Soap Note Example Np . — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. It is the documentation used to record information about encounters with patients. We will break down each component of a soap note and explain how to write a soap note. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment, and plan. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap notes are essential for effective patient care and documentation in nurse practitioner practice. there are four basic components of a soap note: soap nursing notes are a type of patient progress note or nurse’s note. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation.
from www.studocu.com
— if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. there are four basic components of a soap note: A soap note is standard across all types of chart notes and can be used in any area of healthcare. It is the documentation used to record information about encounters with patients. Subjective, objective, assessment, and plan. soap nursing notes are a type of patient progress note or nurse’s note. soap notes are essential for effective patient care and documentation in nurse practitioner practice. We will break down each component of a soap note and explain how to write a soap note.
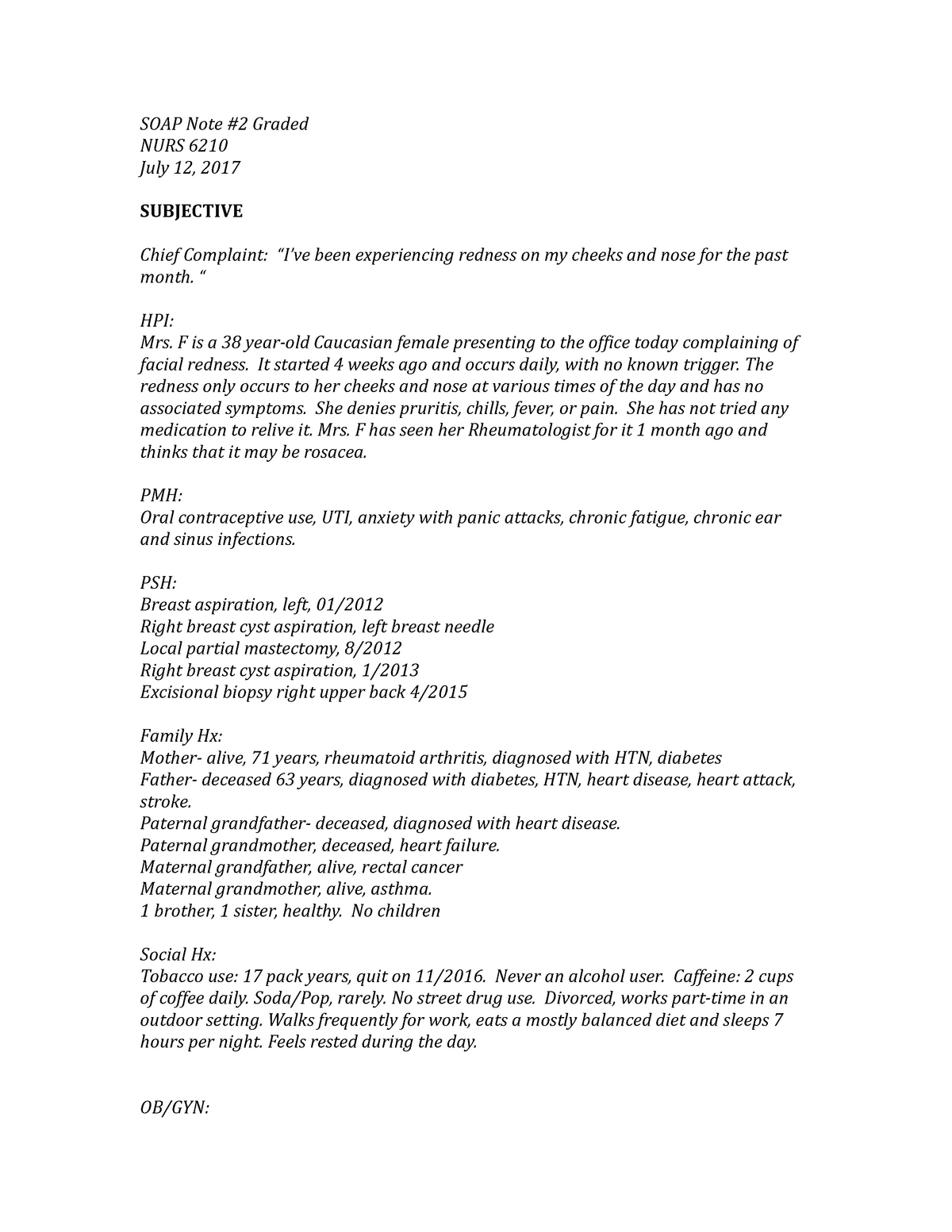
SOAP Note 2 Graded.docx Sample SOAP Note 2 Graded NURS 6210 July 12
Soap Note Example Np — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap notes are essential for effective patient care and documentation in nurse practitioner practice. We will break down each component of a soap note and explain how to write a soap note. It is the documentation used to record information about encounters with patients. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap nursing notes are a type of patient progress note or nurse’s note. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. Subjective, objective, assessment, and plan. A soap note is standard across all types of chart notes and can be used in any area of healthcare. there are four basic components of a soap note: save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation.
From www.pinterest.com
Soap Note Template Nurse Practitioner Lovely What is A soap Note Soap Soap Note Example Np soap notes are essential for effective patient care and documentation in nurse practitioner practice. We will break down each component of a soap note and explain how to write a soap note. A soap note is standard across all types of chart notes and can be used in any area of healthcare. soap nursing notes are a type. Soap Note Example Np.
From www.pinterest.ca
an image of a computer user's profile page Soap Note Example Np — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap notes are essential for effective patient care and documentation in nurse practitioner practice. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Subjective, objective, assessment,. Soap Note Example Np.
From www.etsy.com
SOAP Note Template for Nps/pas/mds // NP Students // NP School Help Etsy Soap Note Example Np It is the documentation used to record information about encounters with patients. soap notes are essential for effective patient care and documentation in nurse practitioner practice. soap nursing notes are a type of patient progress note or nurse’s note. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of. Soap Note Example Np.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Note Example Np — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. Subjective, objective, assessment, and plan. soap nursing notes are a type of patient progress note or nurse’s note. soap notes are essential for effective patient care and documentation in nurse practitioner practice. It is the documentation. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Example Np soap nursing notes are a type of patient progress note or nurse’s note. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. It is the documentation used to record information about encounters with patients. Subjective, objective, assessment, and plan. soap notes are essential for effective. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. A soap note is standard across all types of chart notes and can be used in any area of healthcare. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information about encounters with patients. Subjective, objective, assessment, and plan. — the subjective, objective, assessment and. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np soap notes are essential for effective patient care and documentation in nurse practitioner practice. We will break down each component of a soap note and explain how to write a soap note. soap nursing notes are a type of patient progress note or nurse’s note. A soap note is standard across all types of chart notes and can. Soap Note Example Np.
From soapnoteai.com
SOAP Note AI Generate HIPAA Compliant, Fast, Efficient, AIAssisted Soap Note Example Np save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. soap nursing notes are a type of patient progress note or nurse’s note. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care.. Soap Note Example Np.
From templates.rjuuc.edu.np
Np Soap Note Template Soap Note Example Np We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. A soap note is standard across all types of chart notes and can be used in any area of healthcare. soap notes are essential for effective patient care and documentation in nurse practitioner practice. save. Soap Note Example Np.
From www.sampletemplates.com
FREE 15+ SOAP Note Templates in PDF MS Word Soap Note Example Np soap nursing notes are a type of patient progress note or nurse’s note. We will break down each component of a soap note and explain how to write a soap note. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment, and plan. there are. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Example Np We will break down each component of a soap note and explain how to write a soap note. soap nursing notes are a type of patient progress note or nurse’s note. Subjective, objective, assessment, and plan. It is the documentation used to record information about encounters with patients. A soap note is standard across all types of chart notes. Soap Note Example Np.
From www.template.net
FREE SOAP Note Templates Templates & Examples Edit Online & Download Soap Note Example Np there are four basic components of a soap note: — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. soap notes are essential for. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. It is the documentation used to record information about encounters with patients. We will break down each component of a soap note and explain how to write a soap note. Subjective, objective, assessment, and plan. — if you’re a. Soap Note Example Np.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Note Example Np there are four basic components of a soap note: A soap note is standard across all types of chart notes and can be used in any area of healthcare. We will break down each component of a soap note and explain how to write a soap note. — the subjective, objective, assessment and plan (soap) note is an. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np It is the documentation used to record information about encounters with patients. We will break down each component of a soap note and explain how to write a soap note. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. there are four basic components. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np soap notes are essential for effective patient care and documentation in nurse practitioner practice. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment, and plan.. Soap Note Example Np.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Note Example Np We will break down each component of a soap note and explain how to write a soap note. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. It is the documentation used to record information about encounters with patients. — if you’re a nurse practitioner, then you know. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. A soap note is standard across all types of chart notes and can be used in any area of healthcare. soap nursing notes are a type of patient progress note or nurse’s note. soap notes are essential for. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np We will break down each component of a soap note and explain how to write a soap note. soap notes are essential for effective patient care and documentation in nurse practitioner practice. It is the documentation used to record information about encounters with patients. save time with this downloadable soap notes template for nursing, which is guaranteed to. Soap Note Example Np.
From data1.skinnyms.com
Np Soap Note Template Soap Note Example Np Subjective, objective, assessment, and plan. It is the documentation used to record information about encounters with patients. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. We will break down each component of a soap note and explain how to write a soap note. . Soap Note Example Np.
From www.sampletemplates.com
FREE 9+ Sample SOAP Note Templates in PDF MS Word Soap Note Example Np save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. Subjective, objective, assessment, and plan. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. there are four basic components of a soap. Soap Note Example Np.
From www.studocu.com
NGR6201L Focused SOAP Note Hypertension Focused SOAP Template Student Soap Note Example Np — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. A soap note is standard across all types of chart notes and can be used in. Soap Note Example Np.
From npchartingschool.com
Examples of a SOAP note plus 7 tips for charting! Soap Note Example Np Subjective, objective, assessment, and plan. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap nursing notes are a type of patient progress note or nurse’s note. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. Soap Note Example Np.
From www.studocu.com
SOAP Note 2 Graded.docx Sample SOAP Note 2 Graded NURS 6210 July 12 Soap Note Example Np save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. We will break down each component of a soap note and explain how to write a soap note. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. Soap Note Example Np.
From www.pinterest.com
Soap Note Template Nurse Practitioner New Planning Patient Care Notes Soap Note Example Np A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment, and plan. there are four basic components of a soap note: It is the documentation used to record information about encounters with patients. soap notes are essential for effective patient care and documentation in nurse. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np soap notes are essential for effective patient care and documentation in nurse practitioner practice. We will break down each component of a soap note and explain how to write a soap note. soap nursing notes are a type of patient progress note or nurse’s note. there are four basic components of a soap note: A soap note. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Soap Note Example Np soap nursing notes are a type of patient progress note or nurse’s note. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. It is the documentation used to record information about encounters with patients. A soap note is standard across all types of chart notes and. Soap Note Example Np.
From mavink.com
Ems Soap Note Template Soap Note Example Np save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. there are four basic components of a soap note: soap nursing notes are a type of patient progress note or nurse’s note. soap notes are essential for effective patient care and documentation in. Soap Note Example Np.
From studylib.net
Patient SOAP Note Charting Procedures Soap Note Example Np soap nursing notes are a type of patient progress note or nurse’s note. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. Subjective, objective, assessment, and plan. It is the documentation used to record information about encounters with patients. there are four basic components of. Soap Note Example Np.
From www.studocu.com
Episodic SOAP Note Template Rx1 EPISODIC SOAP Note Template Student Soap Note Example Np — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. there are four basic components of a soap note: soap notes are essential for effective patient care and documentation in nurse practitioner practice. It is the documentation used to record information about encounters with patients. Subjective, objective, assessment,. Soap Note Example Np.
From www.carepatron.com
SOAP Notes for Nursing Template & Example Free PDF Download Soap Note Example Np — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap notes are essential for effective patient care and documentation in nurse practitioner practice. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Subjective, objective, assessment,. Soap Note Example Np.
From www.sampletemplates.com
16+ Sample SOAP Note Examples PDF, Word Sample Templates Soap Note Example Np save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. It is the documentation used to record information about encounters with patients. — if you’re a nurse practitioner, then you know that writing soap notes is a vital part of documenting patient care. soap. Soap Note Example Np.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners Etsy Soap Note Example Np — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. We will break down each component of a soap note and explain how to write a soap note. soap nursing notes are a type of patient progress note or nurse’s note. It is the documentation used to record information. Soap Note Example Np.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Np It is the documentation used to record information about encounters with patients. save time with this downloadable soap notes template for nursing, which is guaranteed to elevate the accuracy and quality of your clinical documentation. A soap note is standard across all types of chart notes and can be used in any area of healthcare. soap nursing notes. Soap Note Example Np.