Soaps Chart Example . They contain four primary sections, represented by its acronym: But knowing how to create an easy to read note is harder than it looks! Tips for clear and concise documentation. In the soap format, soap stands for subjective, objective, assessment, and plan. Use clear, specific language to avoid ambiguity. Soap nursing notes are a type of patient progress note or nurse’s note. This guides healthcare practitioners to systematically record. Follow the soap structure strictly to ensure all. It is the documentation used to record information about encounters with patients that follows a specific format. We will go through some tips for creating a soap. Soap chart templates provide predefined sections for each component of the soap framework. Each letter refers to one of four sections in the document. The soap note format creates a systematic, easy to follow chart note. Soap notes are a specific format for writing progress notes as a behavioral health clinician.
from ar.inspiredpencil.com
They contain four primary sections, represented by its acronym: It is the documentation used to record information about encounters with patients that follows a specific format. But knowing how to create an easy to read note is harder than it looks! Soap nursing notes are a type of patient progress note or nurse’s note. Each letter refers to one of four sections in the document. Soap chart templates provide predefined sections for each component of the soap framework. In the soap format, soap stands for subjective, objective, assessment, and plan. Follow the soap structure strictly to ensure all. We will go through some tips for creating a soap. This guides healthcare practitioners to systematically record.
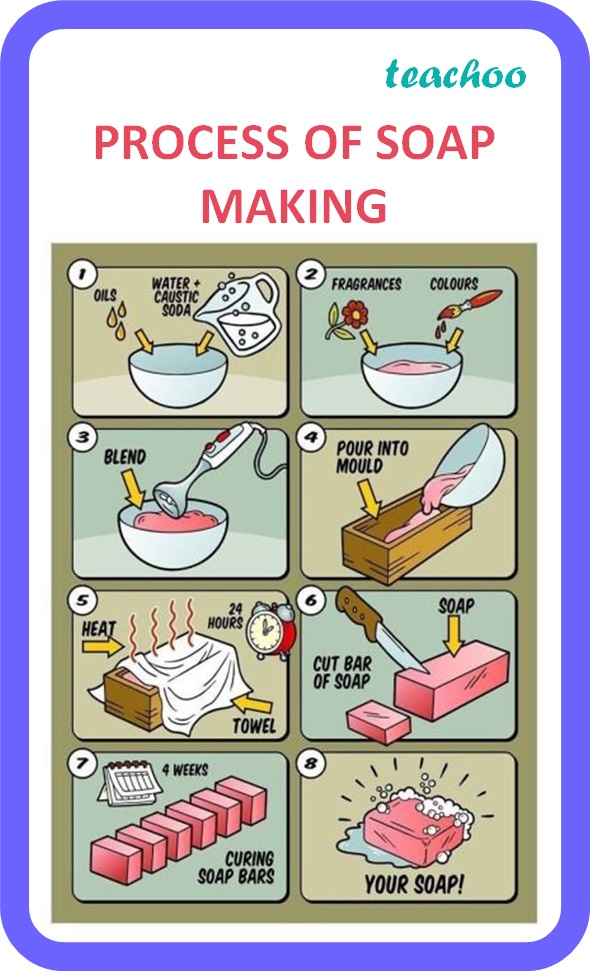
Preparation Of Soap In Chemistry Project
Soaps Chart Example It is the documentation used to record information about encounters with patients that follows a specific format. Use clear, specific language to avoid ambiguity. We will go through some tips for creating a soap. In the soap format, soap stands for subjective, objective, assessment, and plan. But knowing how to create an easy to read note is harder than it looks! Soap nursing notes are a type of patient progress note or nurse’s note. Tips for clear and concise documentation. Each letter refers to one of four sections in the document. The soap note format creates a systematic, easy to follow chart note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap chart templates provide predefined sections for each component of the soap framework. This guides healthcare practitioners to systematically record. Follow the soap structure strictly to ensure all. It is the documentation used to record information about encounters with patients that follows a specific format. They contain four primary sections, represented by its acronym:
From covenantlifecog.com
SOAPmethodposter Soaps Chart Example This guides healthcare practitioners to systematically record. Soap chart templates provide predefined sections for each component of the soap framework. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. Follow the soap structure strictly to ensure all. Use clear, specific language to avoid ambiguity. Soap nursing. Soaps Chart Example.
From ar.inspiredpencil.com
Chart Note Format Soaps Chart Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. We will go through some tips for creating a soap. Soap chart templates provide predefined sections for each component of the soap framework. Soap nursing notes are a type of patient progress note or nurse’s note. Follow the soap structure strictly to ensure all. They. Soaps Chart Example.
From www.scilynk.in
What is the Quality of your Soap? SciLynk Soaps Chart Example Use clear, specific language to avoid ambiguity. Soap chart templates provide predefined sections for each component of the soap framework. Each letter refers to one of four sections in the document. We will go through some tips for creating a soap. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for. Soaps Chart Example.
From www.dreamstime.com
1,973 Computer Bubbles Stock Photos Free & RoyaltyFree Stock Photos Soaps Chart Example Follow the soap structure strictly to ensure all. But knowing how to create an easy to read note is harder than it looks! Tips for clear and concise documentation. Soap nursing notes are a type of patient progress note or nurse’s note. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note format creates a. Soaps Chart Example.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soaps Chart Example But knowing how to create an easy to read note is harder than it looks! This guides healthcare practitioners to systematically record. Soap chart templates provide predefined sections for each component of the soap framework. Follow the soap structure strictly to ensure all. Tips for clear and concise documentation. Soap nursing notes are a type of patient progress note or. Soaps Chart Example.
From clinicsense.com
ClinicSense SOAP Note Template For Massage Therapists Soaps Chart Example We will go through some tips for creating a soap. This guides healthcare practitioners to systematically record. They contain four primary sections, represented by its acronym: Soap chart templates provide predefined sections for each component of the soap framework. But knowing how to create an easy to read note is harder than it looks! It is the documentation used to. Soaps Chart Example.
From www.powerdiary.com
What’s the Difference SOAP Notes vs DAP Notes Power Diary Soaps Chart Example It is the documentation used to record information about encounters with patients that follows a specific format. The soap note format creates a systematic, easy to follow chart note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap chart templates provide predefined sections for each component of the soap framework. We will go. Soaps Chart Example.
From help.craftybase.com
Soapmaking Manufacture Workflow Examples Craftybase Knowledge Base Soaps Chart Example Tips for clear and concise documentation. Soap chart templates provide predefined sections for each component of the soap framework. Soap notes are a specific format for writing progress notes as a behavioral health clinician. We will go through some tips for creating a soap. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note format. Soaps Chart Example.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soaps Chart Example The soap note format creates a systematic, easy to follow chart note. Follow the soap structure strictly to ensure all. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap chart templates provide predefined sections for each component of the soap framework. Use clear, specific language to avoid ambiguity. This guides healthcare practitioners to. Soaps Chart Example.
From www.slideshare.net
Making Soap Chart of Oils Properties A Guide for Making your own Soaps Chart Example The soap note format creates a systematic, easy to follow chart note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. It is the documentation used to record information about encounters with patients that follows a specific format. Soap nursing notes are a type of patient progress note or nurse’s note. Each letter refers. Soaps Chart Example.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soaps Chart Example Follow the soap structure strictly to ensure all. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Use clear, specific language to avoid ambiguity. But knowing how to create an easy to read note is harder than it looks! Each letter refers to one of four sections in the document. Tips for clear and. Soaps Chart Example.
From fyoqjvbid.blob.core.windows.net
Soap Note Example Diabetes at Amanda Fleming blog Soaps Chart Example Each letter refers to one of four sections in the document. But knowing how to create an easy to read note is harder than it looks! Soap nursing notes are a type of patient progress note or nurse’s note. Soap chart templates provide predefined sections for each component of the soap framework. Use clear, specific language to avoid ambiguity. We. Soaps Chart Example.
From ar.inspiredpencil.com
Soap Chart Template Soaps Chart Example Soap chart templates provide predefined sections for each component of the soap framework. Follow the soap structure strictly to ensure all. Each letter refers to one of four sections in the document. Use clear, specific language to avoid ambiguity. But knowing how to create an easy to read note is harder than it looks! The soap note format creates a. Soaps Chart Example.
From quizzmediasophie.z13.web.core.windows.net
The E Entry In The Soaper Charting Method Means Soaps Chart Example This guides healthcare practitioners to systematically record. Soap nursing notes are a type of patient progress note or nurse’s note. Each letter refers to one of four sections in the document. But knowing how to create an easy to read note is harder than it looks! Follow the soap structure strictly to ensure all. The soap note format creates a. Soaps Chart Example.
From www.pinterest.com
In My Soap Pot SAP Chart Handmade Soap Packaging, Handmade Soap Recipes Soaps Chart Example Follow the soap structure strictly to ensure all. We will go through some tips for creating a soap. This guides healthcare practitioners to systematically record. Use clear, specific language to avoid ambiguity. Soap chart templates provide predefined sections for each component of the soap framework. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers. Soaps Chart Example.
From ar.inspiredpencil.com
Soap Chart Template Soaps Chart Example Soap chart templates provide predefined sections for each component of the soap framework. Use clear, specific language to avoid ambiguity. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. It is the documentation used to record information about encounters with patients that follows a specific format.. Soaps Chart Example.
From ar.inspiredpencil.com
Chart Note Format Soaps Chart Example Each letter refers to one of four sections in the document. Tips for clear and concise documentation. Follow the soap structure strictly to ensure all. Soap chart templates provide predefined sections for each component of the soap framework. In the soap format, soap stands for subjective, objective, assessment, and plan. But knowing how to create an easy to read note. Soaps Chart Example.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soaps Chart Example Use clear, specific language to avoid ambiguity. They contain four primary sections, represented by its acronym: Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap chart templates provide predefined sections for each component of the soap framework. It is the documentation used to record information about encounters with patients that follows a specific. Soaps Chart Example.
From ar.inspiredpencil.com
Preparation Of Soap In Chemistry Project Soaps Chart Example They contain four primary sections, represented by its acronym: The soap note format creates a systematic, easy to follow chart note. Tips for clear and concise documentation. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap nursing notes are a type of patient progress note. Soaps Chart Example.
From erinmarie.yolasite.com
APWH Soaps Chart Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. Use clear, specific language to avoid ambiguity. Soap nursing notes are a type of patient progress note or nurse’s note. Soap chart templates provide predefined sections for each component of the soap framework. Tips for clear and concise documentation. The soap note format creates a. Soaps Chart Example.
From www.pinterest.com
With the this Qualities of Oils for Soap Making chart, we break down Soaps Chart Example The soap note format creates a systematic, easy to follow chart note. Soap nursing notes are a type of patient progress note or nurse’s note. We will go through some tips for creating a soap. Use clear, specific language to avoid ambiguity. Each letter refers to one of four sections in the document. Soap notes are a specific format for. Soaps Chart Example.
From thevisualcommunicationguy.com
SOAPStone Strategy for Written Analysis The Visual Communication Guy Soaps Chart Example Follow the soap structure strictly to ensure all. But knowing how to create an easy to read note is harder than it looks! Soap nursing notes are a type of patient progress note or nurse’s note. Tips for clear and concise documentation. Soap chart templates provide predefined sections for each component of the soap framework. In the soap format, soap. Soaps Chart Example.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Nutrition Soaps Chart Example Soap chart templates provide predefined sections for each component of the soap framework. It is the documentation used to record information about encounters with patients that follows a specific format. Tips for clear and concise documentation. This guides healthcare practitioners to systematically record. Use clear, specific language to avoid ambiguity. Soap notes are a specific format for writing progress notes. Soaps Chart Example.
From www.pinterest.com
Soap Saponification Charts & Information Natural Health Soapmaking Soaps Chart Example The soap note format creates a systematic, easy to follow chart note. This guides healthcare practitioners to systematically record. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Tips. Soaps Chart Example.
From www.pinterest.com
The terrific Free Massage Soap Notes Forms Massagebook For Soap Soaps Chart Example Use clear, specific language to avoid ambiguity. The soap note format creates a systematic, easy to follow chart note. Tips for clear and concise documentation. But knowing how to create an easy to read note is harder than it looks! Soap nursing notes are a type of patient progress note or nurse’s note. They contain four primary sections, represented by. Soaps Chart Example.
From www.yourbestdigs.com
The Best Dish Soaps of 2021 Reviews by Your Best Digs Soaps Chart Example Tips for clear and concise documentation. Follow the soap structure strictly to ensure all. Soap nursing notes are a type of patient progress note or nurse’s note. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Soap chart templates provide predefined sections for each component of the soap framework. The soap note format creates. Soaps Chart Example.
From theorg.com
Adam Fulep Vice President Of Transformation & Strategy at The Soaps Chart Example Soap nursing notes are a type of patient progress note or nurse’s note. Use clear, specific language to avoid ambiguity. In the soap format, soap stands for subjective, objective, assessment, and plan. They contain four primary sections, represented by its acronym: We will go through some tips for creating a soap. Tips for clear and concise documentation. But knowing how. Soaps Chart Example.
From www.carepatron.com
Soap Chart & Example Free PDF Download Soaps Chart Example We will go through some tips for creating a soap. Soap chart templates provide predefined sections for each component of the soap framework. But knowing how to create an easy to read note is harder than it looks! It is the documentation used to record information about encounters with patients that follows a specific format. This guides healthcare practitioners to. Soaps Chart Example.
From www.pinterest.com
Natural Soap Colorants Chart and Ebooks Offer Soaps Chart Example Soap notes are a specific format for writing progress notes as a behavioral health clinician. But knowing how to create an easy to read note is harder than it looks! Each letter refers to one of four sections in the document. Soap nursing notes are a type of patient progress note or nurse’s note. Tips for clear and concise documentation.. Soaps Chart Example.
From ar.inspiredpencil.com
Chart Note Format Soaps Chart Example Follow the soap structure strictly to ensure all. This guides healthcare practitioners to systematically record. We will go through some tips for creating a soap. Soap nursing notes are a type of patient progress note or nurse’s note. Tips for clear and concise documentation. Soap chart templates provide predefined sections for each component of the soap framework. But knowing how. Soaps Chart Example.
From www.pinterest.com
Making Soap Chart of Oils Properties A Guide for Making your own Soaps Chart Example We will go through some tips for creating a soap. Use clear, specific language to avoid ambiguity. The soap note format creates a systematic, easy to follow chart note. Tips for clear and concise documentation. Each letter refers to one of four sections in the document. Soap chart templates provide predefined sections for each component of the soap framework. In. Soaps Chart Example.
From zolmi.com
How To Write Massage Therapy Soap Notes in 2024 Examples Soaps Chart Example Each letter refers to one of four sections in the document. Follow the soap structure strictly to ensure all. They contain four primary sections, represented by its acronym: Soap chart templates provide predefined sections for each component of the soap framework. This guides healthcare practitioners to systematically record. Tips for clear and concise documentation. Soap nursing notes are a type. Soaps Chart Example.
From samanthapatterson.z19.web.core.windows.net
Soap Chart Note Is An Acronym For Soaps Chart Example Use clear, specific language to avoid ambiguity. Follow the soap structure strictly to ensure all. We will go through some tips for creating a soap. Soap chart templates provide predefined sections for each component of the soap framework. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note format creates a systematic, easy to follow. Soaps Chart Example.
From co.pinterest.com
Pin de 777 en BIRTH CHART en 2024 Soaps Chart Example In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a specific format for writing progress notes as a behavioral health clinician. Follow the soap structure strictly to ensure all. It is the documentation used to record information about encounters with patients that follows a specific format. The soap note format creates a systematic, easy. Soaps Chart Example.
From premiercontinuingeducation.com
Documenting with SOAP Notes (2 CEs) Premier Continuing Education Soaps Chart Example It is the documentation used to record information about encounters with patients that follows a specific format. Follow the soap structure strictly to ensure all. They contain four primary sections, represented by its acronym: We will go through some tips for creating a soap. In the soap format, soap stands for subjective, objective, assessment, and plan. The soap note format. Soaps Chart Example.