What Does No Pre Authorization Mean . This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. The following are five steps to take when your claims are denied for no authorization. It’s a restriction put in place to determine whether or not they will pay for certain. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. Prior authorization is an approval of coverage from your insurance company, not your doctor. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Best practices for reducing claims denied for. Prior authorization is the approval from your health insurance that may be required for a service,.
from www.planforms.net
Best practices for reducing claims denied for. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Prior authorization is the approval from your health insurance that may be required for a service,. It’s a restriction put in place to determine whether or not they will pay for certain. The following are five steps to take when your claims are denied for no authorization. Prior authorization is an approval of coverage from your insurance company, not your doctor. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization.
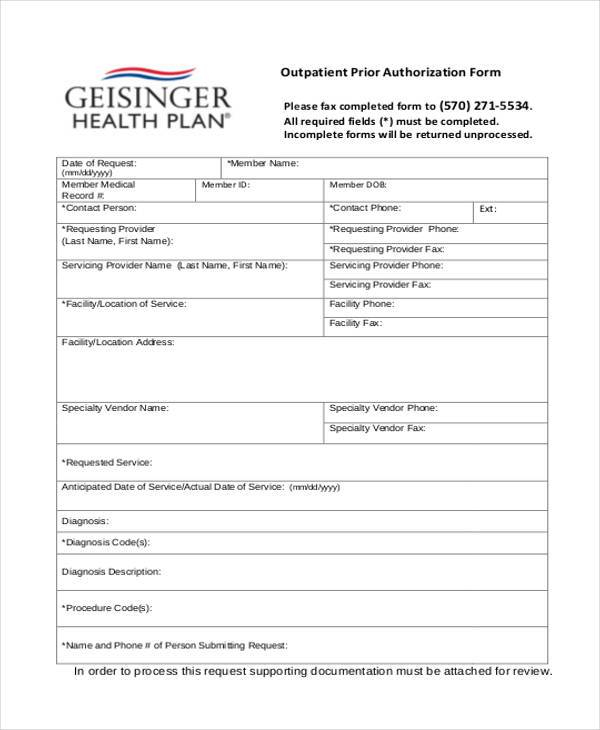
Completing The GHP Prior Authorization Request Form Geisinger
What Does No Pre Authorization Mean It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is the approval from your health insurance that may be required for a service,. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Prior authorization is an approval of coverage from your insurance company, not your doctor. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. The following are five steps to take when your claims are denied for no authorization. Best practices for reducing claims denied for. It’s a restriction put in place to determine whether or not they will pay for certain.
From mxlape.blogspot.com
Sample Forms For Authorized Drivers Download Sample Credit Card What Does No Pre Authorization Mean Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. This approval process is called prior authorization, and. What Does No Pre Authorization Mean.
From dxofxtrfm.blob.core.windows.net
What Does Purchase Authorization Mean at Clayton Henry blog What Does No Pre Authorization Mean Prior authorization is the approval from your health insurance that may be required for a service,. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. The following are five steps to take when your claims are denied for no authorization. Prior authorization is. What Does No Pre Authorization Mean.
From formspal.com
Member Authorization Form ≡ Fill Out Printable PDF Forms Online What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Prior authorization is the approval from your health insurance that may be required for a service,. Prior authorization is an approval of coverage from your insurance company, not your doctor. This approval process is. What Does No Pre Authorization Mean.
From www.youtube.com
Authorization Meaning YouTube What Does No Pre Authorization Mean Prior authorization is an approval of coverage from your insurance company, not your doctor. Prior authorization is the approval from your health insurance that may be required for a service,. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Patients may wait days, weeks. What Does No Pre Authorization Mean.
From sunknowledge.com
What Does Prior Authorization Mean for Medication? What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. It’s a restriction put in place to determine whether or not they will pay for certain. Best practices for reducing claims denied for. Patients may wait days, weeks or even months for a necessary. What Does No Pre Authorization Mean.
From fitsmallbusiness.com
What Is a Credit Card Authorization Form? (+ Free Templates) What Does No Pre Authorization Mean The following are five steps to take when your claims are denied for no authorization. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Best practices for reducing claims denied for. Prior authorization is the approval from your health insurance that may be required. What Does No Pre Authorization Mean.
From www.auth-net.com
Is it Time to Call a Healthcare PreAuthorization Service Learn More What Does No Pre Authorization Mean The following are five steps to take when your claims are denied for no authorization. Best practices for reducing claims denied for. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Prior authorization is an approval of coverage from your insurance company, not. What Does No Pre Authorization Mean.
From practolytics.com
Analyzing Prior Authorization in Healthcare Insurance What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance. What Does No Pre Authorization Mean.
From templatelab.com
46 Authorization Letter Samples & Templates ᐅ TemplateLab What Does No Pre Authorization Mean Prior authorization is an approval of coverage from your insurance company, not your doctor. Best practices for reducing claims denied for. Prior authorization is the approval from your health insurance that may be required for a service,. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first. What Does No Pre Authorization Mean.
From portiva.com
What does Prior Authorization mean for Prescriptions? What Does No Pre Authorization Mean It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is the approval from your health insurance that may be required for a service,. The following are five steps to take when your claims are denied for no authorization. This approval process is called prior authorization, and getting one before you get. What Does No Pre Authorization Mean.
From authorizationletter.org
Authorization Letter What Does No Pre Authorization Mean Prior authorization is an approval of coverage from your insurance company, not your doctor. Prior authorization is the approval from your health insurance that may be required for a service,. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Patients may wait days, weeks. What Does No Pre Authorization Mean.
From www.planforms.net
Completing The GHP Prior Authorization Request Form Geisinger What Does No Pre Authorization Mean Prior authorization is an approval of coverage from your insurance company, not your doctor. Best practices for reducing claims denied for. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for. What Does No Pre Authorization Mean.
From fabalabse.com
What is a credit card authorization? Leia aqui Is a credit card What Does No Pre Authorization Mean Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. It’s a restriction put in place to determine whether or not they will pay for certain. This approval process is called prior authorization, and getting one before you get care means the care is. What Does No Pre Authorization Mean.
From www.templateroller.com
Sample Insurance Appeal Letter for No Authorization Download Printable What Does No Pre Authorization Mean The following are five steps to take when your claims are denied for no authorization. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is. What Does No Pre Authorization Mean.
From ebizcharge.com
What are Pre Authorization Charges? Your Key to Financial Security What Does No Pre Authorization Mean Best practices for reducing claims denied for. It’s a restriction put in place to determine whether or not they will pay for certain. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. The following are five steps to take when your claims are. What Does No Pre Authorization Mean.
From www.vrogue.co
用keepass管理密码并用synology Drive或者goodsync实时双向同步电脑桌面和群晖nas2021年8月5日 What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. The following are five steps to take when your claims are denied for no authorization. This approval process is called prior authorization, and getting one before you get care means the care is appropriate. What Does No Pre Authorization Mean.
From www.psychiatryatlanta.com
What is Prior Authorization? Some Mysteries Explained Atlanta What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. This approval process is called prior authorization, and. What Does No Pre Authorization Mean.
From www.hrrmc.com
Insurance Prior Authorization Timeframes Medical Center in Salida What Does No Pre Authorization Mean The following are five steps to take when your claims are denied for no authorization. Prior authorization is the approval from your health insurance that may be required for a service,. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. This approval process. What Does No Pre Authorization Mean.
From www.authorizationform.net
Medicaid Pre Authorization Form What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. The following are five steps to take when your claims are denied for no authorization. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because. What Does No Pre Authorization Mean.
From www.healthcare.com
Here's What’s Wrong with Prior Authorization for Medication What Does No Pre Authorization Mean Best practices for reducing claims denied for. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Prior authorization is an approval of coverage from your insurance company, not your doctor. Prior authorization is the approval from your health insurance that may be required. What Does No Pre Authorization Mean.
From portiva.com
What does getting Prior Authorization mean? Doc's Clear Way What Does No Pre Authorization Mean Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. The following are five steps to take when your claims are denied for no authorization. Prior authorization is an approval of coverage from your insurance company, not your doctor. This approval process is called. What Does No Pre Authorization Mean.
From q1medicare.com
What is a Prior Authorization in Medicare Part D? What Does No Pre Authorization Mean It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Best practices for reducing claims denied for. Patients may wait days, weeks or even months for a necessary. What Does No Pre Authorization Mean.
From www.reddit.com
"What do you mean it needs Prior Authorization? My doctor already What Does No Pre Authorization Mean This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for a service,. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because. What Does No Pre Authorization Mean.
From www.triagehealth.org
PreAuthorizations for Individual & EmployerSponsored Health Insurance What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Best practices for reducing claims denied for. It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is an approval of coverage from your insurance company,. What Does No Pre Authorization Mean.
From studylib.net
SAMPLE {Letter must be on letterhead with original signature of What Does No Pre Authorization Mean Prior authorization is the approval from your health insurance that may be required for a service,. It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is an approval of coverage from your insurance company, not your doctor. Patients may wait days, weeks or even months for a necessary test or medical. What Does No Pre Authorization Mean.
From mavink.com
No Authorization Appeal Letter What Does No Pre Authorization Mean This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Prior authorization is the approval from your health insurance that may be required for a service,. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because. What Does No Pre Authorization Mean.
From behavehealth.com
Doing a PreCertification or Prior Authorization with Molina HealthCare What Does No Pre Authorization Mean Prior authorization is an approval of coverage from your insurance company, not your doctor. Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. It’s a restriction put in place to determine whether or not they will pay for certain. Prior authorization is the. What Does No Pre Authorization Mean.
From simpleartifact.com
Authorization For Medical Treatment Letter Collection Letter Template What Does No Pre Authorization Mean Best practices for reducing claims denied for. The following are five steps to take when your claims are denied for no authorization. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Patients may wait days, weeks or even months for a necessary test or. What Does No Pre Authorization Mean.
From staffingly.com
PRIOR AUTHORIZATION PROCESS Staffingly, Inc What Does No Pre Authorization Mean It’s a restriction put in place to determine whether or not they will pay for certain. Best practices for reducing claims denied for. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Patients may wait days, weeks or even months for a necessary test. What Does No Pre Authorization Mean.
From bestlettertemplate.com
21+ Free Authorization Letter Sample Template & Examples What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. It’s a restriction put in place to determine. What Does No Pre Authorization Mean.
From simpleartifact.com
Authorization Letter To Represent On Behalf Of Company Collection What Does No Pre Authorization Mean Prior authorization is the approval from your health insurance that may be required for a service,. This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. The following are five steps to take when your claims are denied for no authorization. Patients may wait days,. What Does No Pre Authorization Mean.
From medicare-faqs.com
What Does The Letter After A Medicare Number Mean What Does No Pre Authorization Mean This approval process is called prior authorization, and getting one before you get care means the care is appropriate and can be covered by your. Best practices for reducing claims denied for. It’s a restriction put in place to determine whether or not they will pay for certain. The following are five steps to take when your claims are denied. What Does No Pre Authorization Mean.
From communities.efi.com
Configuring preauthorization amounts for Windcave What Does No Pre Authorization Mean Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed. It’s a restriction put in place to determine whether or not they will pay for certain. Best practices for reducing claims denied for. Prior authorization is an approval of coverage from your insurance company,. What Does No Pre Authorization Mean.
From mymagesvertical.blogspot.com
What Does Debit Card Preauth Hold Mean MymagesVertical What Does No Pre Authorization Mean Prior authorization is the approval from your health insurance that may be required for a service,. It’s a restriction put in place to determine whether or not they will pay for certain. Patients may wait days, weeks or even months for a necessary test or medical procedure to be scheduled because physicians need to first obtain similar authorization. Prior authorization. What Does No Pre Authorization Mean.
From www.pdfprof.com
PDF pxn denial code PDF Télécharger Download What Does No Pre Authorization Mean The following are five steps to take when your claims are denied for no authorization. Prior authorization is the approval from your health insurance that may be required for a service,. It’s a restriction put in place to determine whether or not they will pay for certain. Best practices for reducing claims denied for. Prior authorization is a process required. What Does No Pre Authorization Mean.