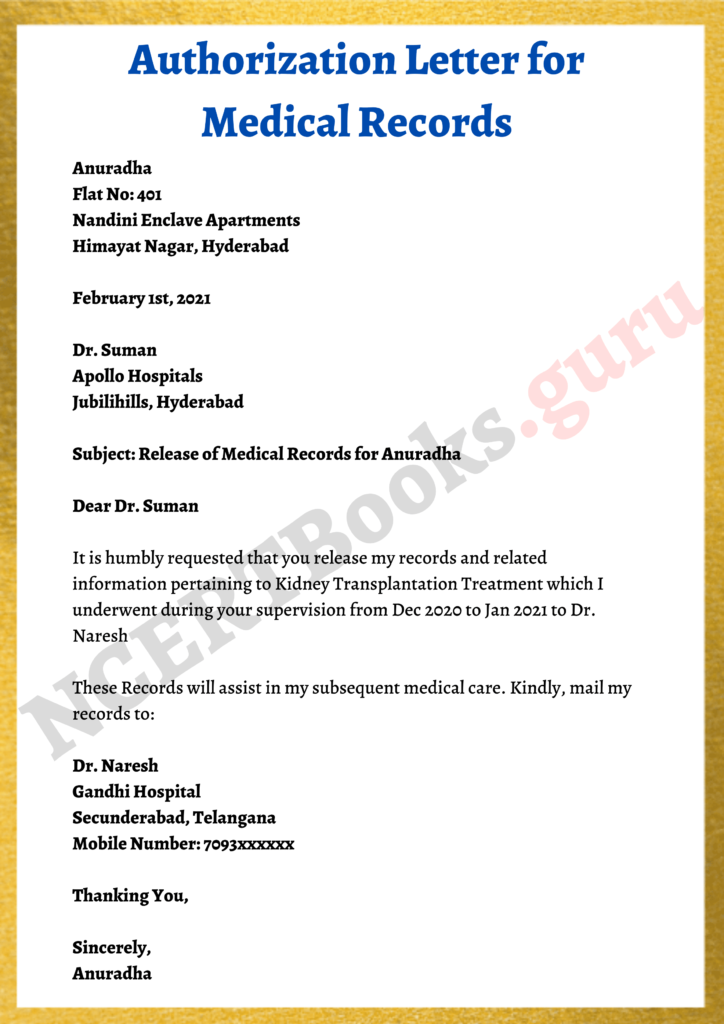
Authorization Letter Template, Samples How to write an Authorization
What Is Retro Authorization In Medical Billing Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Obtained during an ongoing treatment, often for extended. Obtained before the service is provided. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services.
From ircm.com
Optimizing Retro Authorization for Medical Billing Success What Is Retro Authorization In Medical Billing When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. It refers to obtaining approval for medical services. Obtained before the service is provided. Obtained during an ongoing treatment, often for extended. Retroactive authorization refers to requests made to the insurance company for approval after patient’s. What Is Retro Authorization In Medical Billing.
From www.ncertbooks.guru
Authorization Letter Template, Samples How to write an Authorization What Is Retro Authorization In Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Obtained during an ongoing treatment, often for extended. It refers to obtaining approval for medical services. Obtained before the service is provided. Retro authorization also known as retrospective authorization or retro auth is a crucial process. What Is Retro Authorization In Medical Billing.
From www.selecthub.com
Denial Codes in Medical Billing 2023 Comprehensive Guide What Is Retro Authorization In Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. It refers to obtaining approval for medical services. Retro authorization secures approval for medical services already rendered to a patient. Retro authorization is eligible in medical billing when a service that was already performed needs to. What Is Retro Authorization In Medical Billing.
From healthtoinsurance.com
Prior Authorization in Medical Billing Health to Insurance What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Obtained during an ongoing treatment, often for extended. Medical billing companies strive to assist doctors in minimizing. What Is Retro Authorization In Medical Billing.
From slidecourse.blogspot.com
What Is Pre Authorization In Medical Billing What Is Retro Authorization In Medical Billing Retro authorization secures approval for medical services already rendered to a patient. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retro authorization also known as. What Is Retro Authorization In Medical Billing.
From www.invensis.net
Importance of Preauthorization in Revenue Cycle Management (RCM) What Is Retro Authorization In Medical Billing Obtained before the service is provided. Retro authorization secures approval for medical services already rendered to a patient. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Obtained during an ongoing treatment, often for extended. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment. What Is Retro Authorization In Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF What Is Retro Authorization In Medical Billing When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Obtained during an ongoing treatment, often for extended. Obtained before the service. What Is Retro Authorization In Medical Billing.
From www.linkedin.com
Streamlining Healthcare Understanding Retro Authorization in Medical What Is Retro Authorization In Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retro authorization is eligible in medical billing when a service that was. What Is Retro Authorization In Medical Billing.
From umbsbillingservices.com
What Is Retro Authorization in Medical Billing? What Is Retro Authorization In Medical Billing Retro authorization secures approval for medical services already rendered to a patient. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. It refers to obtaining approval for medical services. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance. What Is Retro Authorization In Medical Billing.
From ircm.com
Optimizing Retro Authorization for Medical Billing Success What Is Retro Authorization In Medical Billing Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retro authorization also known as retrospective authorization or retro auth is a. What Is Retro Authorization In Medical Billing.
From www.carecloud.com
Complete Guide Prior Authorization in Medical Billing? What Is Retro Authorization In Medical Billing Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. When a claim is submitted to the payer and denied due to a. What Is Retro Authorization In Medical Billing.
From jqqwmseqmh.blogspot.com
RetroAuthorization Example Letter Printable retro authorization What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Obtained before the service is provided. Obtained during an ongoing treatment, often for extended. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Retro authorization is. What Is Retro Authorization In Medical Billing.
From rightmedicalbilling.com
Prior and Retro Authorization Services Right Medical Billing What Is Retro Authorization In Medical Billing Obtained during an ongoing treatment, often for extended. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization secures approval for medical services already rendered to a patient. Obtained before the service is provided. When a claim is submitted to the payer and denied due to a lack of. What Is Retro Authorization In Medical Billing.
From mwdn.com
TOP 13 things about medical billing and coding software you should know What Is Retro Authorization In Medical Billing It refers to obtaining approval for medical services. Obtained before the service is provided. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period. What Is Retro Authorization In Medical Billing.
From www.caplinehealthcaremanagement.com
What Is Meant By Retro Authorization In Medical Billing? What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Obtained during an ongoing treatment, often for extended. It refers to obtaining approval for medical services. Obtained before the service is provided. Retro authorization secures approval for medical services already rendered to a patient. Retroactive authorization refers to requests made to. What Is Retro Authorization In Medical Billing.
From moussyusa.com
Sample Medical Authorization Form Mous Syusa What Is Retro Authorization In Medical Billing It refers to obtaining approval for medical services. Obtained before the service is provided. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Retro authorization secures approval for medical services already rendered to a patient. Medical billing companies strive to assist doctors in minimizing claim. What Is Retro Authorization In Medical Billing.
From authorizationletter.org
Sample Authorization Letter for Medical Records Example What Is Retro Authorization In Medical Billing Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided. What Is Retro Authorization In Medical Billing.
From businesshobbie.com
Steps Involved In The Medical Billing Process Business Hobbie What Is Retro Authorization In Medical Billing Obtained before the service is provided. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Medical billing companies strive to assist doctors in minimizing claim rejections. What Is Retro Authorization In Medical Billing.
From www.ucontrolbilling.com
Best Authorization In Medical Billing UControl Billing What Is Retro Authorization In Medical Billing Retro authorization secures approval for medical services already rendered to a patient. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Medical. What Is Retro Authorization In Medical Billing.
From umbsbillingservices.com
What Is Retro Authorization in Medical Billing? What Is Retro Authorization In Medical Billing When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing. What Is Retro Authorization In Medical Billing.
From dokumen.tips
(PDF) Retro Authorization Process (*Internal Use Only*) DOKUMEN.TIPS What Is Retro Authorization In Medical Billing It refers to obtaining approval for medical services. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Obtained before the service is. What Is Retro Authorization In Medical Billing.
From www.vrogue.co
What Is Pre Authorization In Medical Billing vrogue.co What Is Retro Authorization In Medical Billing Retro authorization secures approval for medical services already rendered to a patient. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. It refers to obtaining approval for medical services. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective. What Is Retro Authorization In Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF What Is Retro Authorization In Medical Billing It refers to obtaining approval for medical services. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Medical billing companies strive to assist doctors in minimizing. What Is Retro Authorization In Medical Billing.
From www.dexform.com
Medical Authorization Form download free documents for PDF, Word and What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Obtained before the service is provided. Retro authorization secures approval for medical services already rendered to a patient. Obtained during an ongoing treatment, often for extended. When a claim is submitted to the payer and denied due to a lack of. What Is Retro Authorization In Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF What Is Retro Authorization In Medical Billing Obtained before the service is provided. Obtained during an ongoing treatment, often for extended. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Retro authorization secures approval for medical services already rendered to a patient. It refers to obtaining approval for medical services. Retroactive authorization refers to requests made to. What Is Retro Authorization In Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF What Is Retro Authorization In Medical Billing Obtained before the service is provided. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retro authorization secures approval for medical services. What Is Retro Authorization In Medical Billing.
From precisebs.com
Importance of Authorization in Medical Billing Precisebs What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. It refers to obtaining approval for medical services. Retroactive authorization refers to requests made to the insurance company for approval after patient’s. What Is Retro Authorization In Medical Billing.
From www.slideserve.com
PPT Role of Prior Authorization in Medical Billing PowerPoint What Is Retro Authorization In Medical Billing When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. It refers to obtaining approval for medical services. Obtained before the service is provided. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is. What Is Retro Authorization In Medical Billing.
From www.examples.com
Medical Authorization Letter 9+ Examples, Format, How to Write, PDF What Is Retro Authorization In Medical Billing Obtained before the service is provided. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. It refers to obtaining approval for medical services. Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Obtained during an. What Is Retro Authorization In Medical Billing.
From www.caplinedentalservices.com
What is authorization in medical billing? Capline Dental Sservices What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Obtained before the service is provided. Retroactive authorization refers to requests made to the insurance company for approval. What Is Retro Authorization In Medical Billing.
From www.caplinehealthcaremanagement.com
What is Preauthorization in Medical Billing What Is Retro Authorization In Medical Billing Obtained before the service is provided. Obtained during an ongoing treatment, often for extended. Retroactive authorization refers to requests made to the insurance company for approval after patient’s treatment has been provided and the specified period of time. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by. What Is Retro Authorization In Medical Billing.
From www.upwork.com
Prior Authorization and Retro Authorization Services Upwork What Is Retro Authorization In Medical Billing Retro authorization also known as retrospective authorization or retro auth is a crucial process in the medical billing world. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods. What Is Retro Authorization In Medical Billing.
From www.outsourcestrategies.com
Retro Authorization in Medical Billing What Is Retro Authorization In Medical Billing When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. Obtained during an ongoing treatment, often for extended. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Retroactive authorization refers to requests made to the insurance. What Is Retro Authorization In Medical Billing.
From medicalbillingrcm.com
What is Pre Authorization in Medical Billing? What Is Retro Authorization In Medical Billing Retro authorization secures approval for medical services already rendered to a patient. Medical billing companies strive to assist doctors in minimizing claim rejections and enhancing patient satisfaction through effective methods like. Retro authorization is eligible in medical billing when a service that was already performed needs to be reviewed by the insurance company to. Retroactive authorization refers to requests made. What Is Retro Authorization In Medical Billing.
From www.caplinehealthcaremanagement.com
What is Authorization in Medical Billing What Is Retro Authorization In Medical Billing Retro authorization secures approval for medical services already rendered to a patient. When a claim is submitted to the payer and denied due to a lack of prior authorization, retro authorization is initiated by the healthcare. It refers to obtaining approval for medical services. Obtained before the service is provided. Medical billing companies strive to assist doctors in minimizing claim. What Is Retro Authorization In Medical Billing.